Partial Face Transplant
B. DEVAUCHELLE
EDITORIAL COMMENT
This was groundbreaking microsurgery with a startling result. This surgery is still considered experimental, but the obvious improvement in the patient will encourage other centers to follow.
Extended soft-tissue defects of the face are very difficult to reconstruct, especially when multiple anatomic units like the nose, lips, and chin are missing simultaneously. Under such circumstances, several conventional autologous tissue transfers are necessary to restore the form and, if possible, the function, of each of the missing parts of the damaged face. The idea was raised that in such cases, a one-stage reconstruction of the central and lower face could be achieved by microsurgical transfer of a full-thickness composite tissue allograft harvested on the cephalic extremity of a brain-dead donor with similar morphologic characteristics.
INDICATIONS
Previous procedures, which often required several secondary corrections, usually led to poor cosmetic and functional outcomes. The original face of the reconstructed patient had an unattractive appearance with many scars and several mismatching skin paddles, all of them remaining mostly immobile and devoid of any future expressive mobility.
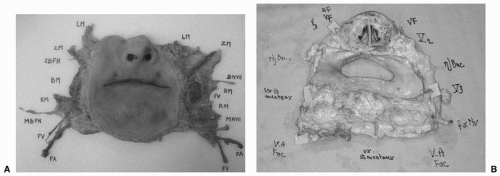
The partial face transplant is a full-thickness composite soft-tissue allograft, including all anatomic components of the nose-lips-chin triangle, harvested down to their skeletal bone support (Fig. 150.1). The transplant is sensate and aims at restoring all complex motor functions devoted to orality—competent feeding, intelligible speech, and restoration of the aesthetic appearance of the central and lower face, with no donor-site morbidity. Furthermore, it allows a one-stage high-quality restoration of an acceptable aesthetic appearance of the central and lower face. Although the ultimate goal of the procedure is certainly not to reach an exact restitution of the recipient’s previous facial identity, the new face, which is finally created with the contribution of the graft, restores a real morphologic individuality to the facial image. A lifelong immunosuppressive treatment remains, at present, a drawback, but is a mandatory medical requirement to obtain the durable benefit of all the surgical advantages.
ANATOMY
The graft is supplied by the right and left facial arteries and veins that, during their ascending course to the medial canthi, give rise to a large number of medial and lateral collateral vessels running into the subcutaneous and submuscular planes. Lateral branches (long and short facial collaterals) are directed to the cheeks, and medial branches distribute to the submental area (submental vessels), to the lips (upper and lower labial vessels), and to the nose. All of these collaterals are richly connected with each other and with branches from
adjacent angiosomes. Major right-left anastomoses crossing the midline exist between the labial, submental, and nasolobar arteries and veins. Thanks to these numerous functional connecting vascular channels, the graft may be revascularized on a single vascular pedicle.
adjacent angiosomes. Major right-left anastomoses crossing the midline exist between the labial, submental, and nasolobar arteries and veins. Thanks to these numerous functional connecting vascular channels, the graft may be revascularized on a single vascular pedicle.
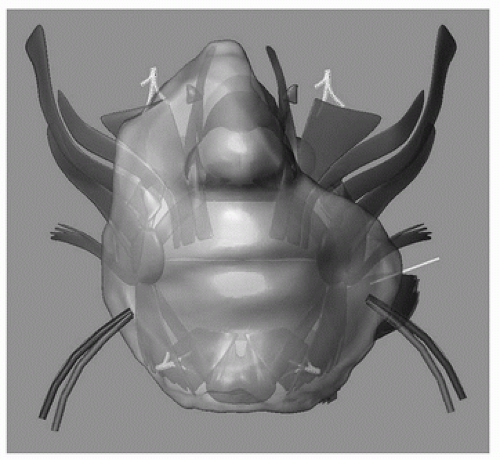 FIGURE 150.1 Schematic anatomic drawing of the nose-lips-chin allograft. Preoperative virtual three-dimensional model of the first partial human face allograft. |
Sensitive nerves to the graft arise from the infraorbital (V2) and mental (V3) nerves on both sides. These nerves leave the corresponding bone foramina on the maxilla and the mandible, and then enter the soft tissues of the mid and lower face; they then quickly divide into small rami distributed to the skin. Due to this early spread in the small terminal rami, the main stem of the maxillary (V2) and inferior alveolar (V3) nerves need to be exposed by an endo-osseous dissection, in order to obtain, after deep subperiosteal elevation of the graft, large proximal nerve stumps suitable for reliable microsurgical anastomoses.
Motor nerves to the graft originate from the terminal zygomatic, buccal, and mandibular branches of the facial nerves, which arise from the parotid area, run laterally above the masseteric fascia, then reach [deep to the superficial muscular aponeurotic system (SMAS) layer] the levator and depressor muscles of the lips. Depending on the extent of the graft, they need to be dissected separately at their exit from the parotid gland or, otherwise, inside the gland or more proximally on the cervico- and temporofacial trunks of the facial nerves.
FLAP DESIGN AND DIMENSIONS
The partial central and lower face allograft is a full-thickness composite tissue transfer, which includes the exact amount of skin necessary to close the recipient’s cutaneous defect, the underlying subcutaneous fat, the four sensitive nerves to these integuments, all perioral muscles with their intact segmental motor nerve supply, the missing cartilage of the nose, the inner lining of both nasal vestibules, and a large patch of anterior and lateral oral mucosa (Fig. 150.2). If necessary, the graft may be enlarged laterally by including the cheeks, with the corresponding buccinator muscles, buccal nerves, and the anterior portion of Bichat’s fat pads.
A brain-dead donor is selected according to strong morphologic and immunologic criteria. Ideally, the anatomic requirements include a similar range of age (within the same decade), the same color and texture of skin, and a comparable overall body habitus. The donor and the recipient should also share the same blood group and have several (as many as possible) positive human leukocyte antigen (HLA) cross-match tests.
OPERATIVE TECHNIQUE