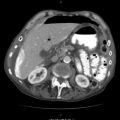
Fig. 35.1
(a) We repair the oesophagus in one layer of Vicryl 1 intermitted horizontal mattress sutures. (b) Then we reinforce our suture line by putting a 2.0 interrupted Vicryl stitch in the space between two consecutive horizontal mattress sutures and then cut all the stitch ends
Do a barium swallow at the seventh day after the repair. If there is a small leak that presents itself as a small sinus, we ignore it and start the patient on liquid diet after another 7 days.
If the gap is too large to approximate the edges of the damaged oesophagus and/or the patient is physiologically unstable, proceed to a bailout solution by proximal drainage of the oesophagus via a NG tube and insertion of an intercostal drain or T-tube (22–24 French) to convert the free perforation into a controlled fistula. This can also apply in situations when the injury is older than 24 h and the repair precarious or the surgeon not experienced with tackling an injury in this anatomical area. After the bailout, a different procedure can be considered if appropriate. Very large defects may require the use of tracheal T-tube with a chest tube intussuscepted over the end of the T-tube. If possible, approximate the edges of the hole around the drain. Drain the pleural cavities with separate tubes. Obtain an oesophagogram after 10 days if there is no clinical leakage; if not, start the patient on liquid diet and then full diet and remove the T-tube after 5–6 weeks by oesophagoscopy to avoid widening of the tract.
When the injury is present for more than 24 h, there is significant infection present that together with the swelling of the oesophageal tissue makes primary repair precarious. There is a variety of methods described for tackling this difficult problem; none of them are complication-free. If it is possible to repair the defect, attempt doing it. As far as we are concerned, this should be the one case where your repair should always be done with interrupted sutures and not continuous, as failure of the suture line is a real threat with stitches cutting through the tissues. The chances of complete opening of the repair in the presence of continuous stitch is higher than if you use interrupted, as hopefully some of them will stay intact and, therefore, keep the defect smaller than the original one. It is wise to buttress the repair. We prefer to mobilise the pleura, which due to inflammation is thickened, and wrap it ‘tightly’ around the repair in immediate contact with the oesophagus but not very ‘tight’ so that it becomes obstructed (Fig. 35.2a, b). This should be about 5 cm long. Books describe wrapping (buttressing) with pericardium, but in our experience, it does contribute to acceptable outcomes. We avoid it as in case of failure of the oesophageal repair, the infection can spread into the pericardial sac. If the oesophageal injury is just above the hiatus, create a diaphragmatic flap and oversew it on the oesophagus, covering the suture line. The base of this flap should start 2 cm from the periphery of the hiatus and extend radially to about 6 cm or even longer if more length is needed to reach the defect site. Rotate the flap upwards from its base, towards the oesophagus, cover the repair or gap, and close the diaphragmatic defect by interrupted sutures (Fig. 35.3a, b). There are cases that none of the repair methods nor are the attempts of forming a controlled fistula likely to be successful. In these cases, it is worth considering isolating the injured area. Distal exclusion of the oesophagus has been practised on the basis that it controls the gastric secretions from being refluxed to the area of the injury. We avoid stapling the distal oesophagus in the chest. We prefer to staple the oesophagus intra-abdominally close to the gastro-oesophageal junction. Mobilise the abdominal oesophagus via an upper abdominal incision exactly the same way as you mobilise for truncal vagotomy. Apply and fire the TA stapler at the gastro-oesophageal junction making sure that you do not include the vagi. Fashion a gastrostomy or probably a jejunostomy. In most cases, this staple line will open by itself as is the case with pyloric exclusion. If this is not the case and the oesophagus has healed, the staple line can be resected, and the oesophagus can be reimplanted at the anterior aspect of the fundus of the stomach.