Chapter 13 Operative wound management
![]() Access the complete reference list online at http://www.expertconsult.com
Access the complete reference list online at http://www.expertconsult.com
![]() IN THIS CHAPTER
IN THIS CHAPTER ![]() Video Content Online • PowerPoint Presentation Online
Video Content Online • PowerPoint Presentation Online
Introduction
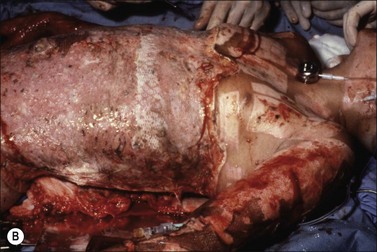
Surgery for burn injury is a key component to the multidisciplinary care of the burn patient. Early excision and grafting has dramatically changed the outcome and survival of the burn patient. Burned tissue promotes an inflammatory response at the junction of the eschar and the underlying viable tissue. Bacterial proliferation in the eschar attracts polymorphonuclear leukocytes that release large quantities of proteolytic enzymes and inflammatory mediators. Subsequent enzymatic action results in separation of the eschar, leaving granulation tissue. In large burns, the inflammatory response at the burned site becomes systemic. Mediators such as prostanoids, thromboxane, histamine, cytokines, and tumor necrosis factor are produced and released from the burn site. The serum levels of these mediators increase proportionally as the surface area of burn increases. The hypermetabolic response with increased protein catabolism, increased energy expenditure, weight loss, poor wound healing, and immune depression continues until the outpouring of mediators abates.1,2
Beneficial effects of operative wound management
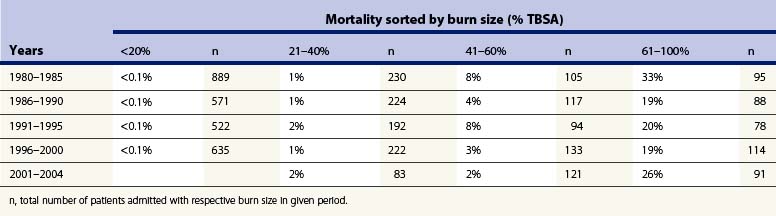
Early excision and skin grafting to achieve wound closure have been shown to reduce infectious complications, reduce the length of hospital stay, and improve survival in burned patients of all ages. Children in particular have benefited from more prompt and extensive surgical intervention.3,4 There has been a remarkable increase in the burn size associated with a 50% mortality risk over recent decades, such that it is now unusual for a child to succumb to burn injury of any size, even if it is associated with an inhalation injury (Tables 13.1 and 13.2). Early prompt initiation of resuscitation, nutritional support, proper critical care and treatment of infection have also played a part in this achievement. Early operative intervention, however, has contributed most towards this major advance. Burke and colleagues reported on results of total excision of full-thickness burns in 1974.5 They applied allografts to cover the wound after excision of burn and controlled rejection by adding immunosuppressants. Children with massive burns began surviving their injuries where they had never previously done so. Improved mortality, shorter hospital stay, and fewer metabolic complications were noted by others when early excision was retrospectively compared with late excision.6 When 32 children with an average age of 7 years and mean burn size of 65% total body surface area (TBSA) who underwent either total excision or serial debridement were studied, mortality, overall blood loss, and cumulative operating time were equivalent.7 The early excision group, however, had their length of hospital stay almost halved (97 ± 8 days vs 57 ± 5 days). Since that time, hundreds of children with burns >30% TBSA treated with early excision have exhibited a length of hospital stay less than 1 day/% TBSA burned.8
Table 13.1 Mortality following burn over time for different age groups, shown as the burn size at which 50% live or die – lethal area 50 (la50)
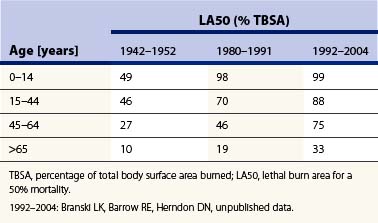
Table 13.2 Pediatric-specific mortality rates over time. Near-total early excision is the basis of these excellent results. Mortality and pediatric burn patients, Shriners Burn Institute, Galveston, Texas
Tompkins and colleagues showed that mortality of adult burn patients at Massachusetts General Hospital declined from 24% in 1974 to 7% for 1979–1984 after prompt eschar excision and immediate wound closure was instituted as standard.9 This study was expanded to include 85 patients aged 17–55 years.10 Those patients aged 17–30 years without inhalation injury showed significantly reduced mortality if treated by early excision (9%) than if treated conservatively (45%). Patients with a concomitant inhalation injury or aged over 30 years, however, derived no survival benefit from early excision. In burned children, Xiao-Wu and colleagues showed that delays in excision of severe burn were associated with longer hospitalization, delayed wound closure, increased rates of invasive wound infection, and increased incidence of sepsis.11
Munster and colleagues demonstrated a statistically significant decrease in length of hospital stay that correlated with a decrease in the interval between surgical interventions over a 14-year period.12 Other variables, such as burn size, inhalation injury, and age, remained static during this time; they found that mortality rate decreased significantly whereas burn indices remained constant. The average annual increase in hospital charges for burn care grew to 9.6%, which was substantially lower than the hospital as a whole (10.8%). Active surgical intervention in burn care can be associated with cost containment and fewer lives lost.
Elderly burn patients also have been shown to benefit from an early surgical treatment. Deitch and colleague operated upon consecutive patients with an average age of 68 years and showed a reduction of 40% in mean length of hospital stay compared to the national average, and mortality was less than predicted.13 Many studies show that early excision can be safely performed in the elderly, with clear benefit of reductions in duration of hospitalizations and the number of septic episodes.14–18
Hypertrophic burn scar formation is common, with dark-skinned patients being more prone to its development. However, the most important determinant of hypertrophic scar is delayed wound healing. Deitch and colleagues have shown that if wounds take more than 10 days to heal the risk is significant, and it rises to 80% if healing is delayed beyond 21 days.19 Surgery is therefore indicated for those whose wounds fail to heal promptly. Operative treatment is also an effective means of limiting the duration of pain that burn patients must endure. Excisional therapy of the burn wound is lifesaving, offers improved cosmetic and functional results, is cost-effective, and more swiftly returns the patient to their normal environment.
Techniques of burn wound excision
Excision of a small burn
Operative intervention is indicated without further delay once a burn wound is determined to be ‘deep.’ ‘Deep’ burns are those which are clearly either full-thickness or deep partial-thickness burns unlikely to heal within 3 weeks. These are typically flame or contact burns. Heimbach and colleagues observed that deep partial-thickness burns did not convert to full-thickness burns when topical antimicrobials were used to control infection.20 Although these wounds eventually healed after many weeks, they showed persistent blistering, pruritus, hypertrophic scar formation, and poor functional results. These observations prompted a prospective trial of early excision and grafting versus non-operative treatment of burns of indeterminate depth of < 20% TBSA.21,22 Shorter hospitalization, lower cost, less time away from work, but greater use of blood products, were seen in those treated with early operation. Those patients treated non-operatively required more late grafts for closure and also developed more hypertrophic scars.
Tangential excision
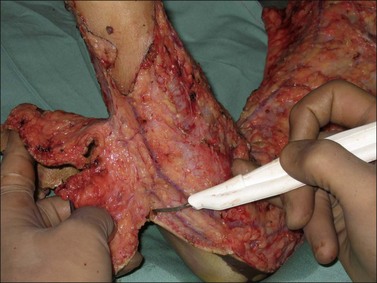
Tangential excision removes burned skin while preserving the underlying viable tissue. Body contours are better preserved than with fascial-level excision, and therefore this is the standard method for small burns. The technique of tangential excision was originally described by Janzekovic, who observed that deep skin graft donor sites could be grafted with thinner split-thickness skin graft taken from another area.23 She then extended this concept to partial-thickness burns by excising thin layers of burn until viable tissue was reached (Fig. 13.1). Split-thickness skin grafts were immediately applied. This technique of tangential excision and autografting of partial-thickness burns was a major advance. Prior to this time, only full-thickness burns were excised, usually as a formal integumentectomy, taking subcutaneous fat and accompanying lymphatics down to the underlying layer of investing fascia (Fig. 13.2). Janzekovic analyzed the results of the use of tangential excision in over 2000 patients. She found that, compared to fascial excision, hospital length of stay, pain, and reconstructive procedures were decreased.24
(Adapted from Janzekovic Z. A new concept in the early excision and immediate grafting of burns. J Trauma 1970 Dec; 10(12): 1103–8 with permission.)23
A number of different instruments can be used to perform tangential excision. The Rosenberg knife, Goulian knife, Watson knife, and the Versajet Hydrosurgery System water dissector are used (Fig. 13.3).25 The Goulian knife and the Watson knife are probably the most popular instruments for tangential excision. If the burn depth is superficial, partial-thickness burns are debrided to a white, shiny dermal surface with punctate bleeding. In full-thickness burns, excision continues layer by layer until viable subcutaneous tissue with a yellow glistening appearance is reached. Dullness, purple discoloration, or thrombosed vessels indicate non-viable tissue upon which grafts will fail, and deeper excision is mandatory (Fig. 13.4). Grafts may take initially, but will eventually fail. When excision is performed on limbs with a pneumatic tourniquet, these features are especially important.
Controlling blood loss
Excision of burns can result in considerable, if not massive, blood loss. Tangential excision can lead to large blood loss unless measures are taken to limit potential hemorrhage. The simplest measure is to operate within 24 hours of injury. Vasoactive metabolites, particularly the potent vasoconstrictor thromboxane, are in abundance during this time to limit blood loss.26 Desai and colleagues showed in a prospective trial of 318 pediatric patients with burns >30% TBSA that early excision of burns is associated with an overall reduction in blood loss.26 The average blood loss per surface area excised (mL/cm2) was compared at various postburn periods of excision. The total blood loss during excision performed within the first 24 hours after burn was 0.4 mL/cm2 excised, compared to 0.75 mL/cm2 excised if performed between days 2 and 16 post burn. The blood loss dropped to 0.49 mL/cm2 excised if the procedure was performed after the 16th day. Overall mortality was 5% for an average burn size of 60% TBSA. Early excision had no adverse effect on mortality. Very early excision led to a halving of blood loss for both large and small burns26,27 (Fig. 13.5).
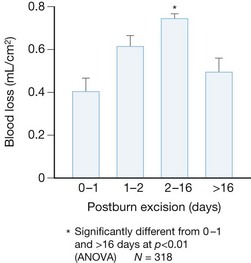
Figure 13.5 Blood loss is almost halved by operating within 24 hours of injury.
(Adapted from Desai MH, Herndon DN, Broemeling L, Barrow RE, Nichols RJ Jr, Rutan RL. Early burn wound excision significantly reduces blood loss. Ann Surg. 1990 Jun; 211(6): 753–9; discussion 759–62 with permission.)26
Other factors associated with increased blood loss during excision of burns are older age, male gender, larger body size, total area of full-thickness burns, high wound bacteria counts, total area excised, and operative time.27
Tumescence with epinephrine containing saline can be injected into the burn wound prior to excision. This technique is particularly useful for the trunk, scalp, and face; 1.6 mL of 1 : 1000 epinephrine (0.8 mL in pediatric patients) is added to 500 mL of 0.45% normal saline solution. The resulting local vasoconstriction will minimize blood loss. One-way syringes, such as the Multi-Ad Fluid Dispensing System or a pneumatic infuser, can make the injection process easier (Fig. 13.6). Monitoring the patient’s hemodynamics is necessary because the epinephrine may cause tachycardia and hypertension, which can worsen bleeding. Another drawback of this technique is that the lack of bleeding from the wound bed makes the adequacy of excision difficult to assess.
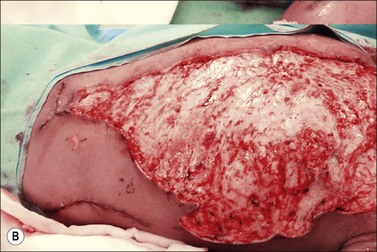
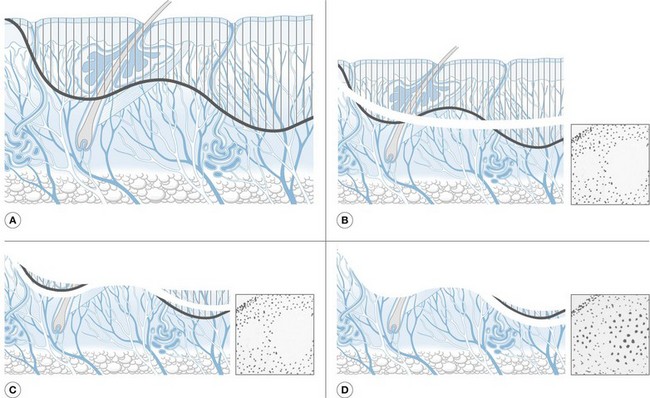
Techniques of wound closure
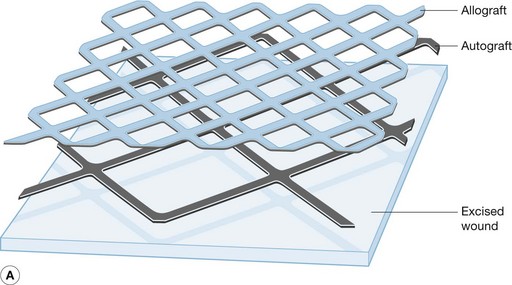
If burns are large and donor sites limited, autograft is meshed. This allows the autograft to be expanded to cover a wider area than its original size. The most common mesh ratios are 2 : 1 and 4 : 1, although different ratios of expansion can be employed. The main advantages of 2 : 1 meshed autograft is the easy handling and application, and the extensive network of slits that allows seroma or hematoma to drain. The main disadvantage is that the diamond-shaped interstices will leave a visible pattern once healed. Much larger areas can be covered when autografts are meshed 4 : 1 or greater and widely expanded. This widely meshed skin requires an overlay coverage of non-expanded allograft in a sandwich pattern to decrease the risk of graft loss. These are applied at 90° to the autograft in a sandwich pattern (Fig. 13.7).28 The difficult handling, the large interstices that take considerable amount of time to heal by epithelialization, the need for an allograft overlay, and the poor cosmetic result limit the use of meshed autograft to massively burned patients. Even in large burns, the face, neck, and hands are grafted with sheet split-thickness skin graft.
Figure 13.7 (a) Schematic representation of ‘sandwich’ technique of allograft overlay.
(Adapted from Alexander JW, MacMillan BG, Law E, Kittur DS. Treatment of severe burns with widely meshed skin autograft and meshed skin allograft overlay. J Trauma. 1981 Jun; 21(6): 433–8 with permission.)28
The Meek technique, which was later modified by Kreis and colleagues, is another tool to cover extremely large burn surface areas.29,30 It uses autograft cut into small squares with the aid of a dermatome and a cork board. These squares are then passed onto prefolded pleated gauze that is expanded in all four directions, leaving uniformly distributed islands of autograft which are then applied to the wound bed. Ratios of expansion can vary from 1 : 3 to 1 : 9. This technique has similar disadvantages to 4 : 1 meshed autograft and requires overlay with allograft.
Advances in wound closure
Dermal replacement
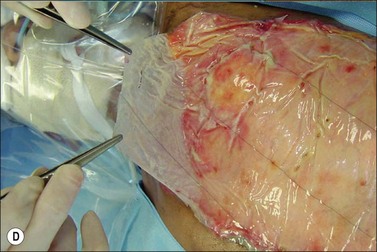
The use of dermal replacement in the treatment of burns brings new hope in providing the highly desired characteristics of normal dermis. Integra is a dermal analog composed of a porous matrix of cross-linked bovine collagen and glucosaminoglycan that provides a scaffold for a cellular invasion and capillary growth. This is placed over the wound bed after excision. The matrix is fully incorporated into the wound bed in 2–3 weeks and a thin split-thickness autograft is placed over it. Except for a possible increase in risk of infections, its use is safe and effective.31 Engraftment is aided by the use of negative-pressure dressings such as VAC Therapy (Fig. 13.8).32
Another dermal analog available for the treatment of full-thickness burns is Alloderm. This consists of cadaveric dermis devoid of cells and epithelial elements. Its use is very similar to that of other dermal analogs, and it has shown favorable results.33
Cultured epidermal autograft
Munster has shown that the use of CEA in the massively burned patient reduced mortality.34 CEA involves obtaining two 2 × 6 cm full-thickness specimens of unburned skin. The skin is processed and cultured ex vivo in the presence of murine fibroblasts that promote growth. The final product takes approximately 3 weeks to be ready for grafting and consists of sheets of keratinocytes, 2–8 cells thick; consequently, shearing and blistering is common for many months. Long-term survival of CEA is therefore particularly problematic on the posterior surfaces of these massively burned patients and goes some way towards explaining the 5–50% long-term CEA engraftment rates reported in the literature. CEA applied to areas such as the back, buttocks, posterior lower extremities, and other dependent areas is prone to shearing and possible graft loss. Barret and colleagues compared the use of CEA with wide mesh autograft and allograft overlay in a group of children with >90% TBSA.35 Once healed, the CEA has a better cosmetic result than healed 4 : 1 meshed autograft, but is associated with a longer hospital stay and more reconstructive procedures. Despite these limitations, including a substantial cost, series from different burn centers have shown promising results. When used in conjunction with allograft dermis, Sood and colleagues reported a graft take of over 72%.36
Tissue engineering technology is advancing rapidly. Fetal skin constructs have been recently successfully trialled and the bilaminar cultured skin substitute is showing promise.37,38