Fig. 38.1
Cardiac repair via a clamshell thoracotomy incision. The proximal part of the severed left mammary artery is identified and ligated
In situations that the patient is not in extremis (and you have time to transfer him from the resuscitation area to theater), it is preferable to get access to the heart by performing a median sternotomy – never forgetting to place a sandbag between the scapulae. This is the ideal incision not only for repairing the heart but also the ascending aorta (one of the rare causes of cardiac tamponade) and the arch of the aorta with its proximal branches. The most common pitfall of this incision is to miss the midline on splitting the sternum. Make the skin incision first and use the diathermy to extend the incision deep to the anterior aspect of the sternum from sternal notch to xiphoid, marking the midline of the sternum with the diathermy. Then divide the intraclavicular ligament so that you create a small retrosternal space at the proximal part of the manubrium either using a diathermy or a right-angled Lahey. When you do this procedure or the lower down description of splitting the sternum, you should place yourself at the left of the patient if you are right-handed and on the right if you are left-handed. You will find that the intraclavicular ligament is very tough, and for most of us, it is quite difficult to perforate with the tip of a closed right-angled Lahey when we are using one hand. Grab the right-angled Lahey with your two hands: the right hand (if you are right-handed) on the vertical part quite close to the tip and the left hand grabbing the handle. Position the tip of the right-angled Lahey just posteriorly to the sternal notch and push the tip at the retromanubrial space with a rotational movement, the force of the movement applied by your right hand. There is a characteristic giving way and noise as the tip of your clamp goes through the tough ligament. As it is difficult to perforate the ligament, it is also difficult then to open the limbs of your right-angled Lahey so that you create the space for the introduction of the pneumatic saw or the tip of the Libscher knife. Hold the two arms of your clamp separately (one arm in each hand) and then open the clamp. This maneuver can sometimes lead to alarming bleeding from the area that is difficult to control due to its limited access. Do not panic! There is always a worry that you have injured a large vessel; remember that the only large vessel in this area is the innominate vein which in any case lies too deep to be injured with this maneuver.
If rapid opening of the sternum is of paramount importance and the bleeding from this area is too much, pack the area, apply some pressure, and perform a medial sternotomy by starting from the xiphisternum upward. If this option is chosen, be very careful as the caudal part of the sternum is thinner, and therefore as you put force on splitting it, it is quite easy to miss the midline and start dividing the intercostals cartilages. In any case, irrespective of from which direction you open the sternum, make sure that you do not miss the midline.
Open the sternum along the diathermy line using a pneumatic saw or a Libscher knife and hammer following religiously the diathermy line, making sure that you apply only the necessary force to split the sternum. If you apply more force than necessary, you may feel a sudden giving way of the resistance of the sternum resulting in the loss of the midline. If you use the Libscher knife and hammer on opening the sternum from a manubrium to xiphoid direction that is the recommended route, make sure that you have placed a sandbag between the shoulder blades of the patient and have his neck extended and his face turned away from you. The hammer should initially hit the Libscher knife at an angle of 30° with the horizontal plane so as to avoid hitting the patient’s jaw (we have seen it happen). After splitting the manubrium, there is enough distance from the jaw so that the sternum is split by hitting the hammer on the knife horizontally. This problem of course does not arise if you use a pneumatic saw, but it is always advisable to have a Libscher knife on standby as it happens sometimes to be let down by “technology” when you most need urgent access to the mediastinum. Your sternal retractor should be placed into the sternotomy including the distal portion of the manubrium, therefore minimizing the risk of fracturing the sternum on rapidly opening the retractor.
On opening with a preoperative diagnosis of penetrating trauma to the heart (which many times is a clinical diagnosis), inspect the pericardium to confirm tamponade, unless there is an obvious source of active bleeding not related to the heart and you misdiagnosed it as cardiac injury. If this is the case, of course you divert your attention to the site of torrential bleeding and you control it. Hemopericardium may be recognized by the presence of a bulging, tense pericardium or sometimes only by the white-bluish color of the underlying clot. A classic mistake is to leave the pericardium unopened due to its normal appearance from the outside. It is amazing how often you can have a pericardial sack containing a significant amount of blood from injury to the heart or intrapericardial mediastinal vessel, which is not visible through the intact pericardium. Take a scalpel and make a small nick in the pericardium if there is a clot underneath or use two mosquitoes to lift the pericardium and then make a nick with the scalpel if you cannot see any blood between the pericardium and the heart. Insert the tip of your scissors inside the hole and open the pericardium in a vertical direction avoiding injury of the phrenic nerve, which should run parallel and to the left of your pericardial incision. The phrenic nerve is significant in size, and it is most unlikely to damage it. On the other hand, if you transect it in the heat of the moment, proceed with your life-saving procedure without too much grief about the nerve. Patients (particularly the young ones as it is in most cases of penetrating cardiac trauma) can have perfectly normal lives with one paralyzed diaphragm. If further access to the heart is required, add a transverse pericardial incision at the caudal end of your vertical incision (an inverted “T”). Start internal cardiac massage if you find the heart in asystole or ventricular fibrillation while inserting some “fast” stitches to close the defect. The pericardial incision should be extensive enough for you to be able to insert not one but both of your hands. Never do intrapericardial massage by using the palm of one hand and compressing the heart against the spine. This traumatizes the heart, and it becomes apparent from the extensive bruising from the heart seen thereafter. The correct way of massaging the heart is to put one palm posterior to it, palm facing upward and fingertips toward the base of the heart, and the other hand palm facing downward on the anterior aspect of the heart. Then start doing cardiac massage by compressing the heart between your two palms maintaining good firm contact between the heart and the palms at all times, minimizing the chance of potential injury from the application of the cardiac massage. In the presence of non-perfusing ventricular arrhythmia, shock the heart with 20 J with one internal paddle behind the heart and the other in the front. If required, repeat the defibrillation by shocking the heart with a maximum of 50 J. Never defibrillate the heart that is at a complete standstill as this will only further damage the myocardium.
When a penetrating injury to the anterior aspect of the heart occurs, the operation is not complete if you do not check for a posterior wall injury – the patient may leave theater only to return because of rebleeding. For checking the posterior aspect of the heart, you must lift the heart out of the pericardial sack, a maneuver for which the anesthetists must be warned of. Insert your whole palm posteriorly to the heart with the tips of your fingers reaching proximally – to the base of the heart. The heart is lifted outside the pericardial sac, with the rotational movement pivoting at the axis of its fibrous base – this way you avoid to kink the cardiac chambers, as the heart is lifted unblock (Fig. 38.2). The heart is always unhappy with this maneuver, so you should repair the posterior injury as quickly as possible as the heart rapidly develops bradycardia that can lead to asystole. As soon as you see bradycardia developing, drop the heart back into the pericardial sac even if you have not yet succeeded to completely repair the posterior injury. The heart is very irritable and may develop a nonresponsive bradycardia even though you replace it to its bed. In this case, it is very useful to pour roughly 40 °C saline on the heart which results in the heart starting to beat normally again, sometimes even developing tachycardia. There are instances that as soon as the surgeon lifts the heart, it responds repeatedly with such an arrhythmia that it does not give him the opportunity to inspect its posterior aspect. In this case partial elevation of the heart by inserting one or gradually two folded abdominal swabs between its posterior aspect and the pericardium gives time to the heart to adapt to elevation.
Fig. 38.2
Lift the heart en bloc to minimize arrhythmias
Lift up the heart again to proceed with the inspection and repair when the rhythm returns to normal. Always remember to make sure that other intrapericardial organs, i.e., inferior vena cava, are intact (Fig. 38.3).
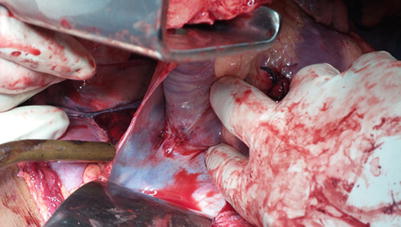
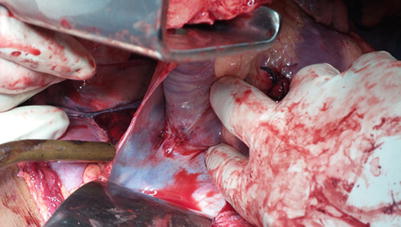
Fig. 38.3
Injury of the heart related with simultaneous injury at the base of the intrapericardial part of the inferior vena cava. Both injuries have been repaired
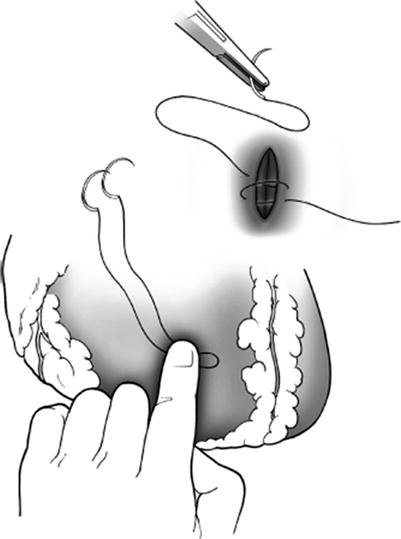
Hold a needle holder in each of your hands, one for inserting the needle in the heart and other for retrieving it. Use a 2.0 silk (when available) and the biggest atraumatic needle you can find when it comes to stitching up the heart. We prefer silk because it is easier for the first knot to hold in the pumping heart, and the last thing you want when you repair hearts is to have loose knots – if silk is not available, use a similar size PDS. While your assistant is controlling the bleeding by applying pressure with a swab on the side of the injury, you position your needle at the needle holder in such a way that the needle holder is very close to the posterior end of the needle. The reason is that in your first through-and-through bite of the heart, you want to insert as much length of needle as possible inside the heart cavity so that you can grab the tip of the needle through the opening of the heart with your needle holder as easily as possible. While inserting your first bite on one side of the defect, there will be a lot of blood spurting out from the heart; keep your cool and insert the tip of your needle holder at the base of the column of the spurting blood and pull your needle out of the defect making sure that your move coincides with the curve of the needle so that you do not slash the myocardium. Reapply your needle on your needle holder while your assistant again controls the bleeding by pressure and insert your needle at the opposite side of the defect. After this bite, things become easier. Hold with your left hand both ends of the stitch and lift them upward. You will see that the two edges of the defect are in this way approximated and you have a spectacular reduction in the amount of blood that is leaking through it. So by holding the initial stitch up, you reapply another stitch so you complete a figure-of-eight stitch (Fig. 38.4). Continue closing the defect by putting more figure-of-eight sutures. It is quite common if your patient is “young at heart” to have a very powerful myocardium that sometimes contracts so forcefully that it kicks away the tip of your needle as you go to insert it inside the myocardium. In this case, hold the handle of your needle holder with both hands and make a fast curved move as you insert the needle inside the myocardium, trying to take advantage of the diastolic period of the heart. It is described in the books that if the defect is not too large, you can insert a Foley catheter and inflate the balloon, therefore controlling the hemorrhage. It does work! Clamp the urine port of the Foley’s and grab the distal 1 cm of the catheter with a clamp and insert it inside the cavity. It is much easier to do that than holding the tip of the catheter with your fingers as you will find that the column of blood escaping from the defect is under a lot of pressure, and it is difficult to insert the tip of the catheter inside the cavity and inflate the balloon with saline. As soon as you inflate the balloon, apply slight upward traction so that you occlude the defect, make sure that you do not overdo it; otherwise, you can make it even bigger, particularly if the injury has to do with the softer right ventricle (Fig. 38.5). This is the part that the balloon catheter helps in stitching up a cardiac wound. What you will see in the books – stating that you can push the balloon inside, put your sutures, and then apply traction at the balloon and occlude your defect again and then repeat the process and complete the repair of the defect – is usually not the case. In most instances the initial obstruction of the defect by the balloon only gives you time to concentrate, probably stabilize the patient, and get ready for the insertion of the first bite. Be prepared: Quite frequently as soon as you insert your first bite, you will hear a popping sound and the balloon will break; you will find again yourself in the situation of having a spurt of blood coming out of the defect. Continue inserting your sutures in a figure of eight as already discussed.