Facial volume loss is an important component of facial aging and tends to present at an earlier age than other aspects of aging. Several surgical and nonsurgical products and techniques are available to replace volume loss associated with aging. One surgical technique uses a patient’s fat cells to replace or augment volume deficiency. Poly-L–lactic acid (PLLA) injection is a nonsurgical option. This article compares these 2 volume augmentation procedures and discusses characteristics of facial aging, the consultation process involved in assessing individual volume loss, procedure details of autologous fat grafting and PLLA injection, the decision of PLLA versus autologous fat, and patient outcomes.
Key points
- •
Facial volume loss, both from bone loss and soft tissue loss, contributes significantly to facial aging.
- •
Understanding the changes that occur and striving to restore patients to their youthful state rather than removing and lifting tissue in isolation is paramount.
- •
A multitude of treatment options has been introduced in the past decade to restore lost volume.
- •
Great advances in understanding youthful contours, both on the surface and in the facial fat pads, have occurred and continue to advance.
- •
Both poly-L–lactic acid (PLLA) and autologous fat transfer offer improvement in the treatment of facial volume loss. Using each procedure appropriately to bring the greatest degree of satisfaction to patients remains the goal.
Introduction
Facial volume loss has increasingly been recognized as a significant contribution to the facial aging process. Changes in facial volume usually present beginning in a patient’s third decade and continue for the ensuing years. The extent and rapidity of facial aging vary between individuals and are strongly dependent on patient bony facial structure, soft tissue adipose content, and skin quality. Studies have analyzed the varying contributions of bone loss versus soft tissue loss in creating this aged appearance with interesting findings.
Restoration of lost volume may be performed by using syringe-based filling agents, such as hyaluronic acid, calcium hydroxyapatite, PLLA, and polymethyl methacrylate; a patient’s own adipocytes through autologous fat transfer; or surgically placed synthetic implants. Each of these methods may lead to acceptable or even exceptional results in the appropriate hands. This article compares 2 of these techniques: autologous fat transfer and injection of PLLA.
Introduction
Facial volume loss has increasingly been recognized as a significant contribution to the facial aging process. Changes in facial volume usually present beginning in a patient’s third decade and continue for the ensuing years. The extent and rapidity of facial aging vary between individuals and are strongly dependent on patient bony facial structure, soft tissue adipose content, and skin quality. Studies have analyzed the varying contributions of bone loss versus soft tissue loss in creating this aged appearance with interesting findings.
Restoration of lost volume may be performed by using syringe-based filling agents, such as hyaluronic acid, calcium hydroxyapatite, PLLA, and polymethyl methacrylate; a patient’s own adipocytes through autologous fat transfer; or surgically placed synthetic implants. Each of these methods may lead to acceptable or even exceptional results in the appropriate hands. This article compares 2 of these techniques: autologous fat transfer and injection of PLLA.
Facial volume loss: youth versus age
Periorbital
The youthful upper periorbital complex consists of a brow that is full over its entire height, propped up by the volume of the brow fat pad. Entire articles have been written and rewritten about the normal aesthetic height of the brow. Often, however, brow shape and configuration are more important than brow height and perhaps lifting is not the solution to the aging brow in all cases. Comparing photos in the latest fashion magazine shows many examples of models, all of whom are exquisitely attractive, with significantly differing relationships between the brow and superior orbital rim ( Fig. 1 ). The upper eyelid also shows a variable fullness between patients; all may be considered youthful and attractive. Some youthful individuals have significant tarsal show with a deep superior orbital sulcus, a high lid crease, and little dermatochalasia. Others have little tarsal show with a more prominent orbital fat component and, therefore, a much fuller-appearing upper eyelid. In the author’s opinion, the restoration of the youthful upper eyelid and brow complex must be tailored to a patient’s unique characteristics and must strive toward the restoration of youthfulness and not an ideal appearance based on the biases of a surgeon. Additionally, the forehead, temporal fossa, and glabellar area should all be convex and full and free of rhytids in the youthful face.

Infraorbital
The youthful lower eyelid complex consists of a short lower eyelid or, rather, a superiorly placed and full upper cheek. The lower eyelid cheek interface should be at the lower tarsal border and flow into a full convex upper anterior cheek. This natural convex fullness results from the quantity of the lower eyelid suborbicularis oculi fat, superficial fat, and inferior orbital rim projection ( Fig. 2 ). The infraorbital area ages prematurely when a negative vector configuration of the midface is present, much as the jaw line and neck age earlier in people with microgenia and a short thyromental distance ( Fig. 3 ). The youthful lower eyelid must also lack pseudoherniation of orbital fat. The cheek skin should be smooth over the underlying fat and the malar cheek fat pad should be shaped as a teardrop, with the rounded leading edge of the tear inferior-medial and tapering laterally over the anterior aspect of the zygomatic arch. The inferior aspect of this teardrop should create a subtle shadow in its interface with the buccal region that parallels that of the jaw line ( Fig. 4 ).


Perioral
Inferior to the cheek fullness, the perioral region should be generally full with a soft transition from the anterior cheek fullness across the melolabial fold and into the cutaneous upper lip; however, presence of a melolabial fold is not necessarily a sign of aging and may be prominent in youth, especially when associated with a full round face. Both the white cutaneous and red mucosal lips are full with associated natural peaks and valleys. The corners of the mouth are neutral or slightly up-turned and there is no marionette line formation.
Jaw and Neck
The jawline should be full and has more vertical height in youth without interruption from jowl formation. The angle of the jaw should have good lateral projection with a well-defined angle that approximates 90° as it ascends to the ramus.
Multifactorial Process of Aging
Aging is the culmination of a multifactorial process that includes the actions of gravity, volume loss, and skin changes due to intrinsic and extrinsic factors.
Periorbital aging
Volume loss in the upper periorbital area leads to exposure of harsh bony contours and the creation of shadows and concavities associated with aging. In the superior rim, this also leads to an apparent descent of the brow. As volume is lost over the bony orbital rim, the support for the soft tissue brow is lost. This effectively raises the position of the bony rim, which is now harsh and skeletonized, and leads visually to a drop in brow height. Illusions of the ratio of the pretarsal skin to lash line and brow also disrupt the normal ratios and offer an appearance of age. Lastly, volume loss in the temporal fossa and forehead contribute, and restoring this area to a youthful convex configuration assists in upper facial rejuventation.
Lower periorbital/cheek aging
Lower periorbital/cheek aging is perhaps most significantly influenced by volume-related changes and responds well to volume replacement. With time, the heart-shaped youthful face gives way to the more rectangular face of age as the loss of fullness in the lower eyelid and cheek region is combined with the increased width of the jawline at the jowl. Additionally, cheek volume loss creates the appearance of shadows as depleted superficial tissues fall and become tethered by various retaining ligaments. Shadows and contour disruptions arise in the lower eyelid and cheek between the orbital fat and the orbital bone. The lower eyelid gains apparent length in this process. Below this, the malar mound and malar septum create a second double contour in the cheek region ( Fig. 5 ). Restoration of youth combines removal of orbital fat pseudoherniation, if present, and placement of volume into the orbital groove/tear trough and cheek region to restore the single convexity of the cheek and raise the cheek eyelid junction, thereby shortening the apparent lower lid height.

Perioral aging
Perioral aging results in deepened nasolabial folds and loss of fullness of the white cutaneous and red mucosal lip, with resultant radial lip lines as well as marionette line formation. Loss of premaxillary volume, through bony changes primarily, causes the nose to become ptotic and the nasolabial angle to deepen.
Jawline aging
Age-related volume loss also occurs along the lower third of the face with recession of the jawline. Comparison of youthful and aged photos of patients often shows the significant mandibular vertical loss and the appearance of jowling may be as much a result of this change as descent of the jowl fat. Restoration of the jawline is usually accomplished with a combination of surgical lifting and the prejowl, chin, and mandibular angle as indicated.
Patient consultation
A consultation begins by listening. Patients are asked to express their age-related concerns. In the past, patients rarely mentioned that their face had become hollow or that they had a tear trough deformity. More recently, however, patients have become savvier about the contribution of volume loss and often present inquiring directly about its replacement.
Brow Assessment
Assessment begins with analysis of hair-bearing brow height in relation to the orbital rim. More often, the brow is at a reasonable height and the primary factor is loss of the brow fat pad volume and associated volume loss of the temporal fossa, forehead, and glabella. It is only in 10% to 15% of patients that surgical brow lifting seems indicated, in the author’s practice. If available, a comparison of patients’ youthful photographs assists in the discussion of volume loss and brow position. Often, the indication for brow lift is more related to lateral brow ptosis, creating a flat brow configuration and associated melancholy appearance.
Lower Eyelid and Cheek Assessment
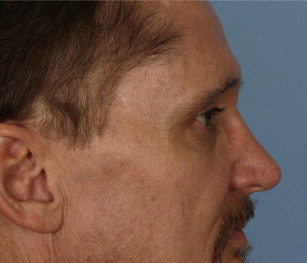
Assessment shifts inferiorly to the lower eyelid and cheek region. First, the presence of lower eyelid steatoblepharon must be determined. An assessment is made on lateral view whether or not any pseudoherniation projects anterior to an ideal convex line to be created at the lower eyelid cheek junction ( Fig. 6 ). This is a judgment that improves with practice, but, especially for less experienced surgeons, if the decision is questionable, fat removal is recommended. If orbital fat reduction is indicated, it is performed conservatively, taking care to minimize the inferior extent of the submuscular dissection to allow an undisturbed tissue plane for placement of autologous fat both in the preperiosteal and submuscular/intramuscular planes. Anterior and lateral cheek volume loss is nearly always present to some degree.
If present, festooning should always be discussed. This is a difficult deformity to correct. In its early stages, filling around the malar mound provides improvement, but if a true edematous festoon is present, the fluctuations in swelling may be exacerbated by filling and may take weeks or months to resolve post-treatment, especially with fat transfer. Treatment of this condition is surgical and beyond the scope of this discussion.
Perioral Assessment
Perioral volume loss should be noted, but neither PLLA nor autologous fat is an ideal volume replacement choice for this area. Although the author always places fat in the perioral region with full face fat transfer, and fat may be placed essentially anywhere in the face safely, patients are warned that fat grafting rarely persists long term in the perioral region. It is postulated, much like skin grafting, that the constant movement of the perioral musculature and the lack of a stable bony platform to place the fat lead to shearing of the vascular ingrowth and eventual graft failure. PLLA has limitations in the perioral area as well. Although it is safe to place PLLA in the cutaneous portions of the perioral unit, placement in the mucosal lip or too near the modiolus is ill advised because of development of palpable nodules.
Jowl Assessment
Assessment of the lower face related to volume involves assessing for the presence of a prejowl deficiency, microgenia, and/or mandibular angle deficiency. As discussed previously, the jowl descent is improved with lifting procedures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




