Fig. 32.1
Anatomic landmarks of the pharyngoesophageal region
The pharynx and cervical esophagus lie deep in the neck and are protected posteriorly by the cervical vertebrae. They are abutted anteriorly by the larynx and trachea. Consequently, the only way to get to the pharyngoesophageal region is via a lateral approach which requires retracting the carotid sheath out of the way. Concomitant (and more deadly) injury to the trachea or vascular structures should be addressed before embarking on a pharyngoesophageal repair.
32.2 Know When to Go In
There are essentially two scenarios in penetrating neck trauma. The first scenario is a patient with an obvious “hard sign” (expanding hematoma, active bleeding, shock, airway compromise, massive subcutaneous emphysema) of vascular or tracheal injury who needs to be in the operating room immediately. Once these injuries are identified and repaired, the pharyngoesophagus should be evaluated. Trace the trajectory of the bullet. Perform maneuvers to see if there is a hole in the esophagus (on table endoscopy, air in the nasogastric tube, etc.), and repair it. If the patient is too unstable for further exploration, then leave a drain and get out.
The second, more common scenario is a patient who is hemodynamically stable and requires evaluation to exclude an injury that should be fixed in the operating room expeditiously. Several retrospective studies found worse esophageal-specific outcomes in patients who had a preoperative evaluation prior to the esophageal repair compared with those who did not. The implication is that delay in repair (while studies are being performed) leads to a worse outcome. The retrospective nature of these studies makes the interpretation difficult, and no specific time frame has been established, but the take-home message is to identify and treat esophageal injury as soon as possible.
There are no hard signs of pharyngoesophageal injury, but a thorough history and physical examination may give clues that further workup is needed. Symptoms of odynophagia or dysphagia and signs of subcutaneous emphysema or hematemesis are indications of pharyngoesophageal injury and warrant further evaluation. In a study of 223 patients with penetrating neck injury, none of the evaluable, asymptomatic patients had an esophageal injury; workup was recommended for symptomatic or unevaluable patients. Similarly, a larger multicenter study of 453 patients with penetrating neck wounds noted no missed injuries in the group of asymptomatic patients. Still, the potential morbidity associated with a missed injury has led to the recommendation that surgeons have a low threshold for obtaining imaging studies in evaluating penetrating injuries to the neck.
Computed tomography angiography (CTA) has emerged as the single imaging modality with the greatest potential to rule out esophageal as well as tracheal and vascular injuries. A missile trajectory away from the esophagus (or other vital structures) obviates the need for exploration or additional invasive studies. Beyond this, CTA has not yet proven itself as a stand-alone study for diagnosing or excluding pharyngoesophageal injury. In 2003, Gonzales evaluated 42 patients with CTA followed by mandatory esophagogram and operative exploration. Two very small stab wound injuries (<5 mm) were missed both by CTA and swallow study, suggesting that CTA was no better than esophagogram. Inaba subsequently found that CTA “overdiagnosed” aerodigestive injury in four patients with subcutaneous air as the common, nonspecific sign. Two patients had the injuries ruled out by negative contrast swallows and endoscopy. The other two patients underwent negative exploration. Most centers are using physical examination along with CTA to evaluate for a possible aerodigestive injury. Finding air near the pharyngoesophagus prompts the need for further study, surgical exploration, or both (Fig. 32.2).
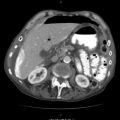
Fig. 32.2
Nondiagnostic CTA images for exclusion of pharyngoesophageal injury. Air near the pharynx and esophagus will require further evaluation if there are no other indications for surgical exploration
Current recommended workup of pharyngoesophageal injury is by contrast esophagography or esophagoscopy. There is no consensus that one study is preferable to the other, and most study protocols seem driven by surgeon preference or institutional availability. If a contrast swallow study is chosen, a majority of authors favor water-soluble esophagogram initially, with thin barium to follow. The sensitivity of esophagography to detect pharyngoesophageal injury varies widely and is reported between 60 and 100 %. Rigid or flexible endoscopy has proven equally, if not more efficacious to esophagogram. Two early studies utilizing rigid esophagoscopy suggested improved sensitivity compared with esophagogram. Since then, flexible endoscopy has been studied with a reported 100 % sensitivity (92 % and 95 % specificity). As flexible endoscopy does not require general anesthesia or manipulation of the cervical spine, it is the scoping modality that we prefer.
Of importance, multiple authors report successful conservative (nonoperative) management of patients with penetrating pharyngoesophageal injury. In these studies, patients are kept nothing per oral (NPO), given intravenous antibiotics, and maintained on surgical nutrition (enteral or parenteral). Stanley made a compelling argument that penetrating injuries of the upper hypopharynx (above the arytenoids) be managed nonoperatively. He suggested that the anatomy of this area favored spontaneous healing yet further demonstrated increased complications to the lower pharynx or cervical esophagus if these areas were not surgically repaired. Nel and Yugeros also reported retrospective success of nonoperative management of the pharynx (but did not specify upper or lower). Madiba successfully managed patients with penetrating injury to the cervical esophagus nonoperatively if their water-soluble contrast study showed contained extravasation (not trickling widely or into the mediastinum). To date, there are no prospective, randomized studies comparing the role of surgical and nonoperative management for penetrating pharyngoesophageal injury. Based on retrospective data, a nonoperative approach seems feasible in a patient with a contained pharyngeal injury who has no other indications for neck exploration.
To summarize, we recommend physical examination and CTA in stable patients with penetrating injuries to the neck. If the examination is negative and the trajectory of the injury is away from the pharyngoesophageal area, no further workup is performed. If there is still potential for pharyngoesophageal injury, we recommend expeditious esophagogram. A small, contained pharyngeal leak can be managed nonoperatively, with plans to repeat the swallow study in 3–5 days. A patient with a larger, noncontained injury should be taken immediately to the operating room for primary repair. Flexible endoscopy is our preferred modality in a patient who needs to go or is already in the operating room, who is intubated (making the logistics of a swallow evaluation difficult) or whose swallow evaluation is “negative,” but whose physical examination or CTA is highly suggestive of a pharyngoesophageal injury.
32.3 How to Do the Repair
So you’ve made the decision to operate. Positioning the patient for a complete neck exploration is the first key to success. Place a shoulder roll and tilt the patient’s head away from the injury – unless of course, there is concern of a cervical spine injury, in which case you will have to keep the head midline. Start your neck exploration on the side that is injured. If the injury is bilateral or you are not sure where the injury originates, start your approach to the esophagus from the patient’s left side. The esophagus deviates slightly to the left in the neck, and there is a lesser chance of injury to the recurrent laryngeal nerve on this side.
Have the anesthesiologist gently place a nasogastric (NG) tube. The NG tube often proves critical in finding your injury when the time comes. Prep and drape both sides of the neck (from the mastoid down), and include the entire chest in the event that mediastinal exploration is warranted. It is also prudent to prepare both groins in case vascular access or saphenous vein harvesting is required.
Start with a generous incision along the anterior border of the sternocleidomastoid (SCM) muscle (Fig. 32.3). If better exposure is required, the incision can be extended all the way up to the mastoid superiorly. Curve posteriorly as you approach the angle of the mandible to avoid injuring the marginal mandibular branch of the facial nerve and the complication of smiling asymmetry. Inferiorly, the incision can be carried down to the sternal notch (and even further if median sternotomy is needed).
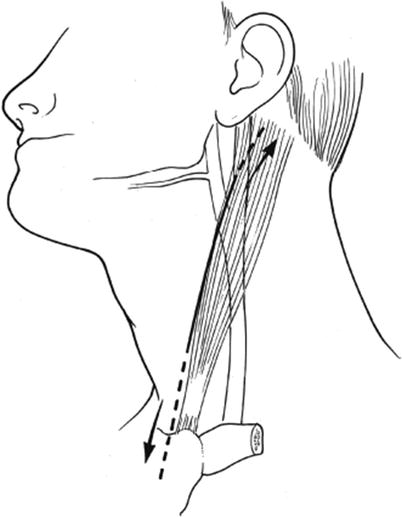
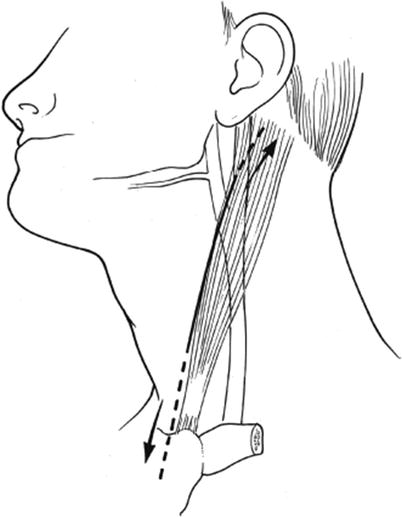
Fig. 32.3
Incision along the anterior border of the sternocleidomastoid muscle
Divide the platysma muscle and look for the SCM. The critical next move is dividing the fibrous tissue (superficial cervical fascia) along the anterior border of the SCM (Fig. 32.4). Use a retractor to pull the SCM laterally so you can fully extend the exposure in either direction. This gives you direct access to the carotid sheath.
Fig. 32.4
Approach to the cervical esophagus
Put in self-retaining retractors, such as blunt-tip Weitlaners, now. Make sure that the Weitlaner retractors prongs sit below the SCM.
You are about to begin your search for the pharyngoesophagus. In order to get to the esophagus, visualize the mantra – “carotid sheath down and thyroid gland up.” That is the path you must create to get to your injury. To safely and effectively perform this retraction, you will need to open the carotid sheath and ligate some key structures. Tackle any encountered vascular injuries first.
Open the carotid sheath laterally over the big blue internal jugular vein (Fig. 32.5). Stay on the anterior surface of the vein, and extend in both directions. As you move superiorly, look for the large facial vein which courses just over the carotid bifurcation. The facial vein is a critical landmark in any neck exploration; once identified, it needs to be ligated and divided. This provides direct access to the carotid bifurcation and also releases the internal jugular for lateral retraction. With the facial vein ligated, you may replace your blunt Weitlaner retractors below the medial aspect of the internal jugular to increase exposure.
Fig. 32.5
Open the carotid sheath over the internal jugular vein and identify the facial vein
Begin to march from superior to inferior along the internal jugular vein to release the thyroid gland and retract it “up” (anteromedially), so you can access the pharyngoesophagus. In your approach, you will sequentially encounter and divide three structures – the middle thyroid vein, the inferior thyroid artery, and the omohyoid muscle (Fig. 32.6). The middle thyroid vein comes directly off the internal jugular and goes into the thyroid gland. Once this is divided, the thyroid gland can be pulled more medially. Next, gently retract the carotid sheath “down” (posterolaterally), and you will see the inferior thyroid artery, a branch of the thyrocervical trunk (from the subclavian artery), coursing horizontally posterior to the carotid and entering the posterolateral aspect of the thyroid. Divide this. Note: The inferior thyroid artery is another crucial landmark as it leads you directly to the recurrent laryngeal nerve. Use this opportunity to look for the nerve in the tracheoesophageal groove, and avoid it. Finally, carry on inferiorly and divide the superior belly of the omohyoid muscle. You now have maximal exposure to the pharyngoesophagus and are ready to go.