Vascular anomalies are localized defects of vascular development. Most of them occur sporadically (ie, there is no familial history of lesions, yet in a few cases clear inheritance is observed). These inherited forms are often characterized by multifocal lesions that are mainly small in size and increase in number with patients’ age. The authors review the known (genetic) causes of vascular anomalies and call attention to the concept of Knudson’s double-hit mechanism to explain incomplete penetrance and large clinical variation in expressivity observed in inherited vascular anomalies. The authors also discuss the identified pathophysiological pathways involved in vascular anomalies and how it has opened the doors toward a more refined classification of vascular anomalies and the development of animal models that can be tested for specific molecular therapies.
Vascular anomalies are localized defects of vascular development. Most of them occur sporadically (ie, there is no familial history of lesions, yet in a few cases clear inheritance is observed). These inherited forms are often characterized by multifocal lesions that are mainly small in size and increase in number with patients’ age. On the basis of these inherited forms, molecular genetic studies have unraveled a number of inherited mutations giving direct insight into the pathophysiological cause and the molecular pathways that are implicated. Genetic defects have been identified for hereditary haemorrhagic telangiectasia (HHT), inherited cutaneomucosal venous malformation (VMCM), glomuvenous malformation (GVM), capillary malformation-arteriovenous malformation (CM-AVM), cerebral cavernous malformation (CCM), and some isolated and syndromic forms of primary lymphedema. The authors focus on these disorders, the implicated mutated genes, and the underlying pathogenic mechanisms. The authors also call attention to the concept of Knudson’s double-hit mechanism to explain incomplete penetrance and the large clinical variation in expressivity of inherited vascular anomalies. This variability renders the making of correct diagnosis of the rare inherited forms difficult. Yet, the identification of the pathophysiological causes and pathways involved in them has had an unprecedented impact on our thinking of their etiopathogenesis, and has opened the doors toward a more refined classification of vascular anomalies. It has also made it possible to develop animal models that can be tested for specific molecular therapies, aimed at alleviating the dysfunctions caused by the aberrant genes and proteins.
Vascular anomalies are histopathologically characterized by a focal increase in the number of vessels that are abnormally tortuous and enlarged. This phenomenon is likely caused by localized defects in vascular development during vasculogenesis and especially during angiogenesis. Vasculogenesis is defined as vessel growth from embryonic cells: hemangioblasts (mesoderm derived precursors) that give rise to angioblasts (endothelial precursors) and hemocytoblasts (blood cell precursors). Angioblast fusion takes place in vascular islets inducing the formation of the primary capillary plexus. During angiogenesis, this primary capillary system extends and matures. It involves both endothelial cell proliferation and mural cell recruitment to generate the fully developed and functional vascular and lymphatic trees. The pathophysiological studies of vascular anomalies have been helped by the astounding parallel progress made in understanding the factors and regulation of the development of the lymphatic and vascular systems.
Several angiogenic factors, such as vascular endothelial growth factors (VEGFs), fibroblast growth factors, platelet derived growth factor beta (PDGF-beta), and angiopoietins (ANGPT-1 and ANGPT-2) regulate angiogenesis. They activate precursor cells, and lead to migration, proliferation, and differentiation of the primary capillary plexus. Vascular endothelial growth factors, angiopoietins, and their endothelial tyrosine kinase receptors are central regulators of vasculogenesis, angiogenesis, and lymphangiogenesis.
Most vascular anomalies are sporadic, yet rare familial cases have been recorded. These forms have allowed to use molecular genetics for the identification of the underlying causes ( Table 1 ). This molecular characterization of the inherited forms has subsequently led to hypothesize on the causes of the more common sporadic forms. In the first such extrapolation, this was shown to be true. Thus, there is hope that in the near future, the molecular basis of vascular anomalies will be deciphered, allowing a precise classification of all of them. Moreover, some inherited forms have been proven to follow paradominant inheritance, which may be a general rule. Thus, inhibition of second hits may play a role in prevention of lesions in the familial forms. Finally, the data have laid the ground to develop specific in vitro and in vivo models of vascular anomalies. These can be used to characterize in detail the pathophysiological mechanisms and to develop novel specific treatments.
| Vascular Anomaly | Clinical Signs | Linked Locus/Loci | Mutated/Predisposing Gene |
|---|---|---|---|
| Hemangioma | Erythematous macular patch, blanched spot or telangiectasia with rapid postnatal growth | — | VEGFR2/TEM8, predisposing variants |
| Venous malformation (VM) | Bluish lesion compressible on palpation | — | TIE2, 40%–50% |
| Cutaneo-mucosal venous malformation (VMCM) | Multiple small punctate bluish spots | 9p21-22 | TIE2 |
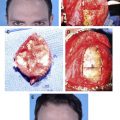
| Glomuvenous malformation (GVM) | Small, multifocal bluish-purple, cobblestone and hyperkeratotic lesions | 1p21-22 | Glomulin |
| Capillary malformation-Arteriovenous malformation (CM-AVM) | Multifocal capillary malformation with pale halo, AVM, AVF, Vein of Galen, aneurysmal malformation, Parkes Weber syndrome | 5q13-22 | RASA1 |
| Hereditary hemorrhagic telangiectasia (HHT1/HHT2/HHT3/HHT4) | Epistaxis, telangiectasia, AVM (lung, liver, brain, gastrointestinal tract) | 9q33-34/12q11-14/5q/7p14 | ENG/ ACVRL1/?/? |
| HHT juvenile polyposis (JPHT) | HHT with juvenile polyposis | 18q21 | SMAD4 |
| Angioma serpiginosum | Patchy capillary malformation with dilated capillaries following Blaschko’s lines, mild nail, hair dystrophy, papillomatosis | Xp11.3-Xq12 | PORCN ? |
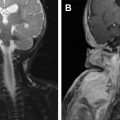
| Cerebral cavernous malformation (CCM1/CCM2/CCM3) | Cerebral capillaro-venous malformations, and sometimes cutaneous lesions (HCCVM) | 7q21-Q22/7p15-p13/3q25.2-27 | KRIT1/malcavernin/PDCD10 |
| Nonne-Milroy syndrome | Lymphedema, hydrocele, large caliber leg veins, cellulitis, curled toenails, papillomatosis | 5q34-35 | VEGFR3 |
| Lymphedema-distichiasis | Lymphedema, distichiasis, ptosis, yellow nails, syndactyly, cleft palate, and cardiac septal defects | 16q24.3 | FOXC2 |
| Hypotrichosis-lymphedema-telangiectasia (HLT) | Sparse hair, lymphedema, and cutaneous telangiectasias | 20q13.33 | SOX18 |
| Hennekam syndrome | Peripheral lymphedema, with visceral involvement, mental retardation and unusual, flat face, hypertelorism, and broad nasal bridge | 18q21.32 | CCBE1 |
| OLEDAID | Osteoporosis lymphedema anhidrotic ectodermal dysplasia with immunodeficiency | Xq28 | NEMO |
| Primary congenital resolving lymphedema | Early onset lymphedema with papillomatosis resolving at 30 to 40 year of age | 6q16.2-q22.1 | ? |
| Aagenaes syndrome or hereditary lymphedema cholestasis (HLC) | Extended lymphedema of lower extremities, malabsorption, growth retardation, rickets, cholestatic jaundice, and hepatomegaly | 15q | ? |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree