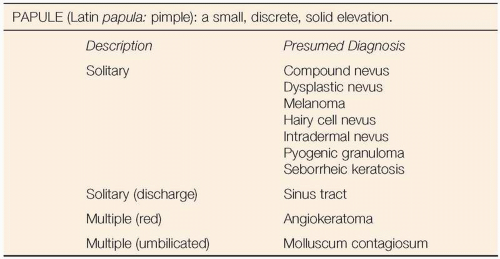
Papules
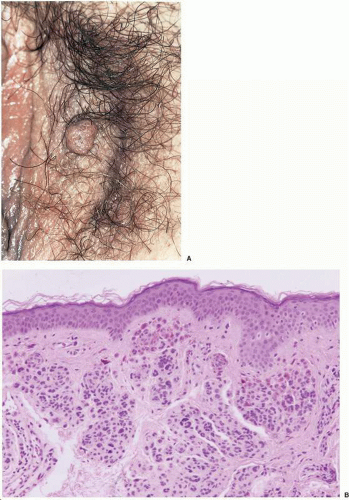
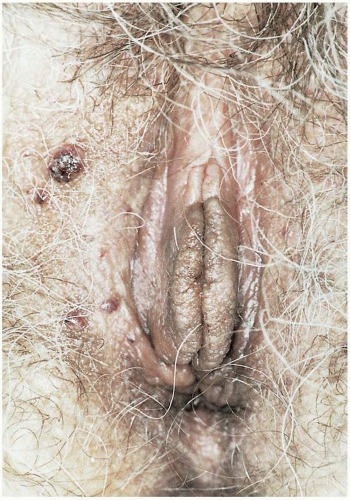 Figure 5.2. Multiple angiokeratoma in a woman with white blood cell α-galactosidase of 36 nM/hr/mg (normal, 50 to 80). Diagnosis of Fabry’s disease was made, and lesions were ablated with a laser. |
DEFINITION
Angiokeratoma is a benign vascular papular lesion containing dilated subepithelial dermal blood vessels that abut the basal epithelial layer.
GENERAL FEATURES
The etiology for these vascular lesions is unknown. Although they are frequently seen in vulvar clinics, the actual incidence in the population at large is unknown.
CLINICAL PRESENTATION
The patient with an angiokeratoma will usually be asymptomatic and of reproductive age. The lesion is usually noted on routine pelvic examination as a small 2- to 5-mm papular lesion. They are often multiple and usually involve only the vulva. Rarely, an angiokeratoma may ulcerate and bleed, as may occur when the clitoris is involved. Unless it has been irritated, an angiokeratoma will not be tender. Color ranges from black to dark red to purplish in hue. Multiple angiokeratomas may be noted in patients with Fabry’s disease, an X-linked recessive disease associated with a deficiency of α-galactosidase A, resulting in deposition of glycosphingolipids throughout a number of body tissues. The disease may be noted in women in the heterozygous state. Heterozygous women usually do not have a severe form of the disease; however, they may have renal involvement resulting in proteinuria, corneal involvement resulting in corneal opacities, neurologic involvement resulting in paresthesias, and dermatologic involvement resulting in angiokeratomas.
MICROSCOPIC FINDINGS
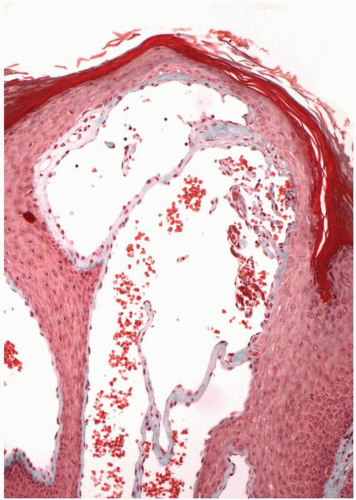
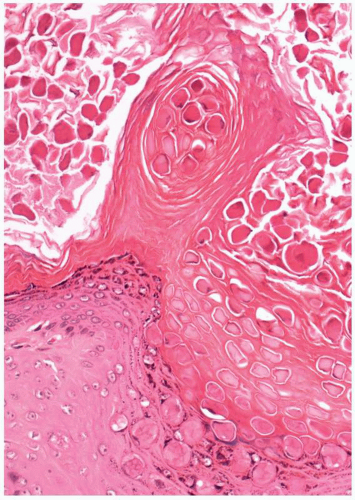
Angiokeratomas are considered variants of hemangiomas. They are characterized by prominent endothelial-lined, blood-filled vascular channels immediately
beneath the basement membrane of the overlying epithelium and separated by the rete ridges of the epithelium. These ridges result from down growth of the overlying epithelium and form epithelial strands and cords that separate the vascular channels, resulting in the multilocular, lobulated appearance. The overlying epithelium usually has some degree of acanthosis and papillomatosis, as well as hyperkeratosis. A mild, chronic inflammatory infiltrate may be seen in the dermis beneath the vascular channels.
beneath the basement membrane of the overlying epithelium and separated by the rete ridges of the epithelium. These ridges result from down growth of the overlying epithelium and form epithelial strands and cords that separate the vascular channels, resulting in the multilocular, lobulated appearance. The overlying epithelium usually has some degree of acanthosis and papillomatosis, as well as hyperkeratosis. A mild, chronic inflammatory infiltrate may be seen in the dermis beneath the vascular channels.
ADJUNCTIVE STUDIES
A patient with multiple angiokeratomas on the vulva should receive consideration for screening for Fabry’s disease. This is accomplished by analysis of white blood cell α-galactosidase activity. If α-galactosidase activity is subnormal, the patient should be counseled concerning her heterozygous state for Fabry’s disease and family members should be screened appropriately.
CLINICAL BEHAVIOR AND TREATMENT
Treatment for angiokeratomas is warranted in symptomatic patients. Otherwise, they may be observed without intervention. The diagnosis should be confirmed by biopsy before ablative procedures are done, because nevi, melanocytic lesions, Kaposi’s sarcoma, and other neoplastic vascular lesions may also present as papular hyperpigmented lesions on the vulva. Excision is easily performed in the clinical setting. It is usually not necessary to take these patients to the operating room; however, multiple lesions requiring numerous incisions or laser ablation will require anesthesia in the operating room. Angiokeratomas tend to recur, and the patient should be forewarned of this. As they recur and become symptomatic, they may be removed individually in the office. Excisions do not need to be deep because these dermal vessels are not deeply seated. Bleeding is usually minimal with their removal. Skin may be left to heal by secondary intention with small lesions, or may be approximated with a single stitch of appropriate suture material after excising larger lesions.
PROGRESSIVE THERAPEUTIC OPTIONS
Progressive therapeutic options are as follows:
After biopsy confirms the diagnosis, asymptomatic lesions may be followed.
Symptomatic lesions may be excised. Multiple lesions may be treated with cryotherapy or with laser ablation.
DEFINITION
Molluscum contagiosum is a moderately infectious DNA pox virus infection that results in formation of papular, centrally umbilicated skin lesions. The incubation period is 14 to 50 days. The disease historically has been common in breast-feeding children, often presenting as perioral lesions secondary to infection from lesions on the mother’s breast. It is increasingly seen in vulvar clinic patients and immunosuppressed patients.
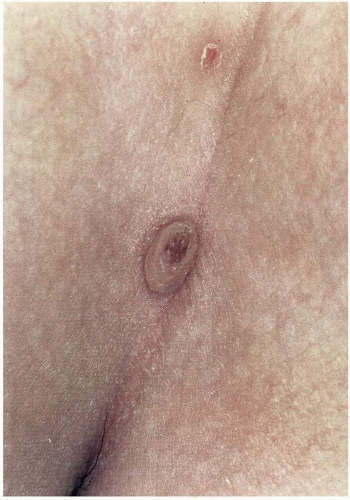
CLINICAL PRESENTATION
Many patients with molluscum contagiosum will be unaware of the vulvar or perianal lesions that have resulted from sexual contact or autoinoculation from sites distant from the vulva. The symptomatic patient will present for evaluation of small, smooth, papular lesions ranging in diameter from 3 to 6 mm. The papules typically have central umbilication, or punctum. The lesions are usually multiple, although isolated from each other. Rarely, a papule may be quite large and pedunculated, without central umbilication. Occasionally, they may be clustered and may form a plaquelike lesion composed of multiple (approaching 100) clustered lesions. The vulvar lesions are usually asymptomatic unless secondarily infected. They are commonly noted by the patient on self-examination. The patient may express concerns that she has a venereal disease such as condyloma acuminatum and will request evaluation and therapy.
DIAGNOSIS
The diagnosis is suspected immediately on observation of the classic lesion or lesions. Diagnosis does not require biopsy. Pressure on the papule will result in extravasation
of the central core, which is characteristic of molluscum contagiosum. Preparation of a cytologic smear, with fixation, and staining like a Pap test for microscopic examination is of value to demonstrate the diagnostic Henderson-Paterson bodies (molluscum bodies). Excision of the papule for histopathologic examination may be required if the diagnosis cannot otherwise be established, for example, a large, pedunculated papule that may resemble an acrochordon or nevus. Immunosuppressed patients may be at higher risk for acquiring this viral infection; therefore patients with molluscum contagiosum should be considered candidates for human immunodeficiency virus (HIV) testing.
of the central core, which is characteristic of molluscum contagiosum. Preparation of a cytologic smear, with fixation, and staining like a Pap test for microscopic examination is of value to demonstrate the diagnostic Henderson-Paterson bodies (molluscum bodies). Excision of the papule for histopathologic examination may be required if the diagnosis cannot otherwise be established, for example, a large, pedunculated papule that may resemble an acrochordon or nevus. Immunosuppressed patients may be at higher risk for acquiring this viral infection; therefore patients with molluscum contagiosum should be considered candidates for human immunodeficiency virus (HIV) testing.
MICROSCOPIC FINDINGS
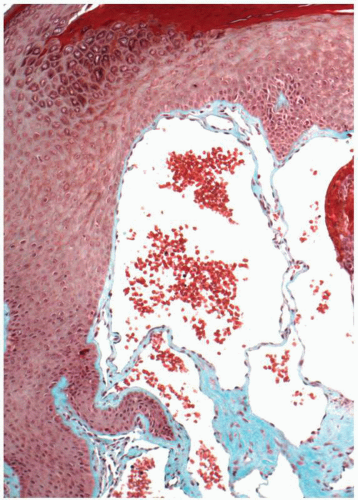
Histologic examination of a recent lesion will usually demonstrate marked acanthosis and the characteristic intracytoplasmic viral inclusions (Henderson-Paterson bodies). Over time the infected cell undergoes lysis. The central punctuation, related to this cellular lysis, is seen histologically if the lesion is bisected. Endothelial proliferation with perivascular inflammation may be present.
Biopsies are not usually obtained for molluscum contagiosum. Cytologic smears of the extruded contents of a molluscum lesion demonstrate epithelial cells with characteristic intracytoplasmic inclusions (molluscum bodies). The cytoplasmic inclusion is usually eosinophilic, but may be basophilic in older lesions. The virus-rich inclusions are released with death of the epithelial cell.
Cross-section of the lesion, at right angles to the epithelium and through the central surface dimple, demonstrates the lesion to be entirely intraepithelial with prominent acanthosis about the central core. The core holds the epithelial cells containing molluscum bodies. The core containing infected, degenerated keratinocytes communicates with the surface at the dimpled epithelium. An inflammatory cell infiltrate is present within the superficial dermis and usually extends perivascularly. Endothelial cell proliferation is evident in these involved areas.
ADJUNCTIVE STUDIES
Immunosuppressed patients may be at higher risk for acquiring this viral infection; therefore patients with extensive lesions of molluscum contagiosum should be considered candidates for testing for HIV.
THERAPY
Traditionally, molluscum contagiosum has been allowed to regress in young children without intervention. Lesions will frequently resolve, although the process may take several months. Most likely this approach has been secondary to a reluctance to perform painful evacuation of the papules in small children. Adults with molluscum contagiosum will be reluctant to follow a program of observation. As the name implies, the lesions are contagious and usually are managed easily by evacuation. The lesions may be curetted with either a small curette or the end of a needle (18 gauge). Local anesthesia is not typically required. Bleeding from the base of the lesion may be easily controlled with Monsel solution or silver nitrate. The patient should be forewarned of the potential for development for scarring and hyperpigmentation after evacuation and chemical cautery. Chemical destruction of papules may be accomplished with applications of trichloroacetic acid (TCA) at 1- to 2-week intervals. Alternatively, lesions may be destroyed with cryotherapy or liquid nitrogen application. Very fine applicator tips are required to minimize lateral tissue destruction.
Electrodesiccation is also an alternative; however, this will be painful. Laser therapy may be used, but extensive scarring may result in a less than optimal cosmetic result and the patient should be forewarned. Large pedunculated, atypical molluscum contagiosum lesions will require sharp excision under local anesthesia for diagnostic purposes and ultimately therapeutic success.
Electrodesiccation is also an alternative; however, this will be painful. Laser therapy may be used, but extensive scarring may result in a less than optimal cosmetic result and the patient should be forewarned. Large pedunculated, atypical molluscum contagiosum lesions will require sharp excision under local anesthesia for diagnostic purposes and ultimately therapeutic success.
PROGRESSIVE THERAPEUTIC OPTIONS
Progressive therapeutic options are as follows:
Evacuation by curettage and placement of chemical cauterizing agents to the base of the papule (silver nitrate or Monsel solution).
Trichloroacetic acid application at 1- to 2-week intervals.
Cryotherapy or liquid nitrogen application to the papule with fine-tipped applicators.
Laser therapy (forewarning patient of potential for scar formation).
Excision of large lesions for diagnosis and therapy.
 Figure 5.8. Irregular, variegated nevus in 20-year-old woman. Lesion was excised and histology was consistent with compound nevus. |
DEFINITION
Nevi are benign skin tumors formed by clusters of neural crest-derived benign nevus cells within the dermis and epidermis.
CLINICAL PRESENTATION
Nevi are found in the vast majority of the population but are not common on the vulvar skin.
CLINICAL PRESENTATION
Nevi observed at birth are termed congenital nevi and are found in approximately 10% of newborns. Such nevi are usually less than 4 mm in greatest horizontal dimension. Large congenital nevi, including giant melanocytic nevi (20 cm or larger in diameter) (garment type), are relatively rare, but do carry an increased risk of malignant melanoma in prepubertal individuals. Melanocytic nevi usually are not present at birth but develop over the ensuing years, frequently during adolescence. Sun-exposed areas of the body have a higher incidence of nevi.
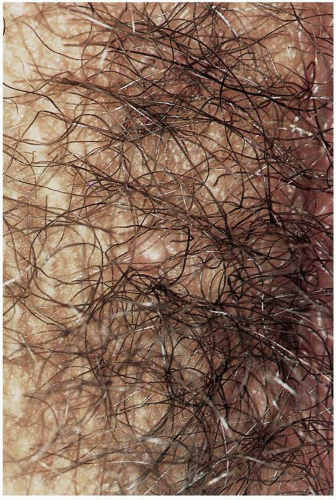
 Figure 5.9. Melanotic, homogenous nevus believed clinically to be a compound nevus. Histology was consistent with an intradermal nevus. |
Vulvar melanocytic nevi may be junctional, compound, or intradermal, and these three types occur with nearly equal distribution on the vulva. Vulvar nevomelanocytic nevi are usually well circumscribed, uniformly pigmented, and less than 10 mm in diameter. Most melanocytic nevi originate as junctional or flat nevi with minimal elevation above the surface skin. The contour is smooth and regular, and the margins are well demarcated. The color is uniformly a
shade of brown (ranging from tan to dark brown or black). Junctional nevi have nevus cells at the epidermal-dermal junction. As the nevus ages the nevus cells will migrate into the upper dermis; elevation of the overlying epithelium results in formation of a papular lesion. As with the junctional nevus, the compound nevus is demarcated with regular borders and the color is uniform. As this lesion ages, nevus cells will become predominantly located in the dermis, forming an intradermal nevus. The intradermal nevus may appear pedunculated or polypoid.
shade of brown (ranging from tan to dark brown or black). Junctional nevi have nevus cells at the epidermal-dermal junction. As the nevus ages the nevus cells will migrate into the upper dermis; elevation of the overlying epithelium results in formation of a papular lesion. As with the junctional nevus, the compound nevus is demarcated with regular borders and the color is uniform. As this lesion ages, nevus cells will become predominantly located in the dermis, forming an intradermal nevus. The intradermal nevus may appear pedunculated or polypoid.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree