Patterns
Intro to Pattern Analysis
In the 1980s, the “ABCD” clinical criteria for melanoma enabled the clinician to use an algorithm for melanoma diagnosis and therefore helped with earlier detection of melanoma. In 2004, “E” was added to the rule to produce the commonly used ABCDE rule for melanoma diagnosis. These criteria for melanoma diagnosis give the lesion in question a score depending on its Asymmetry, Border, Color, Differentiating structures/Diameter >6 mm, and Evolution, or noticed change, within the last few months. Each of these categories is given a number score depending on how many criteria they meet within each category. For example, if a lesion had three distinguishable colors, it would receive a number 3 for the color category. The scores are then totaled and weighed; if the lesion has a total score over 5.45, it is considered a melanoma. This method can be a useful tool for patients to assess their nevi at home, but also can be used by clinicians using dermoscopy to assess each feature more closely.1
Beginning with the handheld dermatoscope, noninvasive technology now enables clinicians to diagnose melanomas and nonmelanoma skin cancers at earlier and earlier stages, as well as prevent biopsies of otherwise benign lesions. Since the advent of this new technology, we are now making the diagnosis of melanoma for lesions that do not yet demonstrate the classic ABCD and even E’s of melanoma and have needed to develop new algorithms for identification and diagnosis.
Pattern analysis provides a stepwise analysis using common patterns and criteria to determine whether a lesion is melanocytic or nonmelanocytic. The lesion is then analyzed to determine which subcategory it falls into and ultimately what the lesion is and therefore whether or not the lesion is suspicious. Whether a lesion is melanocytic or nonmelanocytic can be a very difficult distinction to make, especially when lesions present with very similar patterns; for example, certain types of lentigo lesions (which are nonmelanocytic) can appear similar to a junctional nevus (which is melanocytic). In the color wheel algorithm, it is not as critical to make the distinction between melanocytic and nonmelanocytic or even the final diagnosis of the lesion. Rather, we use pattern analysis as the last step in the algorithm to confirm the need to biopsy and to further narrow down a significantly shortened list of possibilities.
The 7-point checklist is exactly as it sounds: seven criteria that determine a score that helps to determine whether or not the lesion in question is melanoma or otherwise. The criteria are split into two groups that are weighted differently: major and minor criteria. The major criteria include an atypical pigment network, gray-blue areas, and atypical vascular pattern; each receives a score of 2, if present. The minor criteria include radial streaming or streaks, irregular diffuse pigmentation or blotches, irregular dots and globules, and regression pattern; each of these criteria receives a score of 1, if present. If a lesion has a total score of three or more, the lesion is given the diagnosis of melanoma.2
In an effort to streamline and standardize the various methods and algorithms of dermoscopy, a virtual consensus meeting was held in which 40 expert dermoscopists analyzed and reviewed the diagnostic criteria of over 100 lesions. From this meeting, the 2-point checklist was introduced. The first step determines whether the lesion is melanocytic or nonmelanocytic. This is done by first determining if the lesion has any characteristic melanocytic structures in a specific order. If none are found, then any nonmelanocytic features are assessed and determined (dermatofibroma, seborrheic keratosis, angioma, or malignant basal cell and squamous cell carcinoma [SCC]). If still none are identified, then the lesion is analyzed for blood vessel
morphology. If still nothing can be identified, the lesion is termed structureless. The second step is only used if the lesion is determined to be melanocytic. The second step uses one of the previous explained algorithms (pattern analysis, 7-point checklist, etc.) to determine whether the lesion is benign or malignant.3
morphology. If still nothing can be identified, the lesion is termed structureless. The second step is only used if the lesion is determined to be melanocytic. The second step uses one of the previous explained algorithms (pattern analysis, 7-point checklist, etc.) to determine whether the lesion is benign or malignant.3
As one might expect, these methods have their advantages and disadvantages. If you are familiar with them, you are in a good place to start; if you are not familiar with them, have no fear; everything will be explained as we go along. Our approach synthesizes well-established clinical knowledge of the behavior and characteristics of lesions and presents them in an easy-to-follow series of four steps.
To begin our discussion of how dermoscopy can best assist you in your practice, we need to lay the groundwork for confidently identifying benign versus malignant lesions. In this chapter, we will highlight the basic patterns and colors seen in benign lesions and malignant lesions and where the two are often confused.
Keep in mind that the majority of melanomas <1 cm are not clinically obvious, which is precisely why dermoscopy is useful in these situations. When a melanoma is clinically obvious, dermoscopy is not needed. We will be presenting some very challenging clinical pictures of early melanomas, so don’t get discouraged! We’ll provide you with the skills to tackle these tricky presentations.
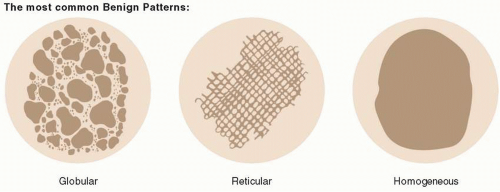
Benign Melanocytic Patterns
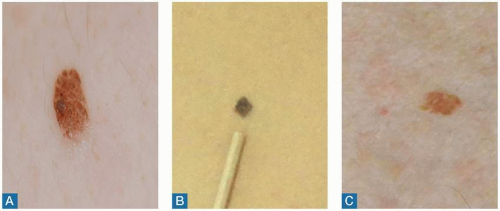
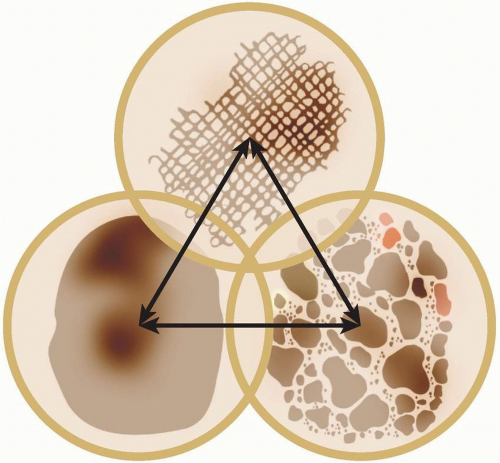
Figure 1.1 shows the three most common benign melanocytic patterns: reticular, globular, and homogenous. If you are considering benign versus malignant nevi, these are the benign patterns that you should be looking for.
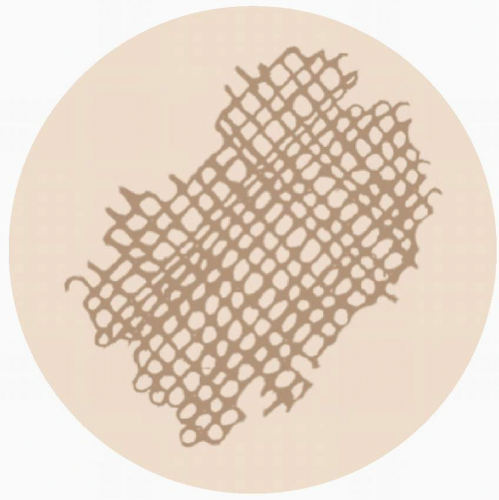
Reticular Pattern
The reticular pattern is characterized by a uniform network that thins at the periphery (Figures 1.2 and 1.3).
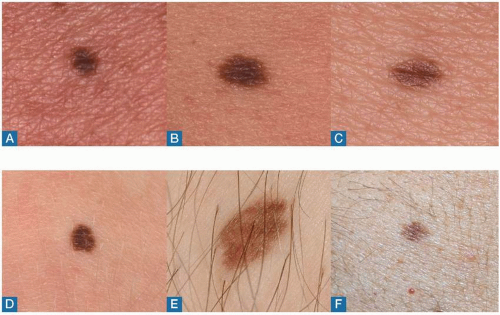
Figure 1.4 demonstrates six examples of junctional nevi (JN), clinically flat lesions with corresponding dermoscopic images (Figure 1.5) that show a clear uniform network with thinning at the periphery—this is characteristic of JN. Note that there is some faint, hypopigmentation (lightening) around the hair follicles. White is not considered a color, and this feature can make a lesion look like it has asymmetry or color variation at times. However, keep in mind that it is the overall symmetry of the lesion that makes it symmetric.
Takeaway: Perifollicular hypopigmentation can be seen in both benign and malignant lesions. It does not contribute to overall lesion asymmetry or lesion color variation.
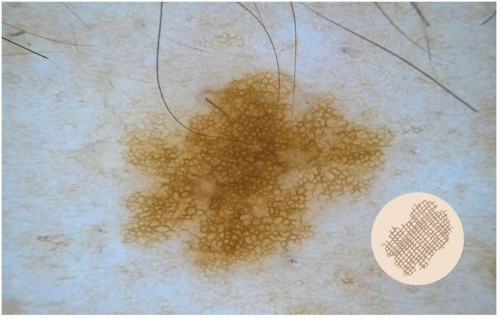 FIGURE 1.3 A dermoscopic example of a reticular pattern. A reticular pattern is characterized by a uniform network that thins at the periphery. |
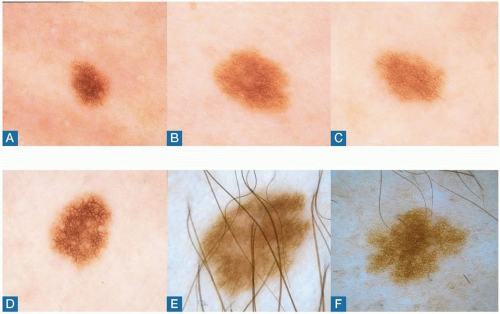 FIGURE 1.5 The corresponding dermoscopic images for the six lesions in Figure 1.4, demonstrating a uniform network thinning at the periphery. Note that there is some hypopigmentation (lightening) around the hair follicles. |
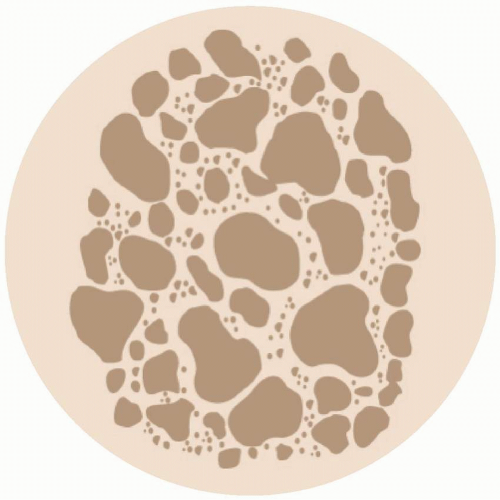
Globular Pattern
The globular pattern is characterized by diffuse globular dots throughout the lesion (Figures 1.6 and 1.7).
Figure 1.8 demonstrates three examples of congenital nevi (CN), clinically elevated lesions with corresponding dermoscopic images (Figure 1.9) showing a diffuse globular pattern.
Note that there is a cobblestone pattern in lesions A and C, as well as some darker dots in lesion B. Asymmetric, dark dots at the periphery of a lesion are often an indication of a malignant feature, but two-tone dark dots evenly distributed throughout a lesion, or centrally located, are benign.
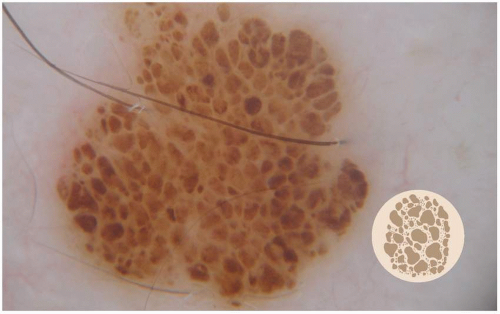 FIGURE 1.7 A dermoscopic example of a globular pattern. A globular pattern is characterized by diffuse dots and globules throughout the lesion. |
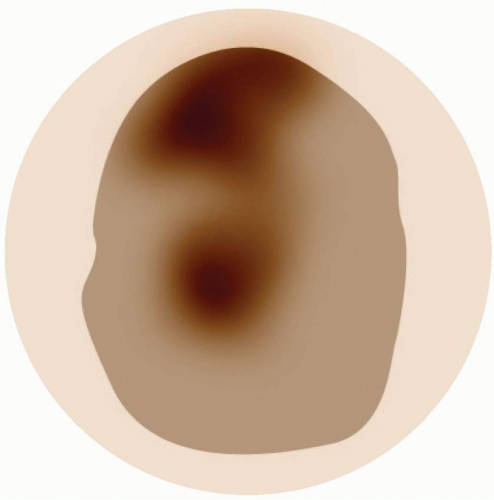
Homogenous Pattern
The homogenous pattern is characterized by a diffuse structureless/nonspecific area. There is neither a reticular network nor globules (Figures 1.10 and 1.11).
The “Tyndall effect” can also be observed in Figures 1.12, 1.13 and 1.14. This is a remarkable blue tint that can be seen with lesions that are deep and dense such as intradermal nevi, CN, blue nevi, and, sometimes, seborrheic keratosis in darker-skinned patients.
Figure 1.13 shows a clinical example of an intradermal nevus (IN). This lesion has a welldefined border and resembles other lesions in the neighborhood, which is a good sign of a benign lesion. This clinical picture helps us to not confuse the dermoscopic picture as malignancy.
Figure 1.15 shows the clinical picture of Figure 1.14, a benign IN. The lesion is not elevated and has a well-defined border.
Pearl
The Tyndall effect can be confused with the blue white veil is only seen in nodular-type melanoma! Remember your clinical history and evaluation! Intradermal, congenital, and blue nevi will have a long-standing history without change, whereas a melanoma will have appeared recently and developed quickly. Additionally, the blue-white veil is only seen in nodular-type or elevated melanomas, which will often have other malignant signs in addition to the blue-white veil (Figure 1.14).
 FIGURE 1.9 The corresponding dermoscopic images for the three lesions in Figure 1.8, demonstrating a diffuse dot/globular pattern. Note that there is a cobblestone pattern in lesions (A) and (C) and some dark dots in lesion (B). |
 FIGURE 1.10 A homogenous pattern is characterized by a diffuse structureless area. There is neither a network nor globules. |
 FIGURE 1.12 A dermoscopic example of a homogenous pattern in an intradermal nevus (IN). A homogenous pattern is characterized by a diffuse structureless area. There is neither a network nor globules. |
 FIGURE 1.13 A clinical example of an intradermal nevus (IN). This lesion has a well-defined border and resembles other lesions, which is often the case with benign lesions. |
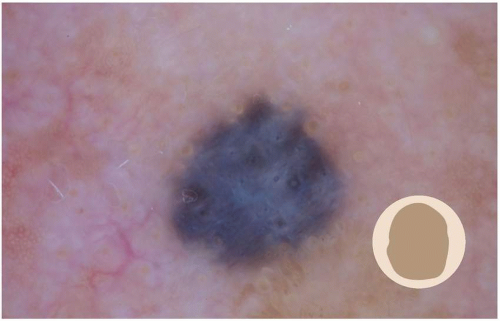
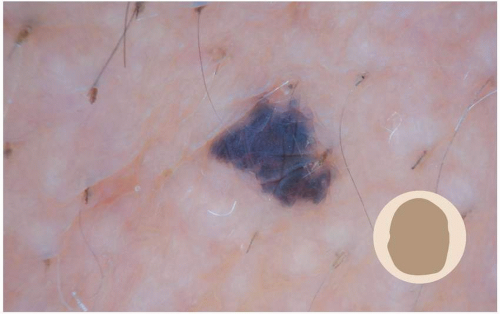
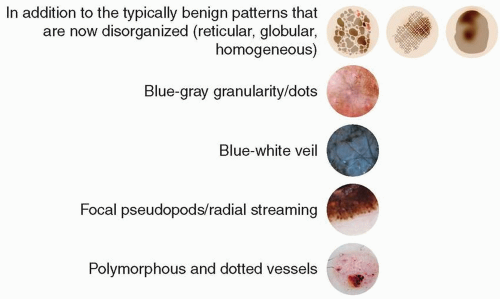
Malignant Melanocytic Patterns
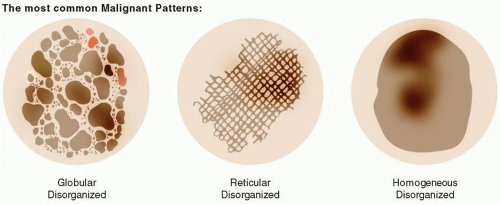
Now that we have a foundation for benign melanocytic patterns, we can introduce the characteristic malignant melanocytic patterns that, if seen in a lesion, raise the suspicion of melanoma (Figure 1.16). Essentially, the malignant patterns are the same as benign, but are no longer diffuse throughout the nevus, but rather disorganized. Then, there are four malignant features that are characteristic of malignant melanomas: blue-gray granularity/dots in superficial lesions,
blue-white veil in nodular lesions, focal pseudopods/radial stream, and polymorphous or dotted vessels that are clustered together asymmetrically (as opposed to the symmetric defined pigment network of dots and globules). These features, if seen, are an indication to biopsy the lesion. We’ll go into each in detail, so don’t get overwhelmed!
blue-white veil in nodular lesions, focal pseudopods/radial stream, and polymorphous or dotted vessels that are clustered together asymmetrically (as opposed to the symmetric defined pigment network of dots and globules). These features, if seen, are an indication to biopsy the lesion. We’ll go into each in detail, so don’t get overwhelmed!
Also keep in mind that the delineation of benign versus malignant is not so black and white. Benign nevi and malignant melanoma can overlap—these are known as atypical or dysplastic nevi or intraepidermal melanocytic proliferations (Figure 1.17).
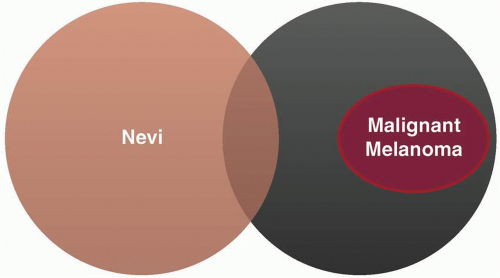 FIGURE 1.17 Benign nevi and malignant melanoma can have overlap. These lesions are known as atypical or dysplastic nevi or intraepidermal melanocytic proliferations. |
In Figure 1.18, we see our normal patterns that have become disorganized and are now indicative of melanoma: reticular disorganized, globular disorganized, and homogenous disorganized.
Reticular Disorganized Pattern
The reticular disorganized pattern is characterized by a nonuniform network that is darkened and thick at the periphery. Figures 1.19 and 1.20 illustrate the schematic and a dermoscopic example.
Figures 1.21 and 1.22 depict three melanomas that have the characteristic reticular disorganized pattern: nonuniform network with a darkened and thick periphery.
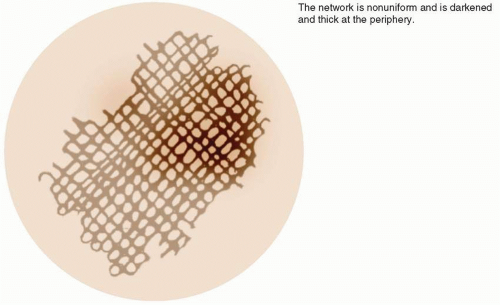 FIGURE 1.19 A reticular disorganized pattern is characterized by a nonuniform network that thickens and darkens at the periphery. |
 FIGURE 1.20 Reticular disorganized pattern is characterized by a nonuniform network that thickens and darkens at the periphery. |
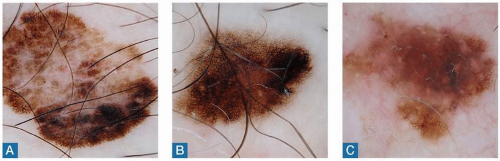 FIGURE 1.22 The corresponding dermoscopic images for the three lesions in Figure 1.21, demonstrating a reticular disorganized pattern. The network is nonuniform and is darkened and thick at the periphery. |
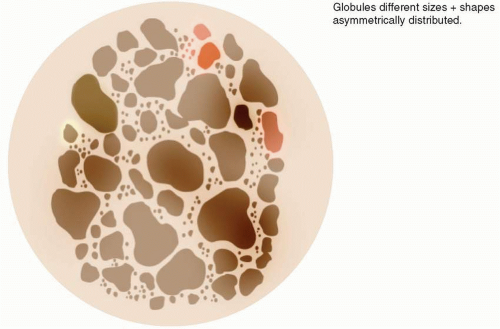
Globular Disorganized Pattern
The globular disorganized pattern is easily identified by globules of different sizes and shapes that are asymmetrically distributed. Figures 1.23 and 1.24 illustrate a schematic and a dermoscopic example.
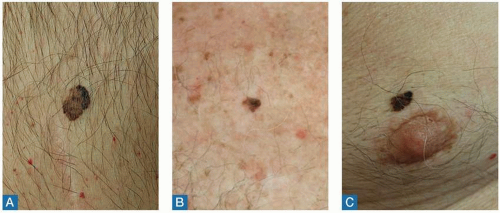
Figures 1.25 and 1.26 show three examples of corresponding clinical and dermoscopic images of malignant melanomas that clearly demonstrate this globular disorganized pattern. Dots of different colors, sizes, and shapes are scattered asymmetrically throughout each lesion.
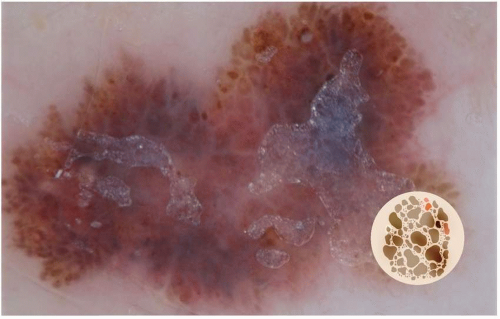 FIGURE 1.24 A dermoscopic example of a disorganized dot globular pattern. Globular disorganized pattern is characterized by globules of different sizes and asymmetrically distributed shapes. |
Homogenous Disorganized Pattern
The homogenous disorganized pattern characteristically has neither network or globules nor one defined color, but has many colors, as well as a diffuse homogenous area (Figure 1.27).
Figure 1.28 is a dermoscopic example of this pattern; there are no definitive networks or globules, but there are clearly different colors of red, pink, and brown spread asymmetrically throughout the lesion.
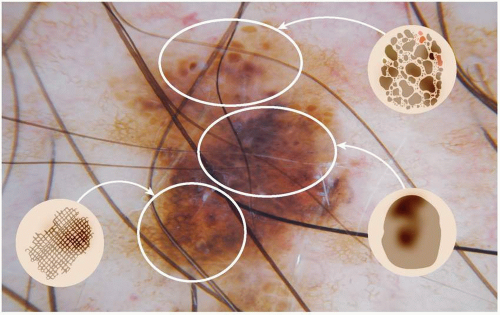
These malignant patterns can even be seen together in an individual lesion (Figure 1.29). Figures 1.30 and 1.31 show examples of how this may present under the dermatoscope. Oftentimes, people think that melanomas have to be darkly pigmented, but these two examples show how the darkness of the pigment is not a requirement for malignancy; rather, the three malignant patterns can be clearly seen with and without heavy pigment.
As mentioned before with the benign homogenous pattern, oftentimes, we immediately associate the color blue with melanoma. However, this is not always true! There are two instances when blue does indicate malignancy: blue-gray granularity in flat/superficial lesions and bluewhite veil in nodular/elevated lesions. If you see blue elsewhere, it is just the Tyndall effect discussed earlier in this chapter.
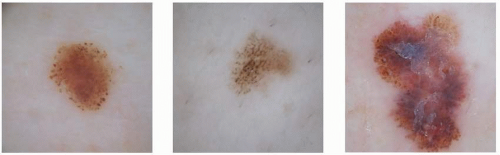 FIGURE 1.26 The corresponding dermoscopic images for the three lesions in Figure 1.25, demonstrating a globular disorganized pattern. Globular disorganized pattern is characterized by globules of different sizes and asymmetrically distributed shapes. |
 FIGURE 1.28 A dermoscopic example of a disorganized homogenous pattern. A homogenous pattern has no network, no globules, and many colors. |
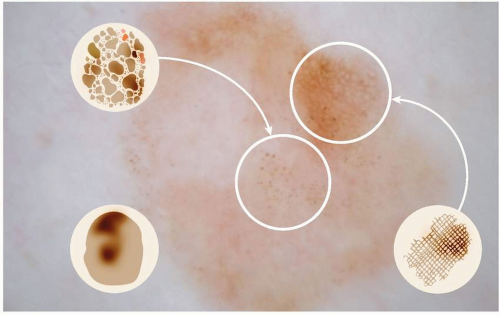 FIGURE 1.31 These disorganized patterns can all be present in a malignant lesion.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|