Positioning
■ Before the procedure, consideration should be given to marking skin landmarks with the patient in the upright sitting position.
■ Relevant landmarks to be identified include the inframammary crease, the anterior axillary fold at the pectoralis major muscle, the posterior axillary fold of the latissimus dorsi muscle, the sternal border of the breast, and the periareolar circle. Identifying these structures with the patient in the sitting position is very important to the final cosmetic outcome, because these sites may be challenging to accurately locate once the patient is anesthetized and lying supine on the operating room (OR) table.
Approach
■ The patient should be supine on the OR table with the arms abducted.
■ It is preferable to have both breasts prepped and draped into the field so that visual comparison with the patient in a beach chair position is possible as the wound is closed. Such an approach allows the surgeon to identify areas of unsightly tugging or dimpling inadvertently created during closure so that they can be addressed at that time.
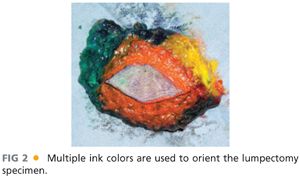
■ Multicolored inking can help orient the specimen and is best performed by the operating surgeon (FIG 2).
TECHNIQUES
PARALLELOGRAM MASTOPEXY LUMPECTOMY
■ The most basic of the oncoplastic techniques, this involves removal of the skin island located directly superficial to the known disease and is most commonly used for superior pole or lateral cancers.11
■ For upper inner quadrant lesions, the skin island excisions should be small or performed using a simple reapproximation of breast tissue and skin without removal of any skin island.12
■ Removal of the overlying parallelogram of skin avoids excessive, redundant skin from being left behind after excision and helps prevent declivity.
■ Be cautious when designing the skin ellipse, because removal of too broad of an island can cause substantial shifting of the NAC.
■ A rounded parallelogram with two equal length lines is drawn, thus marking the skin island to be excised in conjunction with the underlying target lesion and surrounding tissues (FIG 3). For lesions in the upper breast, incisions should be curvilinear, whereas lesions located within the lower breast, including the 3 o’clock and 9 o’clock positions, should have a radially placed parallelogram.

■ The proposed skin incision is made to breast parenchyma (FIG 4).

■ After excision of the skin island, short-distance mastectomy-type skin flaps are raised along both sides of the wound.
■ Dissection is carried down to the chest wall, the breast gland is lifted off the pectoralis muscle (FIG 5), and a standard tumor resection is performed.

■ Four to six marking clips are typically placed at the base of the defect within the surrounding fibroglandular tissue.
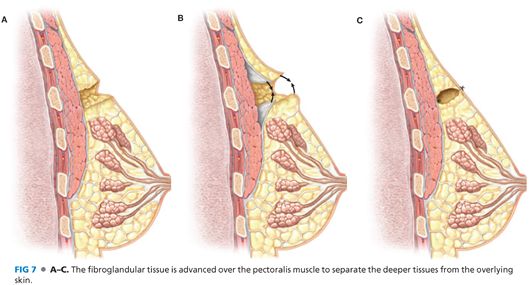
■ Once resection is complete and hemostasis obtained, the fibroglandular tissue at the level of the pectoralis fascia is undermined so that breast tissue advancement can be performed over the muscle (FIG 6).

■ The margins of the residual cavity are then shifted together by the advancement of breast tissue over muscle and the defect is sutured at the deepest edges using 3-0 absorbable suture. The direction of tissue advancement can be adjusted depending on the location of the fibroglandular defect and the excess tissue that can be shifted to close it. The goal of the mastopexy is to perform as complete of a closure over the pectoralis muscle as possible to discourage communication between the anterior skin and the deeper tissues (FIG 7).
■ The superficial tissue layer is closed with interrupted subdermal absorbable sutures (we use 3-0 sutures), whereas the skin is closed by absorbable subcuticular sutures (we use 4-0 sutures) in routine fashion (FIG 8).

BATWING MASTOPEXY LUMPECTOMY
■ For cancers adjacent to or deep to the NAC, but without direct involvement of the nipple, lumpectomy can be performed without sacrifice of the nipple itself.
■ The batwing approach simultaneously preserves NAC viability as well as the breast mound by using mastopexy closure to close the resulting fibroglandular defect of the full-thickness resection.
■ Two similar semicircle incisions are made with angled “wings” on each side of the areola (FIG 9). The two half circles are positioned to allow them to be reapproximated to each other at wound closure.

■ Removal of these skin wings allows the semicircles to be shifted together without creating redundant skin folds at closure (FIG 10).

■ Fibroglandular tissue dissection is carried down deep to the known cancer. In most situations, this dissection is carried down to the chest wall, with the breast gland lifted off the pectoralis muscle in a fashion similar to that for the parallelogram lumpectomy (FIG 11).

■ Following full-thickness resection of the targeted lesion, some mobilization of the fibroglandular tissue for mastopexy closure may be required. The breast tissue is elevated off of the chest wall at the plane between the pectoralis muscle and breast gland and the remaining fibroglandular tissue is then advanced to close the resulting defect.
■ We typically secure the fibroglandular tissue to itself but do not place anchoring stitches into the chest wall, thereby allowing the reapproximated breast tissues to move on the chest wall and adjust to find its most natural way to settle in for final healing. It is important to remember that what looks perfect on the chest wall when the patient is supine on the OR table may not sit as well when she sits upright and the breast becomes pendulous.
■ The superficial layer is closed in the same fashion as the parallelogram mastopexy lumpectomy (FIG 12).

■ As this procedure can cause some lifting of the nipple, it may create asymmetry when compared to the contralateral breast. If desired, a contralateral lift can be performed. Although this can be performed concurrently at the time of lumpectomy, it may be preferable after adjuvant radiation has finished and the treated breast has “declared” its new size and shape.
LATERAL SEGMENTECTOMY
■ A variation of the parallelogram lumpectomy, the lateral segmentectomy is especially useful for lesions located within the lower breast, including the 3 o’clock and 9 o’clock positions.
■ The skin parallelogram is placed radially and, at the corner of the parallelogram which comes closest to the nipple, the design should be positioned such that the closed incision after resection will approach the NAC tangential to the periareolar line (FIG 13). This reduces deviation of the NAC toward the lesion, a condition that can result from scar contraction.
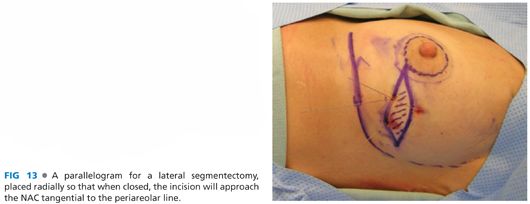
■ This radial approach gives more projection to the nipple, avoiding the downward displacement, which can be caused by a purely horizontal scar in the lower pole of the breast.
■ The proposed skin incision is made to breast parenchyma.
■ After excision of the skin island, short-distance mastectomy-type skin flaps are raised along both sides of the wound.
■ Dissection is carried down to the chest wall, the breast gland is lifted off the pectoralis muscle, and a standard tumor resection is performed (FIG 14).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








