59
Oral Diseases
Common Oral Mucosal Findings
Geographic Tongue (Migratory Glossitis)
• Well-demarcated areas of erythema and atrophy of the filiform papillae, surrounded by a whitish, hyperkeratotic serpiginous border (Fig. 59.1); lesions tend to migrate over time, may affect other oral sites, and are occasionally associated with a burning sensation.

Fig. 59.1 Geographic tongue. A florid example, demonstrating well-delineated areas of erythema partially surrounded by white serpiginous borders. Courtesy, Carl M. Allen, MD, and Charles Camisa, MD.
Scrotal (Fissured) Tongue
Hairy Tongue (Black Hairy Tongue)
• Confluence of hairlike projections, which represent elongated papillae, with yellowish to brown-black discoloration (Fig. 59.3); may have exogenous staining from food, tobacco, or chromogenic bacteria (especially following antibiotic therapy); some patients report an unpleasant odor or taste.
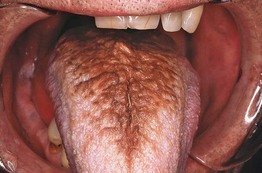
Fig. 59.3 Hairy tongue. The dorsum of the tongue exhibits marked accumulation of keratin and brown discoloration. Courtesy, Carl M. Allen, MD, and Charles Camisa, MD.
• DDx: pigmented papillae of the tongue (in individuals with darkly pigmented skin).
Median Rhomboid Glossitis
• Found in ~1% of adults, often associated with local overgrowth of Candida.
• Well-demarcated diamond- or oval-shaped area of erythema and atrophy on the dorsum of the tongue (Fig. 59.4).

Fig. 59.4 Median rhomboid glossitis. On the dorsum of the tongue (anterior to the circumvallate papillae), there is a well-demarcated, smooth area with loss of the filiform papillae.
• Rx: clotrimazole troches or oral fluconazole (for dosage, see Table 64.5).
Periodontal and Dental Conditions with Dermatologic Relevance
Desquamative Gingivitis
• Clinical finding that can occur in several immune-mediated vesicular and erosive disorders (Fig. 59.5); favors women over 40 years of age.
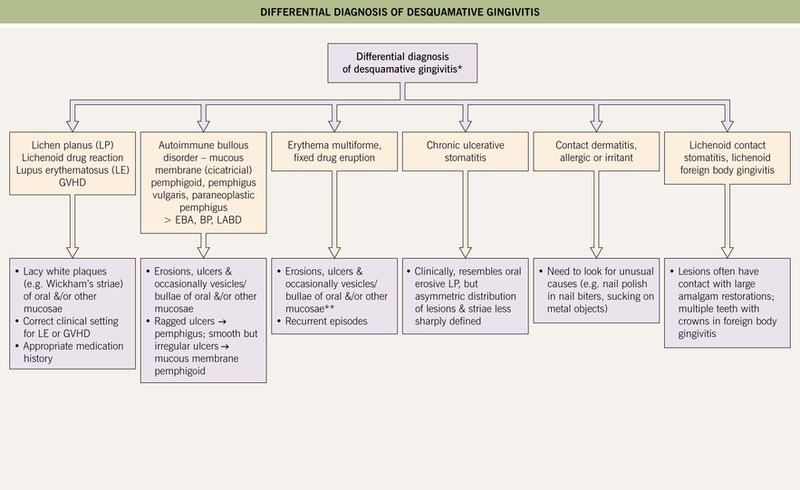
Fig. 59.5 Differential diagnosis of desquamative gingivitis. If the gingivae are painful, hemorrhagic, and necrotic with punched-out interdental papillae, then necrotizing ulcerative gingivitis (trench mouth) should also be considered. *No cutaneous lesions present. **Erythema multiforme is more likely to affect other mucosal sites. BP, bullous pemphigoid; EBA, epidermolysis bullosa acquisita; LABD, linear IgA bullous dermatosis. Courtesy, Carl M. Allen, MD, and Charles Camisa, MD.
• Diffuse gingival erythema with varying degrees of sloughing and erosion; frequently painful.
• Because desquamative gingivitis is often a manifestation of mucous membrane (cicatricial) pemphigoid and other autoimmune bullous disorders, evaluation should include routine histology plus direct and indirect immunofluorescence studies (see Chapter 23).
• Rx: treatment of underlying condition plus meticulous oral hygiene.
Gingival Enlargement (Hyperplasia, Overgrowth)
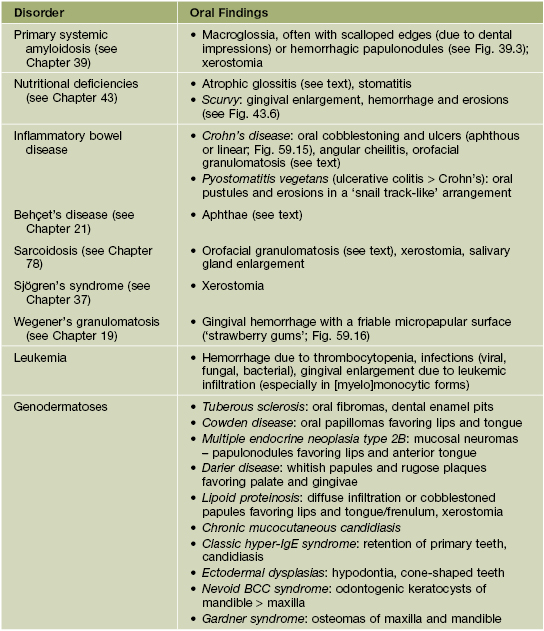
• Systemic medications and other causes of gingival enlargement are listed in Table 59.2.
Table 59.2
Causes of gingival enlargement.
Another term for Wegener’s granulomatosis is granulomatosis with polyangiitis (Wegener’s).
* Consider substitution with oral tacrolimus.
** Often contributes to gingival enlargement related to drugs and other factors.
Dental Sinus
• Occurs in the setting of a chronic periapical abscess in a carious tooth.
• Cutaneous: erythematous papule, often with an umbilicated or ulcerated center; found on the chin or submandibular region (mandibular teeth) > the cheek or upper lip (maxillary teeth) (Fig. 59.6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree