Fig. 12.1
Central lumpectomy. a Preoperative marking with the patient in the upright position. b Intraoperative marking with the patient in the supine position illustrating positional shift of the breast landmarks. c Initial skin incision revealing wide exposure over the target lesion. d Central resection. e Postexcision cavity. f Final closure
Once tissue specimens have been resected and hemostasis has been obtained, the fibroglandular tissue at the level of the pectoralis fascia is undermined so that breast-tissue advancement can be performed over the muscle. Once the fibroglandular tissues have been sufficiently mobilized and hemostasis has been confirmed, the margins of the residual cavity are shifted together by the advancement of breast tissue over muscle and the defect is sutured at the deepest edges using 3-0 absorbable sutures. The direction of tissue advancement can be adjusted depending upon the location of the fibroglandular defect and the excess tissue that can be shifted to close it. The goal of the mastopexy is to perform as complete a closure over the pectoralis muscle as possible to discourage communication between the anterior skin and the deeper tissues. Side to side comparisons with the patient in an upright position are warranted to ensure that no unusual retractions of the tissues or unsightly cosmetic results have occurred.
The superficial tissue layer is next closed with an interrupted subdermal 3-0 absorbable suture, and the skin is closed with 4-0 absorbable subcuticular sutures in routine fashion. Two variations on closure exist. The first, which is more typical, involves closure in a manner which results in a scar that is a horizontal, straight line, and the second involves closing the wound utilizing a purse-string closure to facilitate areolar tattooing.
12.4.2 Batwing Mastopexy Lumpectomy
For cancers adjacent to or deep to the NAC, but without direct involvement of the nipple, lumpectomy can successfully be performed without sacrifice of the nipple itself. The batwing approach preserves the viability of the NAC while preserving the breast mound by using mastopexy closure to close the resulting fibroglandular defect of the full-thickness resection. This procedure may result in lifting of the nipple into the upper breast, and a contralateral lift may need to be performed to achieve symmetry, especially when the native breast is large and pendulous.
Two similar semicircle incisions are made with angled “wings” on each side of the areola (Fig. 12.2a–e). The two half-circles are positioned so they can be reapproximated to each other at wound closure. Removal of these skin wings allows the two semicircles to be shifted together without creating redundant skin folds at closure. Fibroglandular tissue dissection is carried down deep to the known cancer, with the depth in relation to the chest wall dictated by the position of the lesion within the breast. In most situations, the dissection is carried down to the chest wall and the breast gland is lifted off the pectoralis muscle in a fashion similar to that for central lumpectomy. The principles of sharp dissection and the placement of marking clips are also similar to those utilized in central lumpectomy.


Fig. 12.2
Batwing mastopexy lumpectomy. a Preoperative marking with the patient in the upright position. b Intraoperative marking with the patient in the supine position. c Resection cavity. d Final closure. e Postoperative result with the patient in the upright position
Following full-thickness resection of the target, mobilization of the fibroglandular tissue for mastopexy closure will likely be required. The breast tissue is elevated off of the chest wall at the plane between the pectoralis muscle and breast gland, and the fibroglandular tissue is advanced to close the resulting defect. The deepest parts are approximated by interrupted sutures. We typically secure the fibroglandular tissue to fibroglandular tissue and do not place anchoring stitches into the chest wall, thereby allowing the approximated breast tissues to move along the chest wall. The superficial layer is closed in the same fashion as in central lumpectomy. As this procedure can cause some lifting of the nipple, it may create asymmetry compared with the noncancerous breast. A contralateral lift can be performed after adjuvant radiation therapy has been completed and the treated breast has “declared” its new size and shape to achieve symmetry, although some plastic surgeons may choose to perform this symmetry procedure concurrent with the oncologic surgery.
12.4.3 Donut Mastopexy Lumpectomy
For segmentally distributed cancers located in the upper or lateral breast that approach the NAC, donut mastopexy lumpectomy can be used to achieve effective resection of long, narrow segments of breast tissue. Donut mastopexy avoids a visible long radial scar which is against Kraissl’s line or Langer’s line. In this procedure (Fig. 12.3a–f), two concentric lines are placed around the areola and a periareolar “donut” skin island is excised, with only a periareolar scar visible after this operation. Deepithelialization by separating this skin island from the underlying tissues is done, taking care to avoid full devascularization of the areolar skin. The width of the “donut” skin island should be approximately 1 cm, but is somewhat dependent on the size of the areola and the expected extent of excision. Removal of this tissue ring is required, as it allows both adequate access to and exposure of the breast tissue and closure of the skin envelope around the remaining fibroglandular tissue that will reduce tissue volume overall.
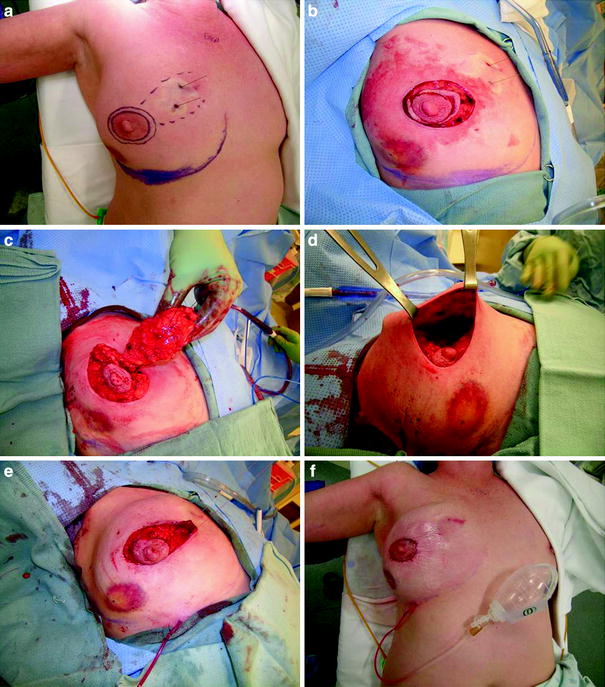
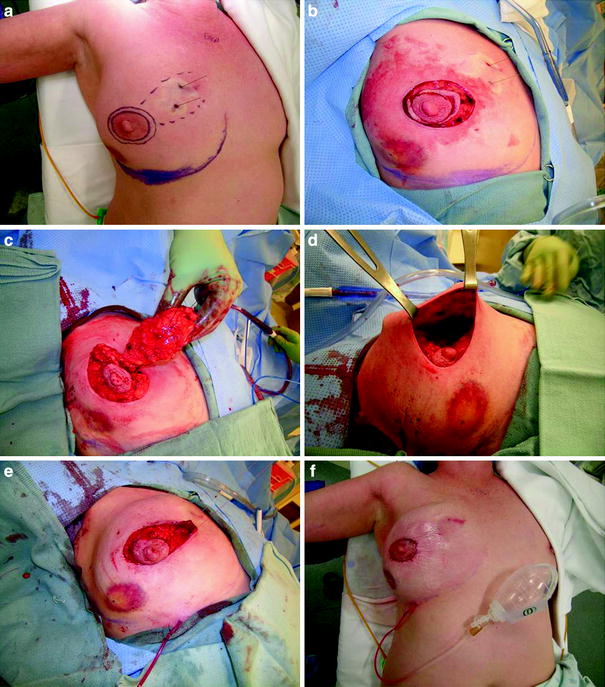
Fig. 12.3
Donut mastopexy lumpectomy. a Preoperative marking including marking of the region to be removed based on preoperative bracketing wires and concentric circles for skin donut excision. b Initial skin incision. c Delivery of tissue segment through the periareolar incision. d Remaining cavity after resection. e Purse-string closure. f Final operative result
A skin envelope is created in all directions around the NAC. The quadrant of breast tissue containing the target lesion is fully exposed utilizing the same dissection used for a skin-sparing mastectomy. The full-thickness breast gland is then separated from the underlying pectoralis muscle and delivered through the circumareolar incision. The segment of breast tissue with the tumor is resected in a wedge-shaped fashion, with the width of tissue excision required to achieve adequate surgical margins balanced against the difficulty that will be created by virtue of an oversized segmental defect.
The remaining fibroglandular tissue is returned to the skin envelope and the peripheral apical corners of the fibroglandular tissue are secured to each other and then anchored to the chest wall. This anchoring step maintains proper orientation of the mobilized fibroglandular tissue within the skin envelope during the initial phases of healing. A purse string using a 3-0 absorbable suture is placed around the areola opening, and is clamped at a size that reapproximates the original NAC. Interrupted inverted 3-0 absorbable sutures are placed subdermally around the NAC, at which time the purse-string suture is tied and then 4-0 subcuticular sutures are used to close the wound. Uplifting of the NAC may create mild asymmetry in comparison with the untreated breast. If desired, a contralateral lift can be performed to achieve symmetry.
12.4.4 Reduction Mastopexy Lumpectomy Modifications
Initially used in women with macromastia and excessive breast ptosis, this procedure is currently used for resection of lesions in the lower hemisphere of the breast between the 4 o’clock and 8 o’clock positions, where “scoop and run” lumpectomy using circumareolar incision would result in unacceptable down-turning of the nipple owing to scar contracture after radiotherapy. This unpleasant cosmetic outcome can be prevented by using the technique of reduction mastopexy lumpectomy (Fig. 12.4a–f). Recently, the indications for using reduction techniques have been expanded to include women with centrally located tumors faced with NAC loss. In these situations, the reduction is coupled with a deepithelialized pedicle flap with an overlying skin island to recreate the NAC, ultimately resulting in a Wise-type scar and a neo-nipple [16].


Fig. 12.4
Reduction mastopexy lumpectomy. a Preoperative skin markings showing the keyhole incision pattern. b Initial skin incision. c Full-thickness resection. d Excised specimen and residual cavity. e Closure. f Final result
In traditional reduction mammoplasty, a keyhole pattern incision is made and the skin above the areola is deepithelialized in preparation for skin closure. A superior pedicle flap is created by inframammary incision and undermining of the breast tissue off the pectoral fascia to mobilize the NAC and underlying tissues. Mobilization of the breast tissue allows palpation of both the deep and the superficial surfaces of the tumor, which can aid the surgeon in determining the lateral margins of excision around the target lesion. When it is used for a central lesion, the primary tumor and overlaying NAC are resected down to the chest wall. The principle of sharp dissection and the placement of marking clips are the same as those for parallelogram mastopexy lumpectomy. A caudally located inferior flap is then deepithelialized, except for an appropriately sized skin island that will function as the neo-nipple. Following this, redundant medial, lateral, and superior tissues are then resected while preserving the pedicle tissue. An incision at the inframammary crease facilitates mobilization and assists in restoration of normal breast shape and contour.
Once all tissues have been resected, the central, inferior pedicle is mobilized, brought cephalad, and utilized to occupy the defect created by removal of the prior NAC. The neo-nipple is sutured to the margins of NAC resection. The medial and lateral breast flaps are undermined and sutured together to fill the excision defect, leaving a typical inverted-T scar. Variations of this technique have been reported, including the Grisotti flap, which extends the pedicle laterally and results in an inferior and laterally sweeping incision [16], and free nipple graft from the skin of the contralateral reduction tissue [17




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








