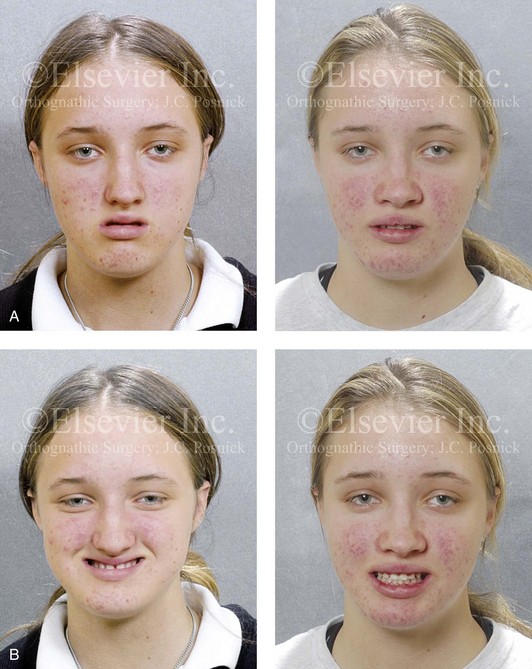
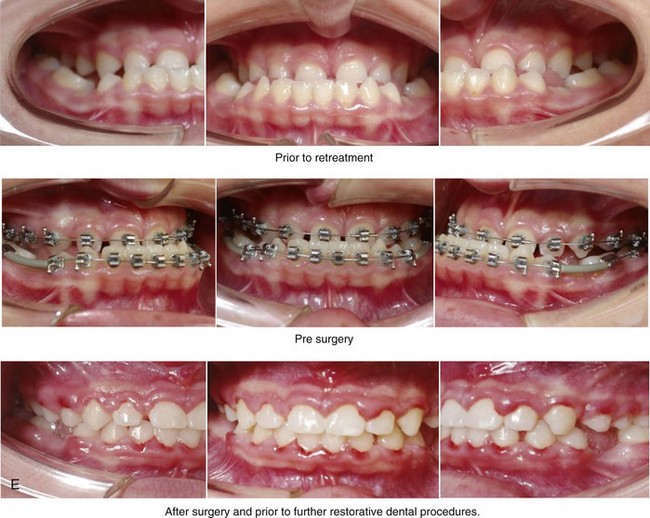
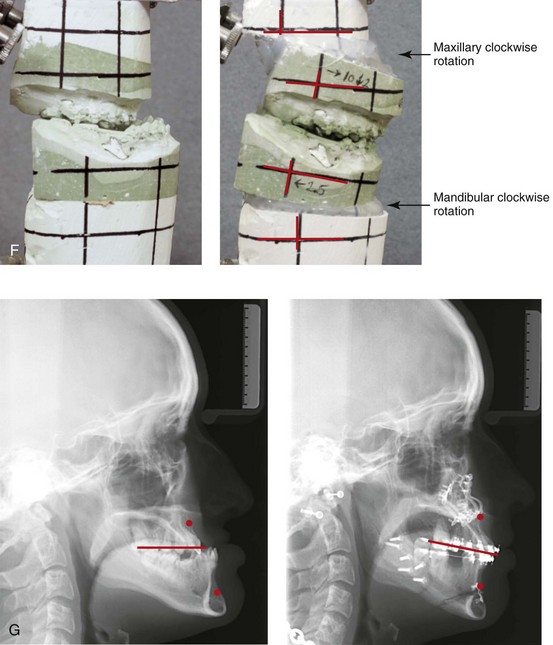
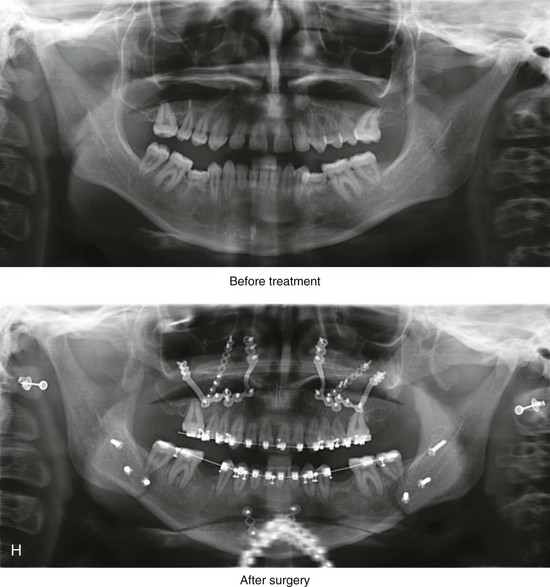
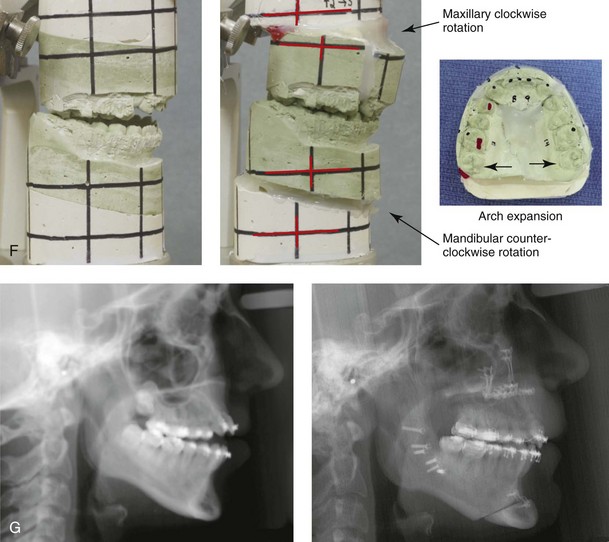
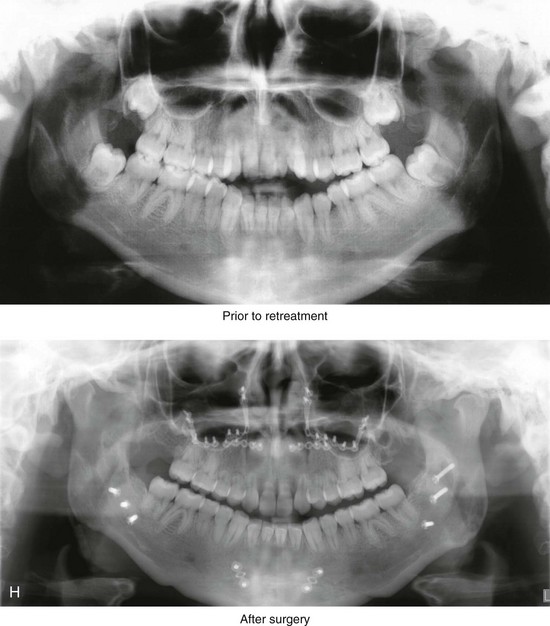
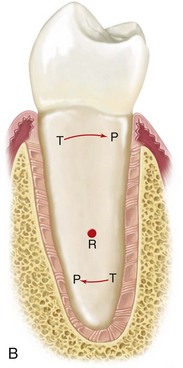
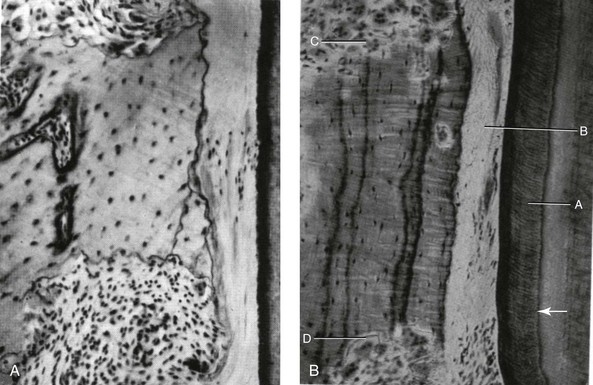
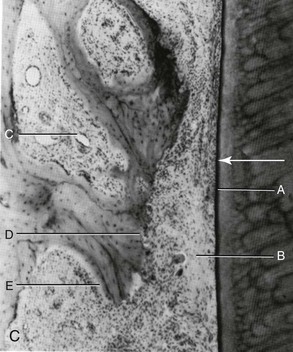
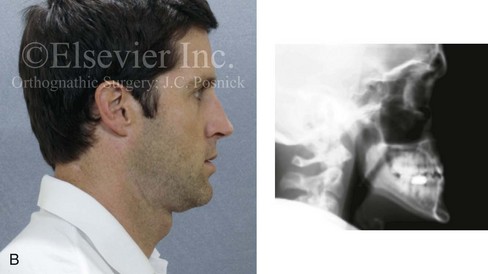
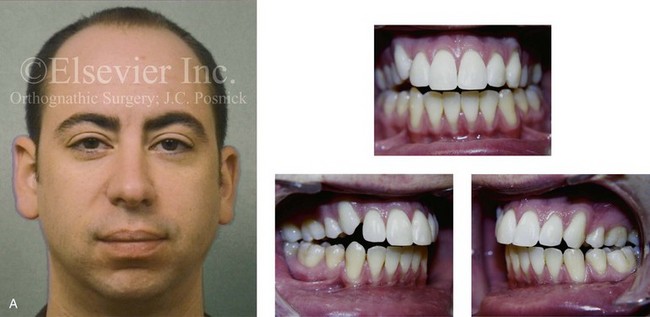
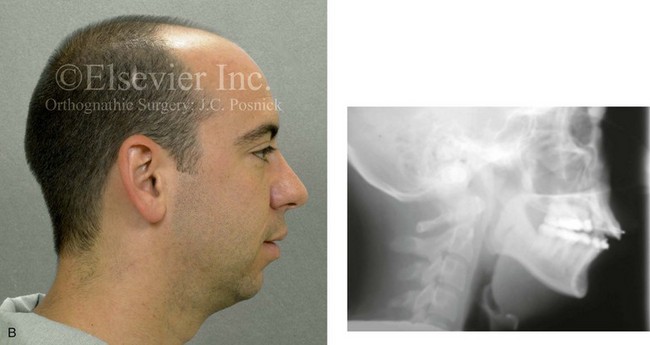
5 Current issues in orthodontic therapy are, for the most part, no longer just a matter of what attachments or mechanical approaches to use.* Contemporary orthodontics focuses on accurate diagnosis and a basic philosophy of treatment to enhance facial aesthetics and to correct dysfunction. The role of orthognathic surgical interventions and coordinated comprehensive dental rehabilitation to achieve the most favorable outcome should always be considered.110 Malocclusions result from a combination of environmental influences and the patient’s morphogenetic hereditary predisposition (see Chapter 4).1,11,15,18,43,44 The dental alignment that naturally occurs in each individual is greatly influenced by the baseline jaw relationships as well as by his or her daily postural masticatory and airway function.† In the presence of a dentofacial deformity, the mere orthodontic movement of the teeth into a “better” interdigitation will not establish normal jaw relationships nor will it correct the head and neck dysfunctions that contribute to or result from the malocclusion.147,157,179–181 The observed crowding of the teeth generally reflects nature’s attempt to establish a homeostatic balance among the available space in the alveolus, the size of the teeth and the dental roots, the position and size of the jaws, and the constant molding and balancing effects of the masticatory and facial musculature with regard to daily function.6,146,147,162–165,182,183 Currently, there are a plethora of appliances than can accomplish almost any desired change in the alignment of the teeth.69,72 From a purely mechanical perspective, orthodontists are trained in the techniques of tooth movement with the goals of improving dental alignment in each jaw and achieving “ideal” occlusion between the upper and lower arches. The orthodontic movement of the teeth is based on the principle that, if prolonged pressure is applied to a tooth, movement will occur as the bone around the tooth remodels. This is primarily a periodontal ligament phenomenon. In the process, bone is selectively resorbed in some areas and deposited in others. The bone that surrounds the tooth responds to the applied force through intermediate structures (periodontal ligaments), and the objective is for the tooth to move without the loss of crestal height or cortical plates while carrying its attachment apparatus along with it. The whole socket must migrate along with the tooth during this process. When orthodontic therapy is used to move teeth outside of a biologic envelope, extended treatment time, the potential for periodontal sequelae, and a less-than-ideal long-term occlusion are the likely consequences.70,86,178 These may occur as a result of the following: (1) attempts to further compensate the position of the teeth toward the skeletal disharmony and outside of the alveolar housing; (2) dental (root) crowding within limited available alveolar bone; or (3) ongoing nasal airway obstruction with an open mouth posture and inadequate lip coverage of the incisors.4,8,9,32,73,85,193 Unless ankylosis is present, each tooth is connected to and separated from the adjacent alveolar bone by a specialized collagen supporting structure known as the periodontal ligament (PDL) (Fig. 5-1). The PDL normally occupies a space of approximately 0.5 mm around all parts of the tooth root. The PDL is comprised of a network of parallel collagenous fibers that insert into the cementum (i.e., the covering of the root surface of each tooth) and then into a dense bony plate (radiographically, this is called the lamina dura) that is adjacent to each tooth within the alveolar bone. These supporting PDL fibers are angulated between the root of the tooth and adjacent bone; they attach apically on the root and extend occlusally to the adjacent bone. Biomechanically, these angulated PDL fibers act as shock absorbers by helping to resist forces that are applied to the tooth during normal chewing function. Figure 5-1 A, Principal fiber bundles of the periodontal ligament on the facial surface of a mandibular premolar (silver stain). B, Distribution of faciolingual forces (arrows) around the axis of rotation (R) in a mandibular premolar. The periodontal ligament fibers are compressed in areas of pressure (P) and taut in areas of tension (T). Part A from Glickman I: Clinical periodontology, ed 4, Philadelphia, 1972, W.B. Saunders Company, Figures 2-3 and 2-8, pp 34 and 38, respectively. Within the periodontal ligament space, there are cellular elements (i.e., mesenchymal cells, nerve endings, and vessels) and interstitial fluid. The primary cellular elements (i.e., mesenchymal cells) are thought to differentiate to form the fibrocytes and the osteocytes. The collagenous elements of the PDL are constantly being renewed and altered, depending on the level of functional stress that they are undergoing. The remodeling and recontouring of the alveolar bone is a necessary component of orthodontic tooth movement, and it is dependent on specialized cells (Fig. 5-2). As part of the remodeling process, bone is removed by osteoclasts that are thought to be derived from the mesenchymal cells. Cementum is removed by specialized cementoclasts, which are also derived from mesenchymal cells. Nerve endings attach to the PDL and to the blood vessels that surround them. The nerve endings are effective for proprioception and for the perception of pain. The interstitial fluid found within the PDL space is derived from the vascular network. It serves as a nutrient source, and it contributes to the shock-absorbing mechanism to better withstand the physiologic forces as well as any pathologic forces that are applied directly to the teeth. Figure 5-2 A, Undermining resorption in a 12-year-old child. This is a view from a short-rooted premolar tooth. The cementum that covers the root surface has not been broken, although the periodontal membrane is hyalinized at the area of greatest pressure. A spicule of bone is being attacked from above and below, away from the compressed PDM. B, Undermining resorption is taking place in a 39-year-old adult. No osteoclastic activity occurs in the compressed PDM, but osteoclasts are at work on bundle bone that has been laid down previously from above and below the area of greatest pressure. A, Thick cementum layer. B, Hyalinized periodontal ligament. C and D, Frontal undermining bone resorption on both sides of the cell-free area. C, Tooth movement with light forces. This image shows the pressure side during the period shortly after hyalinization. A, Root surface. B, Remnants of cell-free, formerly hyalinized tissue. C, Large marrow space in alveolar bone. D, Direct bone resorption. E, Compensatory bone formation in the marrow space as a response to bone resorption on the side of the periodontal ligament. A courtesy K. Reitan from Graber TM: Orthodontics: principles and practice, ed 3, Philadelphia, 1972, W.B. Saunders Company, Figure 10-5, p 496. B courtesy K. Reitan from Graber TM: Orthodontics: principles and practice, ed 3, Philadelphia, 1972, W.B. Saunders Company, Figure 10-5, p 496. C courtesy K. Reitan from Graber TM: Orthodontics: principles and practice, ed 3, Philadelphia, 1972, W.B. Saunders Company, Figure 10-6, p 497. During normal chewing function, the teeth are subjected to intermittent forces that are then transmitted to the periodontal structures.55,88,89,92,118,192,209 When forces are applied to a tooth, the load is dissipated by the periodontal ligament and the interstitial fluid within the tooth socket. These mechanisms allow a more limited force to then be transmitted to the cortical bone that surrounds the tooth socket (i.e., the lamina dura), which “bends” in response. The term bending is used to describe the physiologic response to normal masticatory forces. The bone bending that occurs in response to normal (chewing) function is thought to be an important stimulus to osseous regeneration and repair. This intermittent but repetitive stress loading allows for the modification of the bony architecture as an adaptation to functional demands. If pressure against the tooth is maintained (as opposed to being intermittent, as when chewing), the interstitial fluid within the tooth socket is expressed (i.e., pushed out) and the tooth itself is displaced, thereby compressing the PDL directly against the adjacent bone. This is perceived by the individual as being quite painful, and, if the force is excessive and prolonged, a different physiologic response occurs. This “trauma from occlusion” is a response in which the remodeling of the adjacent compressed bone occurs. A definition of the term traumatic occlusion was first provided by Stillman in 1917. He stated that traumatic occlusion is “a condition where injury results to the supporting structures of the teeth by the act of bringing the jaws into closed contacts.”171 The definition given by the American Association of Periodontics in 1986 is “an injury to the attachment apparatus as a result of excessive occlusal force.”171 Primary occlusal trauma involves excessive forces on a normal periodontium, and secondary occlusal trauma is considered to have occurred when normal forces are placed on a compromised periodontium (see Chapter 6). The intentional application of these principles is how controlled orthodontic tooth movement occurs. The application of light prolonged vector-controlled forces allows for more or less predictable man-made movements of the teeth. Interestingly, nature’s application of these light prolonged forces on the teeth can also occur from maintained posturing of the muscles of the lips, cheeks, and tongue as they press against the teeth, thereby causing dental movement and remodeling of the alveolar ridge. When postural forces from the lip, cheek, or tongue are pathologic, they may contribute to the classic dental compensations that are seen with each specific pattern of developmental dentofacial deformity.* These environmental forces may then be compounded by iatrogenic orthodontic dental compensation maneuvers to further affect periodontal health. For example, consider the retroclination of the lower anterior teeth that is seen with Class III skeletal patterns (Fig. 5-3) (see Chapter 20) or the proclination of the lower incisors that is seen with skeletal Class II cases (Fig. 5-4) (see Chapter 19). In both instances, negative periodontal sequelae may occur. Figure 5-3 A 34-year-old man arrived for the evaluation of a long-standing jaw deformity with malocclusion, chronic obstructive nasal breathing, and periodontal issues. Since his early childhood years, he was known to have a maxillary deficiency with a relative mandibular excess growth pattern. The family elected a camouflage orthodontic approach that included four bicuspid extractions and the introduction of dental compensation in an attempt to neutralize the occlusion when he was 10 to 15 years old. He was a forced mouth breather as a result of the associated increased nasal airway resistance. He underwent septoplasty when he was 20 years old, but this did not result in significant improvement. His general dentist confirmed labial bone loss and gingival recession of the mandibular anterior and maxillary posterior dentition. He was referred to this surgeon, and a comprehensive orthognathic and dental rehabilitation approach was recommended. Consultations with a periodontist, an orthodontist, and an ear, nose, and throat specialist were carried out. The patient was confirmed to have residual deviation of the septum and enlarged inferior turbinates, which explained the continued difficulty that he had with breathing through his nose. A degree of root resorption of the anterior dentition was confirmed. The need for gingival grafting to attain improved root coverage and to generate a wider band of attachment was recommended (i.e., teeth nos. 3, 11, 14, 19, 20, 23 through 26, 29, and 30). This will be followed by the orthodontic removal of dental compensation and then orthognathic and intranasal procedures to improve long-term dental health, to enhance facial aesthetics, and to open the upper airway. A, Frontal facial and occlusal views before retreatment. B, Profile facial view and lateral cephalometric radiograph before retreatment. C, Panorex radiograph with retreatment in progress. Figure 5-4 A man in his early twenties with a primary mandibular deficiency growth pattern. During his teenage years, he underwent failed growth modification attempts followed by orthodontic camouflage maneuvers that included four bicuspid extractions in an attempt to neutralize the occlusion. Deterioration of the periodontium with labial bone loss and gingiva recession along the mandibular anterior dentition is evident. The patient was referred to this surgeon, and a comprehensive orthognathic and dental rehabilitation approach was approved. A, Frontal facial and occlusal views before retreatment. B, Profile facial view and lateral cephalometric radiograph before retreatment. The specific anatomic response to orthodontic forces is dependent on the force magnitude. “Heavy” forces often result in pain, necrosis of cellular elements within the PDL (i.e., hyalinization), and remodeling with the resorption of the alveolar bone that is being compressed (i.e., the hyalinization zone). It may also result in the resorption of the root apex, remodeling with the loss of crestal bone, and fenestrations or dehiscence through the cortical plates. When light and constant forces are applied to the tooth, there is compression without necrosis of the PDL elements and remodeling of the tooth socket without significant irreversible necrosis. As long as the tooth is being moved into adequate alveolar bone and the forces are light, the root of the tooth is less likely to resorb, and the alveolar crest height and cortical plates are for the most part preserved.30 The objective of the orthodontic movement of a tooth is to produce the desired new tooth position as quickly as can be done, with as little damage as possible to the tooth, the PDL, the alveolar bone, and the adjacent teeth. The heavier the sustained pressure, the greater the reduction in blood flow where compression is occurring in the PDL.25,166,174 When only light prolonged force is applied to a tooth, the partially compressed PDL experiences diminished blood flow, and the interstitial fluids are expressed (pushed out) from the PDL space as the tooth moves within the socket.125 Animal experiments confirm that, within a few hours, there will be increased levels of cyclic adenosine monophosphate (cAMP).175 cAMP is known for its importance in the alteration of cell functions. Within 4 hours of continued sustained low pressure, mesenchymal cell differentiation occurs. From a clinical perspective, it is known that, if orthodontic appliances are used for less than 4 to 6 hours per day, not enough sustained force will be applied, and little or no tooth movement will occur.143,148 It is known that the osteoclasts attack the compressed area of lamina dura to remove bone.184 The radiographic appearance of a widened PDL (on the tension side) in the presence of light prolonged orthodontic forces indicates that tooth movement is soon to begin.66 On the compression side, osteoclasts are removing the lamina dura. On the tension side, remodeling activity involves osteoblasts laying down new bone. The course of events is different if the prolonged force applied to the tooth is too great. If the force transmitted to the periodontal ligament totally occludes the blood vessels, thereby cutting off all blood supply to the area, generalized necrosis occurs within the compressed area. Although some avascular areas in the PDL will occur even with light forces, if the predominant forces are “heavy,” then the response is necrosis. Irreversible damage can then occur, and this includes remodeling with the loss of crestal bone, root resorption, and cortical plate dehiscence. The histologic findings within the PDL—even with light forces during the compression process—show the disappearance of cells within the vessels. The histologic appearance is descriptively said to be “hyalinized” because of its visual resemblance to hyaline connective tissue. After this hyalinization process begins, after several days of delay, the remodeling of bone that borders the sporadic necrotic areas of the PDL will occur as osteoclasts (derived from adjacent undamaged areas) arrive and do their work. The process of bone removal is called undermining resorption. This term is visually descriptive when it is viewed under the microscope, because the attack by the osteoclasts is from the underside of the lamina dura. After the hyalinization (i.e., the compression of blood flow with isolated necrosis) and the undermining resorption (i.e., the osteoclastic activity on the underside of the lamina dura) have “softened” the lamina dura, tooth movement is soon to occur. The chronology of tooth movement with frontal resorption is different than that of undermining resorption. With frontal resorption, a steady attack on the outer surface of the lamina dura results in smooth, continuous tooth movement. With undermining resorption, there will be a delay in the removal of the bone adjacent to the tooth. When heavy force (i.e., pressure) is again reinitiated, there will be a similar delay in tooth movement until a second round of undermining resorption can occur.171 The orthodontic movement of a tooth is clinically more efficient when there are only minimal areas of PDL necrosis. As a result, only limited levels of pain are experienced by the individual undergoing treatment. Unfortunately, neither aspect is completely avoidable. To date, a completely smooth progression of tooth movement with consistent light force over time has proven to be unattainable within the human biologic system. One important compounding factor is that the individual who is undergoing orthodontic tooth movement must also continue with the everyday functions of mastication, speech, swallowing, and breathing within a 24-hour cycle. These functions also place forces on the teeth, which may either conflict with or expedite the applied orthodontic forces. Another factor is the relative ineffectiveness of the appliances (i.e., the materials) used to apply sustained appropriate levels of force. To review, in clinical orthodontic practice, on one end of the spectrum, too much sustained force is detrimental to the tissues; alternatively, too little force will not produce the tooth movement that is desired.25 The bisphosphonates act as inhibitors of osteoclast-mediated bone resorption, which by definition have an effect on bone remodeling.5,102 There is evidence to suggest that tooth movement in patients who are receiving parenteral bisphosphonate therapy may be retarded, with a subsequent risk for osteonecrosis of the jaws.113 Bartzela and colleagues conducted a systematic review of the literature regarding the effects of medications and dietary supplements on the rate of experimental orthodontic tooth movement.23 The results of their literature search indicated the following: • The therapeutic administration of eicosanoids results in increased tooth movement. • Nonsteroidal anti-inflammatory drugs decreased tooth movement; however, non-nonsteroidal anti-inflammatory analgesics (e.g., Paracetamol [acetaminophen]) had no effect. • Corticosteroid hormones, parathyroid hormone, and thyroxin have all been shown to increase tooth movement. • Estrogens probably reduce tooth movement, although no direct evidence is available. • Vitamin D3 stimulates tooth movement, and dietary calcium seems to reduce it. The term anchorage as it applies to orthodontics refers to the nature and degree of resistance to displacement provided by an anatomic unit (e.g., molars and premolars, temporary skeletal anchorage devices, hard palate) when it is used for the purpose of effecting tooth movement.139 When planning orthodontic therapy, the clinician must consider not just the tooth movement that is desired but any reciprocal effects that may occur throughout the dental arches as well. Reciprocal effects must be controlled to achieve the desired repositioning of all of the teeth and to establish preferred occlusion. In a completely reciprocal situation, Newton’s theory is easy to understand. When the forces applied to similar teeth and to similar arch segments are equal, there will be an equal force distribution in each PDL with this same degree of movement. A classic clinical case analysis that is frequently used to understand the “reciprocal/nonreciprocal” concept is to consider the type of tooth movement that occurs when an elastomeric chain is placed across a first premolar extraction site in the maxilla. This pits the central incisor, the lateral incisor, and the canine in the anterior segment in opposition to the second premolar and the first molar in the posterior segment. The same total force would be felt by the three anterior teeth and the two posterior teeth as the action of the chain is equal in each segment. However, equal reciprocal movement would require the same total PDL surface area over which the force is distributed. Because the measured PDL area for the two posterior teeth is larger than the three anterior teeth, the movement will not be reciprocal. In this typical, real-life clinical setting, the anterior teeth move back into the bicuspid extraction sites more than the posterior teeth migrate forward. If it is desired that the anterior teeth move entirely into the extraction space, reinforced anchorage will be required. This may be accomplished by incorporating the second molar into the posterior unit. This changes the root surface area ratios, which results in additional retraction of the anterior teeth. Other methods of reinforcing posterior anchorage include the use of extra oral force, such as headgear, TADs, and palatal support through the use of Nance appliances or a transpalatal bar.148 Cortical bone is more resistant to resorption; therefore, tooth movement is slowed whenever the root to be moved contacts it. This can be problematic, for example, when there is a dense cortical layer of bone formed within the alveolar process of a previously (long-ago) extracted tooth. It can be more difficult to close an “old” extraction site, because tooth movement is slowed to a minimum when the root encounters cortical bone along the resorbing side of the alveolar ridge.118,126 Tooth movement is also greatly slowed and root resorption more likely when a tooth (or tooth root) is forced against a cortical plate (e.g., a labial plate, a lingual plate), such as may occur during attempts to correct incisor inclination. In theory, the optimal force level for the orthodontic movement of a tooth is the lightest force (and the resulting pressure) needed to produce the near-maximum preferred response.176 Forces that are more than “optimal”—although effective for the production of tooth movement—are both unnecessary and possibly traumatic to the tooth, the periodontium, the alveolar ridge height, and the cortical plates. Recent research indicates that, when therapeutic orthodontic forces are applied, there is a degree of injury to the cementum. In current clinical practice, with the use of continuous light forces, this occurrence is less frequent. The repair of any limited cemental injury generally occurs. Alternatively, heavy orthodontic forces—whether continuous or intermittent—may lead to root resorption, because the cementoclasts remove not only cementum but also dentin of the root (Fig. 5-5). The permanent loss of root structure only occurs when an island of cementum and dentin becomes completely separated from the rest of the root surface. When this happens, resorption without reincorporation occurs.34,37,84,103,121 The permanent loss of root structure related to orthodontic treatment is generally seen at the root apex. Figure 5-5 A 14-year-old girl was referred by her orthodontist for surgical evaluation. She presented with a jaw deformity and associated malocclusion characterized by maxillary deficiency in combination with asymmetrical mandibular excess. She is congenitally missing teeth (all of the third molars, the maxillary right second molar, the maxillary left second molar, the mandibular left second bicuspid, and the mandibular right second bicuspid), and she has short dental roots. At the time of arrival, she had already undergone attempts at growth modification, including a face mask followed by rapid palatal expansion. At presentation, there was an asymmetrical Angle Class III negative overjet with a bilateral posterior crossbite malocclusion. Current maxillofacial dysmorphology and dental anomalies have negative consequences on the patient’s speech, swallowing, breathing, chewing, and lip closure/posture. At this time, the patient agreed to a comprehensive facial and dental rehabilitation approach with a desire to achieve improvements in breathing, lip closure/posture, occlusion, long-term dental health, and enhanced aesthetics. After periodontal and restorative dental evaluation, limited orthodontics and then jaw and intranasal procedures were carried out. The procedures included a Le Fort I osteotomy, sagittal ramus osteotomies of the mandible, an osseous genioplasty, a septoplasty, and inferior turbinate reduction. With finishing orthodontics, restorative dentistry is planned. A, Frontal views in repose before and after surgery. B, Frontal views with smile before and after surgery. C, Oblique facial views before and after surgery. D, Profile views before and after surgery. E, Occlusal views before retreatment, with orthodontics in progress, and then after surgery but before final restorative work. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after surgery. H, Panoramic radiographs before retreatment and after surgery. The resorption of the tooth roots during orthodontic treatment has been documented to occur in three distinct forms: (1) moderate generalized resorption; (2) severe generalized resorption (see Figs. 5-5 and 5-6); and (3) severe localized resorption. The shortening of the root length of the maxillary incisors (i.e., severe localized resorption) is seen more often than this condition appears to occur in the other teeth (Fig. 5-7). Although some studies have shown that measurable root resorption can be identified in 90% of maxillary incisors and in more than half of all other teeth during a typical fixed orthodontic appliance treatment, the shortening is almost imperceptible, and it is clinically insignificant for most. Nevertheless, occasionally the loss of one third or one half or more of the root structure is observed in patients who underwent what was considered to be routine orthodontic treatment. When this does occur, it is either severe generalized resorption or severe localized resorption. Fortunately, severe root resorption of all orthodontically treated teeth is not common. When severe generalized resorption does occur, it is often seen without any orthodontic or other forms of active dental treatment, and it may be of an uncertain etiology. If there is evidence of root resorption before orthodontic treatment, the patient should be considered at high risk for further resorption during orthodontic treatment. Radiographs should be taken during treatment to watch for this occurrence. If resorption becomes apparent, the patient is informed, and the treatment plan altered. In contrast with severe generalized resorption, severe localized resorption is more frequently associated with specific forms of orthodontic treatment. Risk factors are likely to include heavy continuous orthodontic forces being place on the teeth and a prolonged duration of treatment. Localized resorption is more frequently seen in the maxillary incisors, when the root apices are forced against the facial cortical plate during treatment. For example, in the clinician’s attempts to compensate for a long face Class II skeletal pattern with an anterior open bite, the maxillary incisor crowns may be detorqued (resulting in a loss of proper buccolingual inclination) and vertically lengthened as the bicuspid extraction sites and the open bite are closed. This may cause the incisor roots to come into heavy contact with the labial cortical plate and thus result in so-called “round tripping.” Forces must then be reapplied to the incisors to establish adequate palatal root torque.
Orthodontic Considerations in the Evaluation and Treatment of Dentofacial Deformities
Orthodontic Treatment Philosophy
The Biologic Basis for Orthodontic Tooth Movement
Periodontal Ligament Structure and Function

Response of the Teeth and the Periodontium to Normal Occlusal Function


Orthodontic Tooth Movement
The Periodontal Ligament and Bone Response to Sustained Orthodontic Force
The Amount of Orthodontic Force Applied to the Teeth
Medication Effects on the Rate of Orthodontic Tooth Movement
The Role of Anchorage in the Orthodontic Movement of Teeth
Reciprocal Tooth Movement
Cortical Walls as Limiting Factors to Orthodontic Tooth Movement
Negative Sequelae of Orthodontic Forces
Effects on Root Structure