Pediatrics
DEFINITION
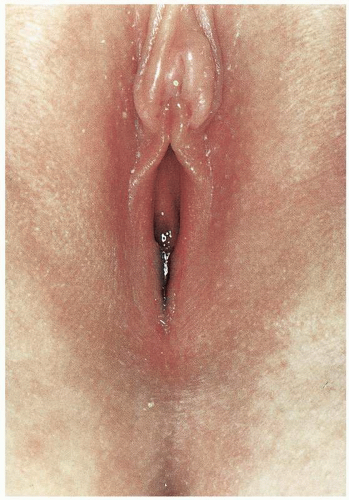
Fusion of the labia minora results in labial adhesion or agglutination.
GENERAL FEATURES
The incidence of childhood labial agglutination is unknown, although it appears to be a rare problem. The etiology of the condition is poorly understood. Labial agglutination may be a consequence of a developmental abnormality (congenital) or may evolve as a consequence of labial and vestibular irritation initiating denuded epithelial surfaces that adhere to one another as a consequence of their close proximity.
CLINICAL PRESENTATION
The usual patient with labial adhesions will be brought to the clinic by her concerned mother who has noted
no orifice at the vaginal opening. She will describe what appears to be an abnormality and will request further evaluation. Occasionally a child with labial adhesion will present with recurrent vaginal infections and urinary difficulties such as cystitis. The latter will be the case especially if labial fusion has resulted in almost complete obliteration of the vestibule.
no orifice at the vaginal opening. She will describe what appears to be an abnormality and will request further evaluation. Occasionally a child with labial adhesion will present with recurrent vaginal infections and urinary difficulties such as cystitis. The latter will be the case especially if labial fusion has resulted in almost complete obliteration of the vestibule.
MICROSCOPIC FINDINGS
The clinical findings do not require biopsy. The vestibular epithelium of the child, with the exception of the newborn, is not glycogen rich and is nonkeratinized. No specific pathologic findings are known to be associated with labial agglutination of the newborn. In some societies where female circumcision is practiced, labial agglutination is relatively common and may be associated with introital stenosis and keratinous cysts.
ADJUNCTIVE STUDIES
None.
DIFFERENTIAL DIAGNOSIS
The patient with a markedly adherent introitus may create concerns that one is dealing with an atretic vaginal canal of müllerian agenesis or androgen insensitivity syndrome. Placement of a lubricated cotton swab within the introital orifice will demonstrate the thin groove representing the adherent labia.
CLINICAL BEHAVIOR AND TREATMENT
For the asymptomatic child with labial agglutination that is too adherent to separate gently in the office, topical estrogen cream, applied once per evening for 2 weeks may resolve the agglutination, and typically no further therapy is warranted. It is not in the patient’s best interest to undergo general anesthesia for separation of the labia unless symptoms warrant such an invasive procedure. If the patient suffers from recurrent vaginal infections or bladder infections, the procedure is indicated. If indications are present for the procedure, and gentle traction in the office demonstrates markedly agglutinated labia, the procedure is best accomplished under appropriate anesthesia. Usually, placement of a probe or cotton swab to the adhesion, with gentle traction toward the perineum, will result in separation of the labia. Without postoperative separation of these denuded epithelial surfaces, fusion will recur. A time-honored approach to this problem has been the daily application of estrogen cream to the introitus. Although no pharmacologic data exist to support the antiadhesion benefit of estrogen creams, the effect may be related to maturation of the epithelium of the labia minora and vestibule. Topical estrogen is regularly used and is often successful. It may be that the benefit of the application is in part mechanical and that daily separation of the labia while applying the estrogen cream allows for epithelialization to occur and diminishes the chance of subsequent adhesion of the labia. This approach may be used as a substitute for surgery in the patient who has evidence of minimal agglutination.
Parents of the infant should be reassured that there is no evidence of a major abnormality, and if the infant is asymptomatic, the parents may be reassured that the labial orifice may expand on its own with the passage of time.
PROGRESSIVE THERAPEUTIC OPTIONS
Progressive therapeutic options are as follows:
In the asymptomatic patient, observation alone with reassurance should be adequate. If the parent wishes “to intervene,” daily application of estrogen cream for 2 weeks may be attempted, accompanied by gentle traction.
For the symptomatic patient, attempt gentle separation in the office. Markedly adherent labia will require lysis in the operating room if there is no response to topical estrogen. A “pediatric pain cocktail” may be administered to avoid anesthesia; however, close cardiopulmonary monitoring will be necessary. Postoperative daily separation of the labia by the parent is mandatory until reepithelialization has been completed. Estrogen cream may be applied during these daily efforts.
DEFINITION
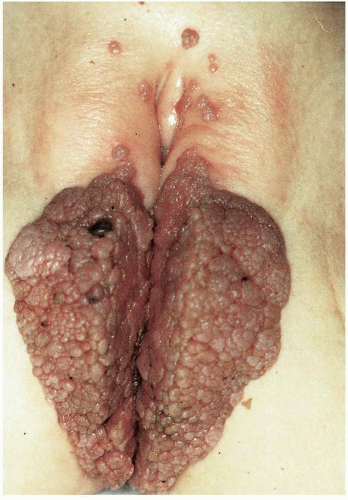
Condyloma acuminatum (pl. condylomata acuminata) (venereal wart, genital wart) is derived from the Greek phrase for caruncle and the Latin phrase for sharply pointed, and as such the terminology adequately defines the condition caused by human papillomavirus (HPV).
GENERAL FEATURES
HPV-related genital infection is the most common sexually transmitted disease seen by obstetricians and gynecologists. Increasingly, sexually active adolescents present with obvious venereal warts, or less obvious but more frequent abnormal cervical cytology, as a consequence of HPV infection. Vulvar venereal warts may be observed in early infancy and may be acquired during transmission through an infected birth canal or, in some cases, as a consequence of sexual abuse.
The incubation period for HPV may be prolonged, and clinical evidence of a viral infection acquired during transmission through an infected birth canal may not be apparent for months or perhaps years after birth. Often in children the actual mode of transmission remains unknown. With advent of sexually activity in early to late adolescence the mode of transmission becomes much more apparent.
CLINICAL PRESENTATION
The child with vulvar condyloma acuminatum will usually be brought to the physician for evaluation of the warty, macular or papular lesions. Often this may be delayed and the process may be diffuse when first seen by the physician. Immunosuppressed patients, especially
children with diabetes, may manifest diffuse disease. In such patients it is not uncommon to see warts elsewhere on the body surface.
children with diabetes, may manifest diffuse disease. In such patients it is not uncommon to see warts elsewhere on the body surface.
Condylomata are typically multiple and may involve the vulvar vestibule; labia minora and labia majora, including hair-bearing; skin and the perianal area. The application of 3% topical acetic acid (or white vinegar), which will make the lesions whiter and distinct from the adjacent normal mucosa or skin, and examination with an illuminated magnification device, or colposcope, is usually helpful because the lesions can be quite small and skin colored, although some are red or pink in color.
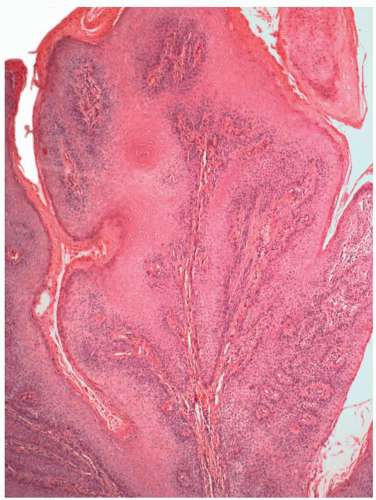
MICROSCOPIC FEATURES
Condylomata acuminata may be verrucous, papillary, or sessile, although some may be macular or papular in character. In larger exophytic papillary lesions, complex branching papillae are usually present. Variable degrees of epithelial thickening are usually seen with acanthosis and crowding of parabasal cells. Koilocytosis is usually seen in some keratinocytes in the upper third of the epithelium, although this may not be evident in lesions that have prominent dyskeratosis, parakeratosis, and hyperkeratosis. The hyperplastic epithelial changes are associated with exaggerated intracellular bridges. The nuclei are usually not atypical, although some increased numbers of normal-appearing mitotic figures may be evident. Condyloma acuminatum that have moderate to severe nuclear atypia should be classified as condyloma acuminatum with high-grade vulvar intraepithelial neoplasia (VIN 2-3).
ADJUNCTIVE STUDIES
The child with vulvar condyloma acuminatum should be suspect for other venereal diseases, and appropriate studies should be obtained. These would include cultures for gonorrhea, assays for chlamydia, serology for syphilis, and serology for human immunodeficiency virus (HIV). Consideration should also be given to evaluating for systemic diseases that may impair host immune defense, such as diabetes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree