This article presents a comprehensive clinical approach to plasma resurfacing for skin regeneration. Plasma technology, preoperative protocols, resurfacing technique, postoperative care, clinical outcomes, evidence-based results, and appropriate candidates for this procedure are discussed. Specific penetration depth and specific laser energy measurements are provided. Nitrogen plasma skin regeneration is a skin-resurfacing technique that offers excellent improvement of mild to moderate skin wrinkles and overall skin rejuvenation. It also provides excellent improvement in uniformity of skin color and texture in patients with hyperpigmentation with Fitzpatrick skin types 1 through 4.
Perspectives on skin resurfacing
The most common objectives of a facial resurfacing technique are to remove wrinkles or scars and rejuvenate skin. Rejuvenation may include improvements in texture and uniformity in color. The various machines and techniques accomplish their results with varying depths of epidermal and dermal penetration, and stimulation of neocollagenesis. Before the introduction of aesthetic uses for the carbon dioxide laser in the mid-1990s, mechanical dermabrasion with a diamond fraise or wire brush and various chemical peels were the predominant treatments. Mechanical dermabrasion is less prevalent today. Medium-depth and deep chemical peels are still performed successfully by many medical practitioners, and superficial peels are now commonly done in medical and nonmedical spalike settings.
Principles of Lasers
Lasers function according to the principles of photothermolysis. Each laser commonly delivers a light of a pure, single color (wavelength) to the skin. The part of the skin targeted by the laser is related to the color of the laser light and the color of the target (chromophore) in the skin. Each laser wavelength has a complementary color or range of colors that best absorb the wavelength of the light it produces. For the carbon dioxide laser (10,600 nm), for example, the primary target of the laser is water. Because skin cells are mostly water, the laser targets these cells and vaporizes them in a very controlled and precise manner. Some lasers combine more than 1 wavelength to selectively target more than 1 chromophore.
Lasers for Skin Rejuvenation
Common lasers for skin rejuvenation are the 10,600-nm carbon dioxide laser, the 2940-nm erbium:YAG laser, and the fractionated erbium 1550-nm and 1410-nm lasers. The introduction of fractionated technology brought some practical solutions for patients requesting procedures that could be done with shorter postprocedure downtime under local anesthesia. Fractionated technology provides a means of delivering the laser beam in distinct columns of light spaced so as to spare tissue between adjacent targeted areas. This tissue sparing leads to shorter healing times and less tissue ablation. Full ablative laser treatments are also still popular for maximum wrinkle reduction and skin rejuvenation, if a patient will accept a few more days of downtime.
Neocollagenesis
The appropriate technology for a particular patient depends on the depth of the wrinkles or scars to be treated, how much excess pigment, solar elastosis, or other signs of sun damage prevails, how the patient’s skin will react to light and heat, and the amount of downtime the patient will tolerate. While all of the various techniques will mechanically or chemically peel the epidermis, the amount of heat delivered to the skin and the depth of that heat penetration are major determinants of the amount of neocollagenesis that actually tightens the dermis. The depth of penetration for each laser depends on the wavelength of the target chromophore, the number of passes, and the amount of laser energy delivered. Typical depths of penetration are as follows:
| Carbon dioxide | 10,600 nm | 450 μm to 1–2 mm (though rarely beyond 1 mm) |
| Erbium:YAG | 2940 nm | 3–120 μm |
| Erbium fiber, diode pumped | 1550 nm | 250–800 μm |
The Introduction of Plasma Technology
Portrait PSR 3 is a Class II nonlaser device that provides many of the same advantages of a laser as well as reasonably short postprocedure downtime. Introduced into the United States market for cosmetic use by Rhytec, Inc (Waltham, MA, USA) in 2005, it is a machine that produces nitrogen plasma in its hand piece. (Energist Group [Swansea, UK] now owns the manufacturing rights and distribution rights for the device, spare parts, and service.)
Plasma, an ionized gas, is the fourth state of matter. The explosions off the sun’s surface, electrical storms, and the Aurora Borealis all contain plasma. Plasma television sets, though now largely replaced by LCD and LED technology, are commonplace today. Plasma technology is nothing new to medicine. Unlike surgical cautery devices that produce plasma, the Portrait hand piece does not touch the skin. Nitrogen plasma is delivered to the skin in one or more passes in a technique similar to that of laser resurfacing ( Fig. 1 ). An ultrahigh-frequency pulse of radiofrequency energy driven through a tungsten element ignites nitrogen gas flowing through the hand piece. This pulse of energy converts the stable nitrogen gas to unstable, ionized nitrogen plasma (see Fig. 1 ).

Portrait is approved by the Food and Drug Administration (FDA) for treating facial and nonfacial rhytids, acne scars, and superficial benign skin lesions such as seborrheic keratoses, viral papillomata, and actinic keratoses in Fitzpatrick skin types 1 through 4. The author has been using this device since July 2006 and has also successfully treated benign skin lentigines. If there is any question of malignancy, the lesion is biopsied first.
The device is contraindicated for nursing or pregnant mothers and in patients prone to keloid formation. In accordance with the original protocols, all retinols are discontinued for 4 to 6 weeks before the treatment.
Plasma skin regeneration is a resurfacing technique
This technology, though originally labeled plasma skin regeneration (PSR), is truly a skin-resurfacing technique. The heat generated in the dermis is ablative enough to stimulate neocollagenesis. The efficacy of this technology is well established in the literature, and the new collagen produced is essentially vertically oriented, as is normal collagen. Typical penetration is to 500 to 600 μm in normally hydrated skin at energies over 3.0 J. It can be used as a single or multiple treatment modality with well documented neocollagenesis in both modes, significant decreases in facial rhytids, and overall improvement in the general appearance of facial, neck, chest, and dorsal hand skin. Although not as efficacious in treating acne scars as the carbon dioxide laser, it can improve some acne scarring by as much as 34%.
Holcomb and colleagues have demonstrated the safety and enhanced results that are possible when combining facelift and cosmetic eyelid surgery with plasma resurfacing, and also gave very specific recommendations for technique and energy levels to be used.
Plasma skin regeneration is a resurfacing technique
This technology, though originally labeled plasma skin regeneration (PSR), is truly a skin-resurfacing technique. The heat generated in the dermis is ablative enough to stimulate neocollagenesis. The efficacy of this technology is well established in the literature, and the new collagen produced is essentially vertically oriented, as is normal collagen. Typical penetration is to 500 to 600 μm in normally hydrated skin at energies over 3.0 J. It can be used as a single or multiple treatment modality with well documented neocollagenesis in both modes, significant decreases in facial rhytids, and overall improvement in the general appearance of facial, neck, chest, and dorsal hand skin. Although not as efficacious in treating acne scars as the carbon dioxide laser, it can improve some acne scarring by as much as 34%.
Holcomb and colleagues have demonstrated the safety and enhanced results that are possible when combining facelift and cosmetic eyelid surgery with plasma resurfacing, and also gave very specific recommendations for technique and energy levels to be used.
Our protocol for plasma skin resurfacing
Skin Preparation
Before recommending any resurfacing technique, a thorough family and personal history are important. Specifically, it is important to determine the patient’s propensity for postinflammatory hyperpigmentation. In New England, we (the author’s group) see many patients who appear to have Fitzpatrick type-3 skin with a significant propensity for hyperpigmentation. European lineage mixed with Native American lineage and French Canadian lineage mixed with Native American lineage are commonplace in our population. After taking a careful history of the patient’s sun exposure habits and how the patient’s skin has reacted to severe sun exposure in the past, we often treat these patients as we would patients with Fitzpatrick type-4 skin (see Operative Technique). All patients are pretreated with 4% hydroquinone for 4 to 6 weeks before the treatment. Hydroquinone is restarted 7 to 10 days after the treatment. Retinols are discontinued 6 weeks before treatment. We routinely pretreat our patients scheduled for carbon dioxide laser resurfacing with retinol and hydroquinone, and our plasma-resurfacing patients with just hydroquinone. To the author’s knowledge, no studies have been done using preoperative retinols for patients being treated with nitrogen plasma. After the procedure we usually wait 30 days before restarting retinols in both groups.
Infection Prophylaxis
All patients receiving perioral treatments are started on valacylovir, 1 g daily for 7 days starting on the day of treatment for herpes simplex prophylaxis. All patients are placed on bacterial prophylaxis for 7 days starting on the day of treatment. Most patients receive cephalexin. Penicillin-allergic patients are given clindamycin or doxycycline.
Operative Technique
The delivery system consists of a tube that delivers nitrogen gas to a disposable hand piece that ignites the nitrogen gas, converting it to plasma just before it is delivered to the skin. The ignition takes place by vibrating a tungsten filament at an ultrahigh radiofrequency. An electronic key that controls hand-piece function is programmed for a limited number of treatments per hand piece. The FDA required this feature at the time of approval.
Sedation
Most of our patients are treated in our office under topical or topical plus subcutaneous local anesthesia. We have a Level 1 treatment facility, so we do not use any intravenous sedation. Patients who request sedation or general anesthesia have their procedures in the day-surgery unit of our hospital. Our office is located in the same building.
Skin preparation
- •
The original studies were done after hydrating the skin for 1 hour before the treatment. For this we use a topical anesthetic cream of benzocaine, tetracaine, and lidocaine compounded at a local compounding pharmacy, or commercially available 4% lidocaine cream.
- •
If the patient is under general anesthesia (eg, at the time of a facelift), the skin is hydrated with a petroleum ointment (Aquaphor).
- •
If treating without this period of hydration, the fluences are decreased about 30%.
- •
In the office, patients are given 5 to 10 mg of diazepam by mouth at the beginning of the 1-hour hydration period and 5 mg of oxycodone or a combination tablet of oxycodone, 5 mg and acetaminophen, 325 mg by mouth 15 minutes later.
- •
Topical anesthetic alone is usually sufficient for patients having treatments below 2 J (PSR 1; see later discussion).
- •
For higher-energy treatments (PSR 2 and PSR 2/3; see later discussion), regional blocks and direct infiltration are done with a total of 15 to 20 mL of 0.5% lidocaine, 1:200,000 epinephrine 10 minutes before the procedure. All 3 branches of the trigeminal nerve are blocked.
- •
Infiltration is also done directly along the superior edge of the entire length of the brow, the entire lower eyelid, the temple just anterior to the temple tuft of hair, and an area along the jaw line and lateral cheek about 1.5 cm wide beginning just anterior to the sideburn and extending to the marionette crease.
- •
An upper dental block is placed intraorally, after applying a topical oral anesthetic gel (Hurricaine).
- •
The most tender areas of the treatment are the temples, lateral cheeks, jaw line, upper hairline, and upper lip.
- •
Just before the treatment, we remove the topical anesthetic cream with a moist sponge and draw a grid on the skin with a temporary marker to help ensure that the energy is delivered uniformly ( Fig. 2 ). Because this treatment is not chromophore dependent, the marker can be any color.
Fig. 2
Topical anesthetic cream and grid to guide the treatment.
( Courtesy of Energist Group, Nyack, NY & Swansea, Wales, UK; with permission.)
Skin care during treatment
- •
An important feature of this treatment is that the epidermis is purposely and carefully left intact. The intact epidermis acts as a biological dressing.
- •
During a treatment above 2 J per pulse, we frequently apply an ice pack to the first side of the face treated while treating the opposite side. A cooling device that blows cool air will also work well. The immediate cooling should not adversely affect the efficacy of the treatment.
Skin care after treatment
- •
We apply a petroleum-based ointment (Aquaphor) immediately after the treatment along with a cool gel mask. The petroleum ointment acts as a heat sink by itself, and the gel mask seems to facilitate the process.
- •
The skin is protected from the mask by soft gauze. The mask is left in place until it is again room temperature, after about 30 minutes.
- •
Our music or the patient’s own music also helps with pain control at this point.
- •
The petroleum ointment is reapplied and the patient is discharged. Most patients report that the only pain is like intense sunburn, which is largely gone within 1 to 4 hours.
Posttreatment pain relief
- •
Some patients take oxycodone the evening of the procedure and some just acetaminophen, 650 to 1000 g. Usually no pain medication is needed after the first day. If a patient complains of significant pain the next day, we observe them more closely for a herpes simplex infection. Postoperatively this procedure should not be very painful.
Treatment protocols
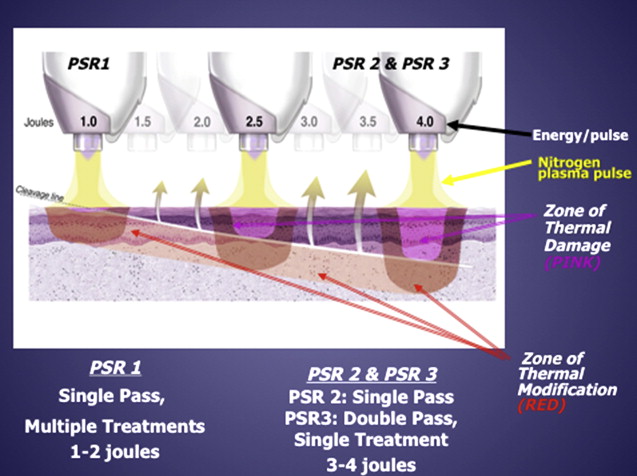
There is a specific nomenclature for the various treatment protocols ( Fig. 3 ):
- •
PSR 1: 1 to 2 J per pulse in a single pass
- •
PSR 2: 2 to 4 J per pulse in a single pass
- •
PSR 3: 2 to 4 J per pulse in a double pass
- •
PSR 2/3: PSR 2 and PSR 3 to different parts of the face.