50. Otoplasty
Joseph M. Brown, Jeffrey E. Janis, Charles H. Thorne
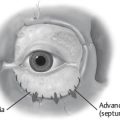
NORMAL EAR ANATOMY AND DEVELOPMENT1–5 (Fig. 50-1)
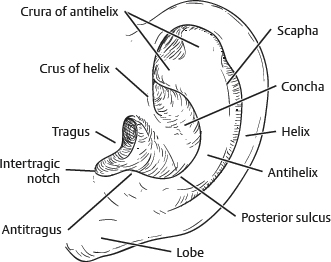
Fig. 50-1 Anatomy of the external ear.
■ Lateral skin (scapha) is adherent and thin with little subcutaneous tissue.
■ Medial skin is loose, fibrofatty, and thick.
■ The ear is 85% of its adult size by the sixth year of life.
■ Average length of 10-year-old male ear is 60 mm.
■ Ear cartilage becomes stiffer and more brittle with age.
■ Neonatal cartilage is malleable and softer.
TIP: Good outcomes have been achieved by molding techniques if implemented within the first few weeks of life while circulating maternal hormones remain elevated.
EMBRYOLOGY
Ear begins to protrude approximately 3-4 months of gestation.
VASCULARITY (Fig. 50-2)
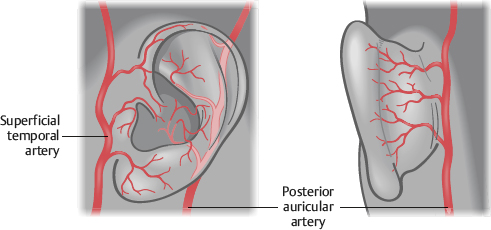
Fig. 50-2 Vascularity of the external ear.
■ External carotid gives off two terminal branches to the ear:
• Posterior auricular artery
• Superficial temporal artery
INNERVATION
■ Auriculotemporal nerve (CN V)
• Innervates tragus and crus helicis
■ Great auricular nerve (C2-3)
• Divides into anterior and posterior branches
• Innervates remaining scapha and lobule
■ Arnold nerve (CN X)
• External acoustic meatus and medial conchal bowl
■ Lesser occipital nerve (C2-3)
CARTILAGINOUS ANATOMY (Fig. 50-3)
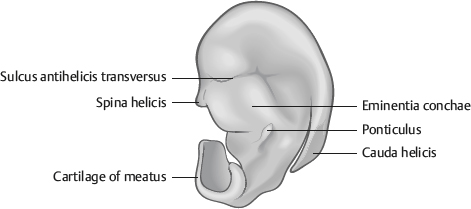
Fig. 50-3 Cartilaginous anatomy (posterior view).
■ Posterior surface has two important landmarks:
• Ponticulus is the site of attachment to the auricularis posterior muscle.
• Must be dissected and removed before conchamastoid sutures (Furnas technique)
• Cauda helicis serves as possible transition point from posterior dissection to an anterior dissection in the subperichondrial plane without violating the lateral skin envelope.
NORMAL PROPORTIONS OF THE AESTHETIC EAR4,6 (Fig. 50-4)
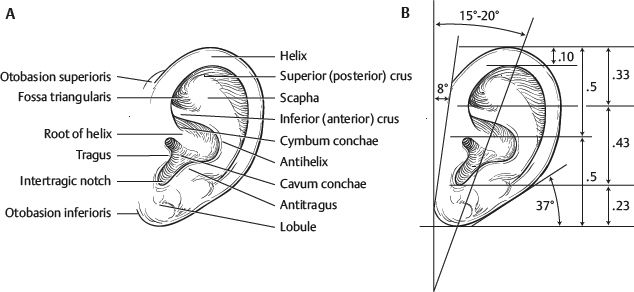
Fig. 50-4 Proportions of the ear. A, The normal ear and its parts. B, The ear’s critical proportions.
■ The long axis of the ear inclines posteriorly approximately 20 degrees from vertical.
■ The ear axis does not normally parallel the bridge of the nose.
• Usually a 150 degrees differential
■ The ear is positioned approximately one ear length (5.5-7 cm) posterior to the lateral orbital rim between horizontal planes that intersect the eyebrow and columella.
■ The width is approximately 50%-60% of the length.
• Width 3-4.5 cm
• Length 5.5-7 cm
■ The anterolateral aspect of the helix protrudes at a 21-30 degree angle from the scalp.
■ The anterolateral aspect of the helix is approximately 1.5-2 cm from the scalp.
• There is a large amount of racial and gender variation.
■ The lobule and antihelical fold lie in a parallel plane at an acute angle to the mastoid process.
■ The helix should project 2-5 mm more laterally than the antihelix in frontal view.
EPIDEMIOLOGY/PATHOLOGY6–9
■ Autosomal dominant trait
■ Incidence in whites is about 5%.
■ Three major contributing factors to the abnormal morphology:
1. Underdeveloped antihelical fold
► Obtuse conchoscaphal angle (>90 degrees)
► Scapha and helical rim protrude causing prominent upper and middle third of ear.
2. Prominent concha
► Either excessively deep conchal wall (>1.5 cm)10 or obtuse conchamastoid angle
► Causes prominent middle third of ear
3. Protruding earlobe
► Causes prominent lower third of the ear
■ Multiple studies5,6,11,12 indicate protruding ears may lead to teasing and bullying that can result in emotional and behavioral problems in the long term.
■ Recent literature emphasize that, performed in the correct patients, otoplasty can positively affect patients’ self-esteem, psychological well-being, and quality of life.
GOALS OF SURGICAL TREATMENT9
■ All upper-third ear protrusion must be corrected.
■ The helix of both ears should be visible beyond (lateral to) the antihelix from an anterior view.
■ The helix should have a smooth and regular contour along its course.
■ When viewed from behind, the contour of the helical rim should be a straight line.
■ The postauricular sulcus should not be markedly decreased or distorted.
■ The helix-to-mastoid distance should be in the normal range of 10-12 mm in the upper third, 16-18 mm in the middle third, and 20-22 mm in the lower third.
■ The position of the lateral ear border to the head should match within 3 mm at any point between the two ears.
PREOPERATIVE EVALUATION13
■ A thorough history should be obtained.
• The history should include the motivations and desires of the patient, as well as any indication of psychological stress.
■ Examination should focus on the following:
• Degree of antihelical folding
• Depth of the conchal bowl
• Plane of the lobule and deformity, if present
• Angle between the helical rim and the mastoid plane
• Quality and spring of the auricular cartilage
► To assess likelihood of necessity of cartilage scoring
SENIOR AUTHOR TIP: First question: Are the protruding ears of normal shape or are they protruding AND of abnormal shape (e.g., constricted ear, Stahl ear).
■ Preoperative photographs should be obtained. Spira14 recommended taking two frontals, right and left lateral views, and a modified worm’s-eye view.
• Two frontal views help to accommodate the patient’s blink reflex.
• Worm’s-eye view helps to determine the degree of the deformity that may otherwise be masked by lighting/shadows.
SENIOR AUTHOR TIP: I think the posterior view is critical and perhaps more important than some of the views mentioned previously.
INDICATIONS/CONTRAINDICATIONS
■ Contraindications
• Surgical intervention should not be performed before patients are 4 years of age. In the neonatal period, nonoperative management can be very effective, as elevated circulating estrogen levels keep auricular cartilage malleable and responsive to molding casts.
■ The ear is nearly fully developed by 6-7 years of age, at which time surgery should be considered in appropriate candidates.
NOTE: However, it is important to address timing of surgery on a patient-to-patient basis, because some patients may experience significant bullying at an even younger age, and earlier intervention may be necessary.
• Balogh and Millesi15 have shown that auricular growth was not halted after a 7-year mean follow-up in 76 patients who underwent cartilage excision otoplasty for prominent ears.
• Patients with prominent ears generally do not care if a little growth inhibition results from the surgery.
INFORMED CONSENT
■ Addressing specific concerns for each patient and setting appropriate expectations are essential.
■ Although the goal of this surgery is to improve self-image through correction of the deformity, it does not guarantee a “better life.”
■ Risks include undercorrection, overcorrection, unnatural or sharp contours, hematoma, infection, chondritis, recurrent deformity (early and/or late), persistent asymmetry with the contralateral ear, and protrusion of permanent sutures through the medial skin.
EQUIPMENT
■ A Dingman otoabrader or half of an Adson-Brown Tissue forceps may be used for cartilage scoring.
■ Aside from this, no special equipment is required for this surgery.
■ Methylene blue is a useful tool for transposing landmarks on the anterolateral surface of the ear to the cranial surface through the use with a 25-gauge needle.
SURGICAL TECHNIQUES
■ Most common
• Mustardé16: Cartilage shaping
• Furnas17: Cartilage shaping
• Converse–Wood-Smith18: Cartilage breaking
■ Others
• Stenstroem19: Cartilage scoring
• Chongchet20: Cartilage scoring
NOTE: Cartilage-scoring techniques are based on the observation that cartilage curls away from a cut surface because of release of “interlocked stresses” when the perichondrium and outermost layer of chondrocytes are incised.21,22
TIP: Even when performing a unilateral otoplasty, draping both ears into the field for intraoperative assessment for symmetry is encouraged. To prevent asymmetry after the procedure, performing an otoplasty on both ears should be considered, even if only one appears particularly prominent.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree