23
Pemphigus
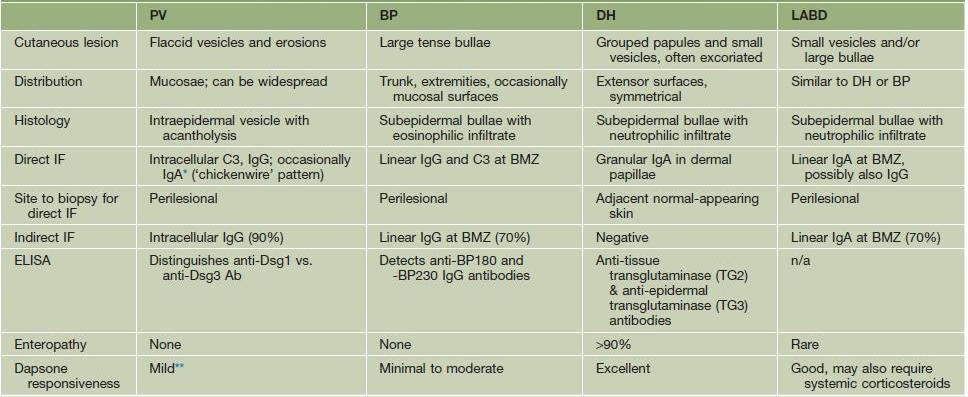
Chapters 23–25 review the major autoimmune bullous diseases (Table 23.1). Because of the significant overlap in their clinical presentations, histologic examination of lesional skin (see Fig. 1.12B) as well as direct immunofluorescence (DIF) of perilesional skin (Figs. 23.1–23.3) are usually required in order to establish a specific diagnosis. Indirect immunofluorescence (IIF) and/or ELISA of sera provide additional helpful information; for example, the latter can detect anti-desmoglein 3 (Dsg3) versus anti-Dsg1 antibodies.
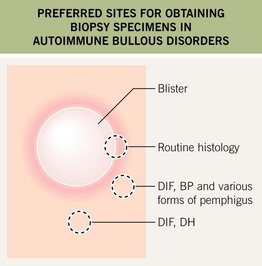
Fig. 23.1 Preferred sites for obtaining biopsy specimens in autoimmune bullous diseases. If the edematous papule or vesicle is small enough, it can be removed in its entirety for routine histology. Otherwise, a biopsy specimen that includes the inflammatory rim as well as the edge of a fresh vesicle or bulla is appropriate. In bullous pemphigoid (BP) and pemphigus vulgaris, a perilesional biopsy is done for direct immunofluorescence (DIF), whereas in dermatitis herpetiformis (DH), nearby normal skin is preferred for DIF.
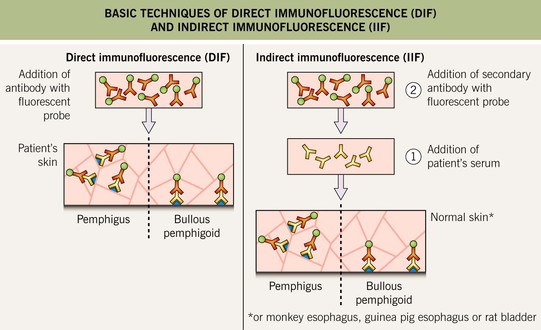
Fig. 23.2 Basic techniques of direct immunofluorescence (DIF) and indirect immunofluorescence (IIF). DIF is performed on skin biopsies to detect tissue-bound immunodeposits (see Fig. 23.1). IIF is performed utilizing patients’ sera to detect circulating autoantibodies that bind epithelial antigens. The preferred substrate for IIF is monkey esophagus for pemphigus vulgaris, guinea pig esophagus for pemphigus foliaceus, and human skin for the pemphigoid group and LABD.
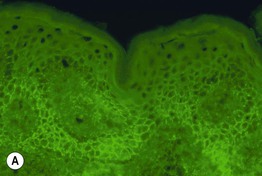
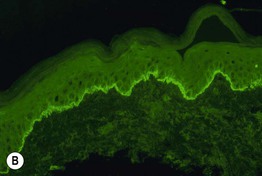
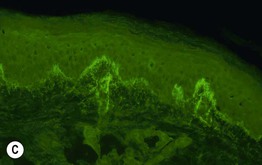
Fig. 23.3 Direct immunofluorescence (DIF) of skin in patients with pemphigus vulgaris (PV), bullous pemphigoid (BP), and dermatitis herpetiformis (DH). A Intercellular deposits of IgG within the lower epidermis in a chickenwire pattern (PV). B Linear deposits of C3 at the basement membrane zone (BP); a similar pattern of IgA deposition is seen in linear IgA bullous dermatosis. C Granular deposits of IgA within the dermal papillae (DH). Courtesy, Christine Ko, MD.
Pemphigus is classically divided into three major groups: (1) pemphigus vulgaris, with pemphigus vegetans representing a rare variant; (2) pemphigus foliaceus, with pemphigus erythematosus representing an unusual localized variant, and fogo selvagem, an endemic form; and (3) paraneoplastic pemphigus. Additional subtypes include the two forms of IgA pemphigus and drug-induced pemphigus.
Pemphigus Vulgaris and Pemphigus Vegetans
• The decrease in cell–cell adhesion leads to the separation of individual keratinocytes from one another (referred to as acantholysis) and the formation of a split within the epidermis or mucosal epithelium, primarily in its lower portion, just above the basal layer (see Fig. 1.12B).
• Clinically, almost all patients with pemphigus vulgaris have painful erosions of the oral mucosa and at least half will have flaccid bullae of the skin plus erosions due to their rupture; lesions can be localized or widespread (Fig. 23.4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree