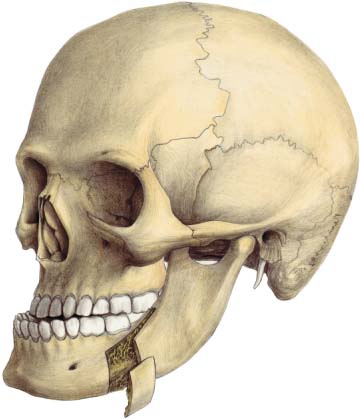
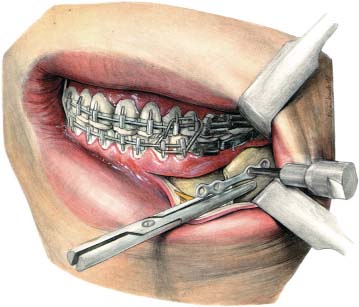
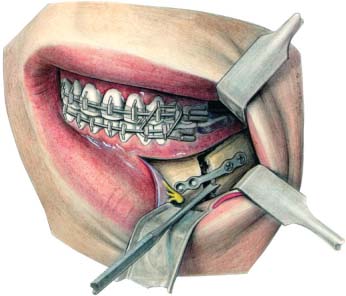
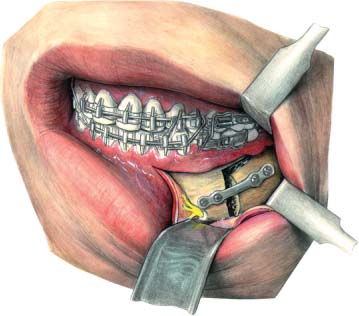
22 Osteotomies of the Mandible The sagittal split osteotomy described by Obwegeser (Trauner and Obwegeser, 1957) is probably the most frequently used osteotomy to correct mandibular anomalies including hypoplasia, hyperplasia, and asymmetries. Miniplates can be used to stabilize these osteotomies, allowing for early release of, or even no, intermaxillary fixation. Studies have proven that the stability achieved, in advancement as well as setback cases, is adequate and highly predictable (Borstlap et al., 2004, 2005). The advantages of using plates as compared with positional or lag screws can be summarized as follows: • Plates can be bent to adapt to the anatomical situation caused by the positional changes of the fragments; excessive, unwanted torquing, particularly of the proximal fragments, can thus be avoided. • Extraoral stab incisions are not necessary when using miniplate fixation. • Damage to the inferior alveolar nerve can be minimized because the nerve cannot be injured by the screws; since the fragments are not pulled together by screws, the nerve cannot be damaged by compression either. • If, after the patient is awake and sitting up in a natural position, the occlusion is found to be inadequate because of a changed position of the distal fragment, the plates may be adjusted without a further general anesthetic. The procedure can be done under local anesthesia, several days after the first operation, when the swelling has subsided. Adjustment usually only includes repositioning of the screws in the distal fragment, after fine adjustment of the occlusion with temporary intermaxillary fixation. Disadvantages include the following: • The bone cuts have to be brought relatively further forward to allow for easy application of the plates; this may increase the risk of buccal plate fractures (bad splits). • Ischemic necrosis of parts of the buccal plate around the screws is sometimes seen. This gives rise to an inflammatory reaction but does not usually interfere with overall bone-healing. The sagittal split osteotomy (Trauner and Obwegeser, 1957) is performed using the modifications of Dal-Pont (1961), Hunsuck (1968) and Epker (1977). The anterior vertical cut is situated approximately between the first and the second molar. Following placement of an acrylic splint and intermaxillary fixation, the proximal fragment has to be positioned with a gauze-packing instrument. In cases of setback of the distal fragment, the appropriate amount of bone to be cut from the proximal segment can now be calculated (Fig. 22.1). An appropriate miniplate is selected, long enough to include two holes in the proximal and distal segment. The plate is bent to lie passively against the bone fragments. A straight Kocher clamp is then applied to the proximal segment and the segment is rotated anteriorly and superiorly. A hole in the proximal segment is drilled and the plate screwed in position using a 5-mm or 7-mm screw (Fig. 22.2). Plate position may now be checked and adjustments can be made. Following this, a second hole is made while the proximal fragment is again pulled forward and slightly rotated upward. The second screw is then placed and tightened. Next, the gauze-packing instrument is used to push the proximal fragment into its proper position, taking care to correctly align the lower margin in relation to the distal segment (Fig. 22.3). Holes are drilled in the distal segment and screws placed and tightened (Fig. 22.4). A similar procedure is performed on the other side, after which the intermaxillary fixation is released. The occlusion can now be checked by manually manipulating the chin with the condyles seated in their fossae. If an error is noted, intermaxillary fixation can be reapplied and the plates readjusted, which involves repositioning the distal screws only. Fig. 22.1 Buccal cortical fragment to be removed to allow the mandible to be set back. Fig. 22.2 The first screw is inserted. At this stage the proximal fragment may be placed in its proper position, to check plate alignment. Fig. 22.3 A gauze-packing instrument is used to hold the proximal fragment in position while screws are inserted in the distal fragment. Fig. 22.4 The screws have been inserted in the proximal fragment and the distal fragment is in place. In Angle class II cases the osteotomy is performed using the same technique as in Angle class III patients. After osteotomy the mandible is positioned forward and the cortical bone gap is bridged with a four-hole or six-hole miniplate (Figs. 22.5, 22.6). If the buccal plate is inadvertently fractured while splitting the mandible (bad split), the loose fragment can be fixed to the proximal fragment using a miniplate. In these circumstances it is best to complete the splitting first. The proximal fragment can then be mobilized and pulled forward to allow the miniplate to be fixed (Fig. 22.7). The fixed fragment can thus be used for fixation of the osteotomy site, but clearly this type of fixation cannot be described as rigid. A period of intermaxillary fixation of at least 4 weeks is recommended for such patients. The vertical ramus osteotomy has frequently been used in the past for the correction of mandibular hyperplasia (Robinson, 1956). The application of an intraoral vertical ramus osteotomy, however, almost precludes the use of rigid fixation, including miniplates, because of lack of access and the risk of damage to the inferior alveolar nerve.
Sagittal Split Osteotomy
Introduction
Technique
Vertical Ramus Osteotomy
Introduction
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree