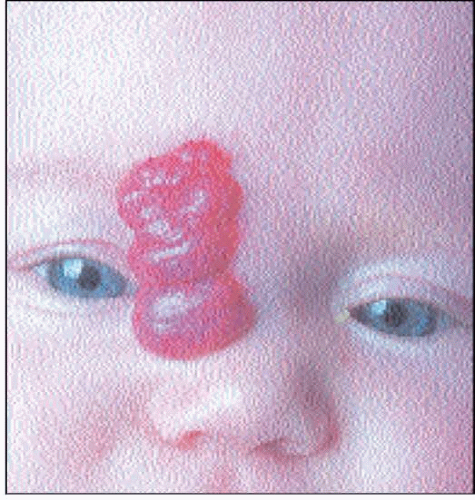
Infantile haemangiomas are benign vascular tumours which affect 1-2% of infants, most commonly on the head and neck. They are not present, or just visible at birth, and grow rapidly in the first 6 months of life to become distinctive bright red nodules, sometimes with a deeper component (
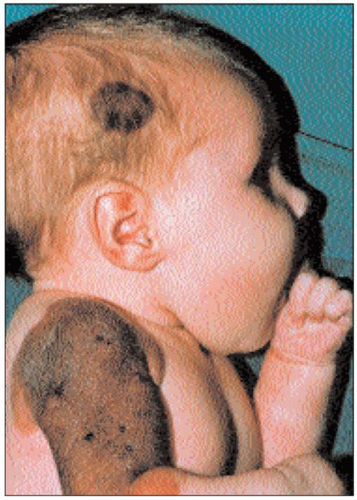
2.1). At around 12 months of age, they start to undergo spontaneous resolution (
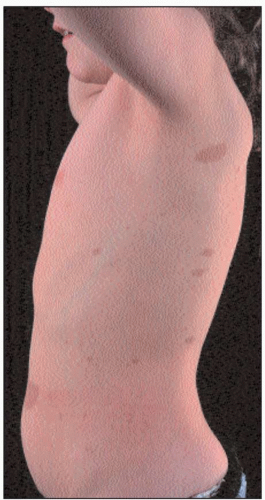
2.2). Fifty per cent of lesions will disappear by 5 years of age and 90% by 9 years. There may be residual flaccid skin and telangiectasia. Complications of ulceration (
2.3), haemorrhage, and interference with function may occur during the phase of rapid proliferation. Rarely, multiple haemangiomas occur, which may be associated with internal haemangiomas. Very infrequently, large haemangiomas may be associated with structural brain and cardiac abnormalities, or consumptive coagulopathy.