Fig. 16.1
Preoperative marking and planning
With the breast lifted so that the lower pole can be seen, the drawing of the inferior flap is started at the central portion and is extended to 1–2 cm below the inferior edge of the areola.
16.4 Surgical Principle and Intraoperative Sequence for Tumor-Adapted Reduction Mammoplasty with a Modified Inferior Flap and a Superior Pedicled Nipple–Areola Complex
The outlined flap is decorticated, and an incision is made on its edges downward to the muscular level to allow the shaping of a dermolipoglandular flap, supplied by the fourth, fifth, and sixth intercostal perforating vessels (Fig. 16.2). The nipple–areola complex and the skin in the upper and lateral pole are completely undermined.
Fig. 16.2
Surgical principle of the reduction mammoplasty—modified inferior flap with superior pedicled nipple–areola complex (according to Rezai)
When the resection of the remaining tissue of the breast is complete, the flap is attached to the pectoralis fascia with separate stitches.
In the case of a tumor-adapted reduction mammoplasty (Fig. 16.3), the breast cancer is marked preoperatively with wires to achieve segmentally resected tumors for further histopathologic evaluation of tumor-free margins.
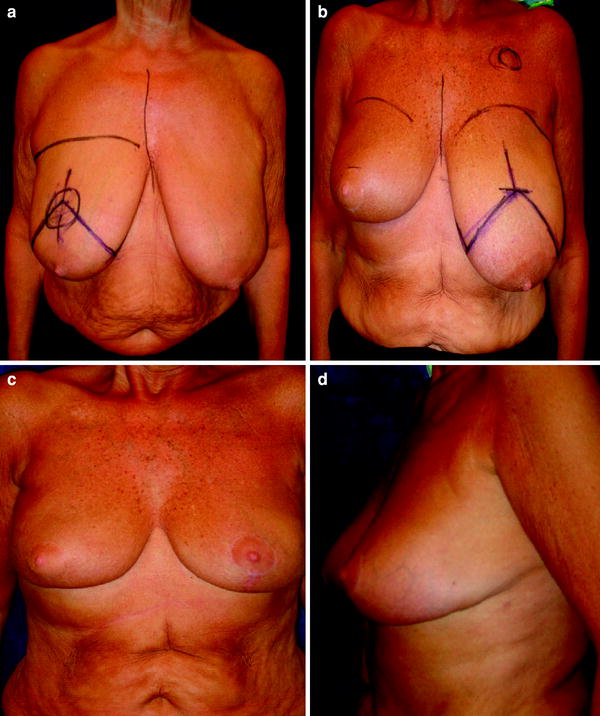
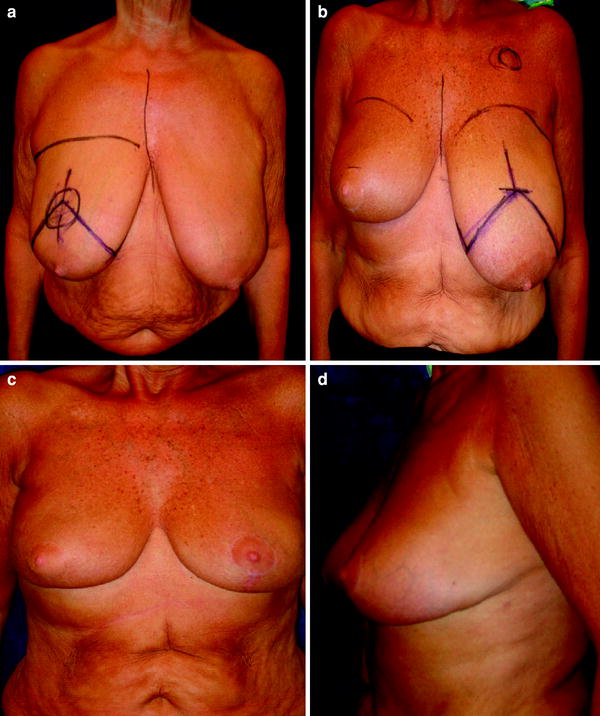
Fig. 16.3
Preoperative drawing and postoperative results. a Tumor-adapted reduction mammaplasty (right side). b Contralateral alignment (left side). c Postoperative result (anterior projection). d Postoperative result (lateral projection)
The lower edges of the lateral lines are joined at the middle point of the flap base. The new position of the nipple–areola complex is marked at the main projection. After decortication, the superior pedicled nipple–areola complex and the skin are sutured with Monocryl 3-0 sutures.
This surgical principle for a modified inferior flap technique with an inverted-T skin incision can also be combined with vertical, L, and periareolar skin incisions depending on the desired size and shape of the reduced breast.
Since 1993 we have performed this technique as a routine procedure in aesthetic reduction mammoplasty and in tumor-adapted reduction mammoplasty as the surgical part of breast conservation treatment.
16.5 Timing of Contralateral Breast Alignment
Spear [14] emphasized that an immediate one-step procedure of tumor-adapted reduction mammaplasty and contralateral breast reduction gives the woman an important boost, both physically and psychologically, during management of their breast cancer.
Patel [15] did not find differences in a head-to-head-comparison of quality of life and aesthetic outcomes following immediate, staged-immediate, and delayed oncoplastic reduction mammoplasty. However, with a small number of patients in a 7-year period, we feel that a two-step procedure better avoids differences at mid-term (6 months) and thus provide women with better long-term results. The contralateral alignment of the breast may be exerted after 6 months when the ptosis of the breast that has been operated on is overt.
16.6 Comments and Discussion
Breast conservation therapy for early-stage breast cancer including a segmental partial mastectomy with an attempt to obtain a gross negative margin of at least 1 mm is the treatment of choice for patients with unicentric primary breast cancer. Postoperative breast radiation therapy is an essential component of breast conservation therapy, and results in 12-year local recurrence rates of 10 %, compared with 35 % seen in women who undergo lumpectomy without radiation therapy [3]. For women with locally advanced breast cancer, breast conservation therapy remains an option if the tumor can be appropriately downstaged with induction chemotherapy, and postoperative breast irradiation yields local recurrence rates that are similar to those seen with early-stage disease [2].
Breast cancer patients with macromastia (whether related to obesity or particular body habitus) present particular challenges to the radiation oncologist. The large breast may require higher-energy photons to ensure delivery of radiation to the deeper tissue, and the dose inhomogeneity that can result may lead to significant radiation toxicity with regard to the skin. Significantly worse aesthetic results from breast conservation treatment associated with large, pendulous breasts have been documented in several series [16, 17].
The fairly logical surgical therapeutic modification of reduction mammoplasty has attracted relatively poor attention. Its use as a postradiation procedure to restore symmetry in treated patients with macromastia has been discussed in a few case reports [14




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








