
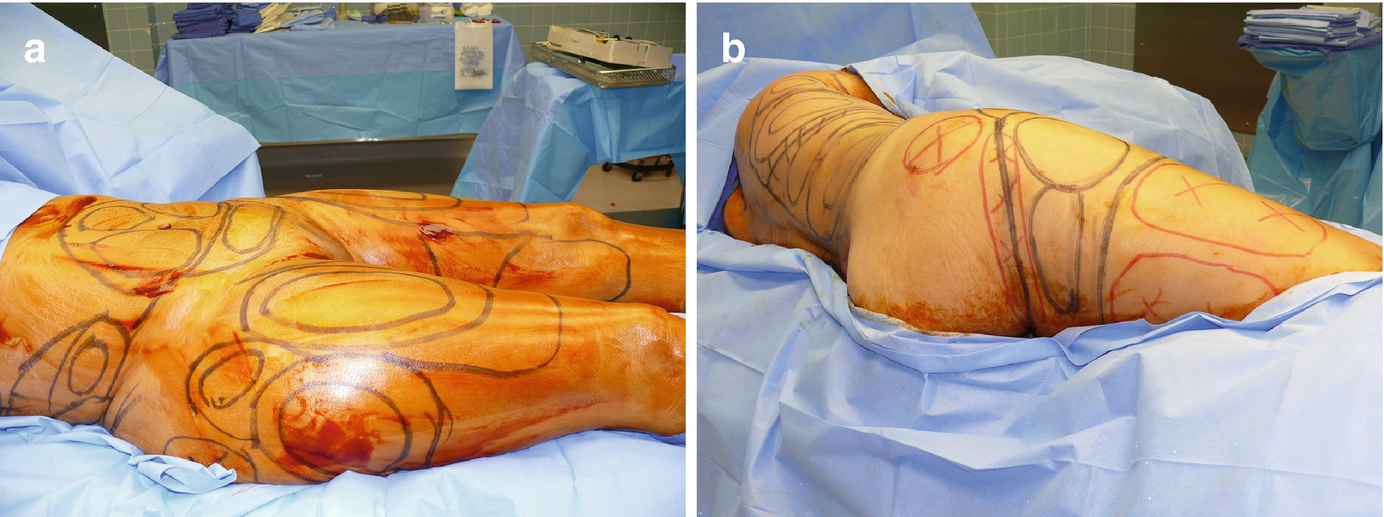
(a–e) Preoperative markings, lower extremities. Zones of adherence are marked in red
For the purpose of planning contouring procedures in the upper extremity, Gilliland and Lyos [8] conceptually divided the arm into three regions: anteromedial, anterolateral, and posterolateral. The majority of the lipodystrophy in the upper extremity occurs in the posterolateral area of the arm. A small amount of fat is present in the anterolateral region and there is minimal fat in the anteromedial region. The great majority of upper extremity liposuction is performed in the posterolateral and anterolateral regions. Liposuction in the anteromedial region should be avoided in most cases since a pinch test in this region frequently is less than 1 cm and extracting fat in this area commonly results in contour irregularities.
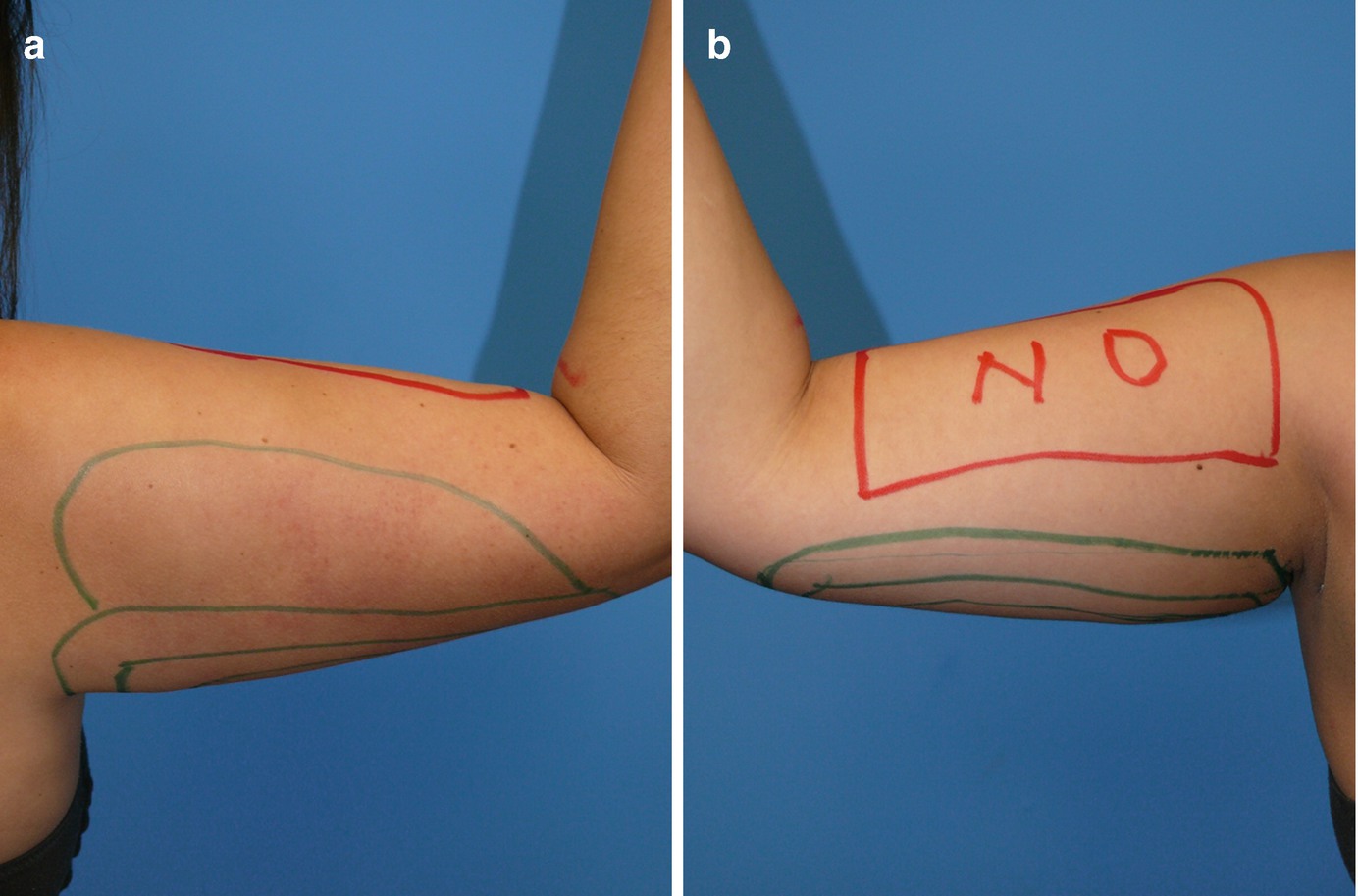
(a, b) Preoperative markings, upper extremities. Areas marked in red should be avoided
Indications
Thigh contouring: patient selection criteria
Type | Skin tone | Degree of lipodystrophy | Recommendations |
|---|---|---|---|
I. | Good skin tone | Moderate | VAL, UAL, or SAL |
II. | Moderate laxity | Moderate | VAL or UAL |
III. | Moderate laxity | Minimal | Thighplasty |
IV. | Significant laxity | Moderate to large | VAL-thighplasty |
Individuals who are close to their ideal body weight and have a disproportionately high distribution of fat in the lower extremities in relation to their trunk are still the best candidates for thigh liposuction. The fat in the upper medial thigh is soft, relatively loose, and covered by very thin dermis as opposed to upper lateral thigh fat which is dense, relatively fibrous, and covered by thicker dermis. These anatomical differences make the upper lateral thigh a relatively forgiving area for contouring with liposuction as opposed to the upper inner thigh which is quite unforgiving. Poor patient selection and overextraction resulting in excessive skin laxity and contour deformities are the most common causes of inferior aesthetic results following contouring of the thighs. Definitely any type of liposuction procedure of the medial thighs (either SAL or VAL) should be avoided in patients with significant skin laxity or minimal fat distribution in the area (pinch test of less than 2 cm). An excisional procedure such as a thighplasty is recommended for those patients. In patients with skin laxity and significant fatty deposits in the thigh, the author frequently performs a VASER-assisted thighplasty. This procedure is ideal for large thighs with loose skin since it limits the tissue undermining, diminishes the empty space, and preserves the majority of the lymphatic drainage. This technique has significantly reduced the seroma formation and wound healing complications that were associated with procedures that employed open resection and wide tissue undermining.
Arm contouring: patient selection criteria
Type | Skin tone | Degree of lipodystrophy | Recommendations |
|---|---|---|---|
I. | Good skin tone | Moderate | VAL, UAL, or SAL |
II. | Moderate laxity | Moderate | VAL or UAL |
III. | Moderate laxity | Minimal | Brachioplasty |
IV. | Significant laxity | Moderate to large | VAL-brachioplasty |
Patient Evaluation
The patient selection criteria have expanded over the years particularly since the advent of VAL; however one criterion that remains unchanged in patient selection is the health status of the prospective patient. As with any elective, aesthetic procedure, liposuction should be reserved for healthy individuals in relatively good physical condition. It is of paramount importance that from a psychological point of view, the prospective patient is capable of understanding the limitations of the surgery and can establish realistic expectations regarding the expected outcome. Once the patient meets the physical and psychological requirements for undergoing elective, aesthetic surgery, the plastic surgeon can then determine if they are a suitable candidate for liposuction. The most important factors to be evaluated in the particular anatomical area being considered for contouring are the amount of excess fat present and the condition of its overlying skin envelope.
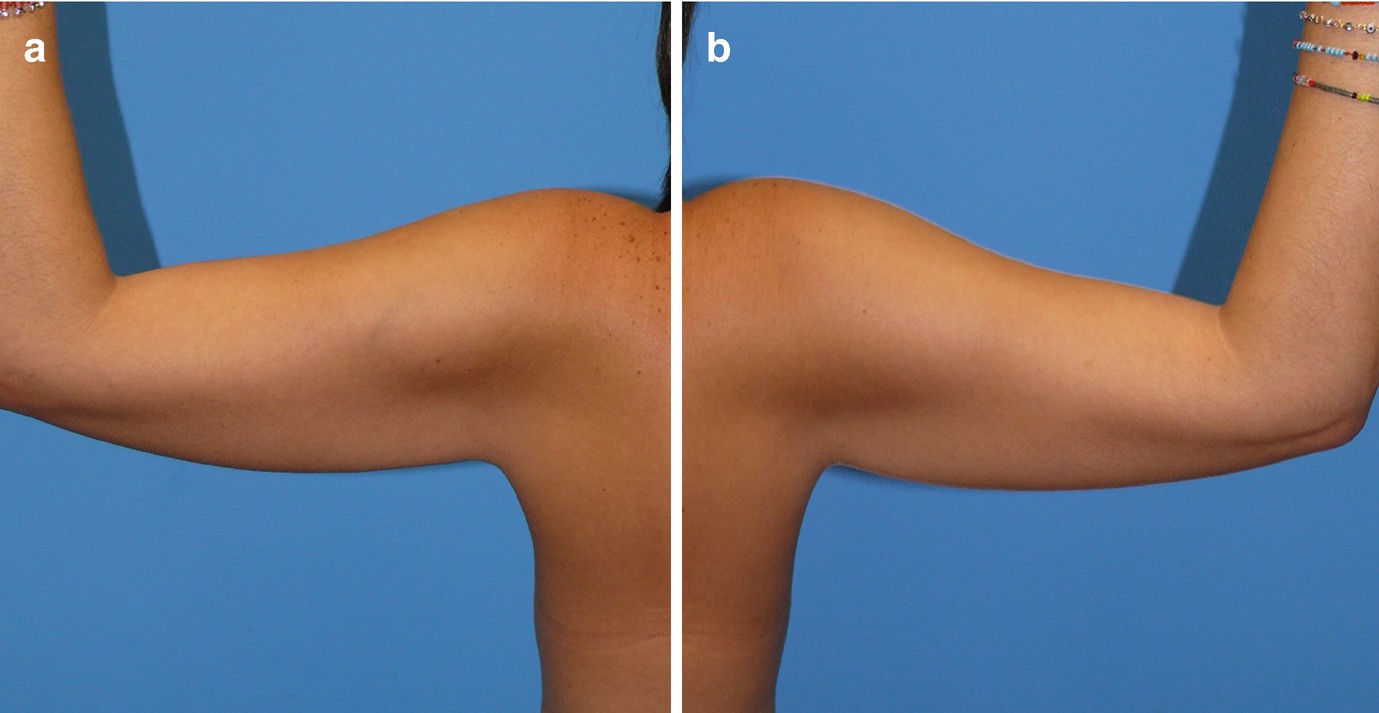
(a, b) Preoperative photography upper extremities
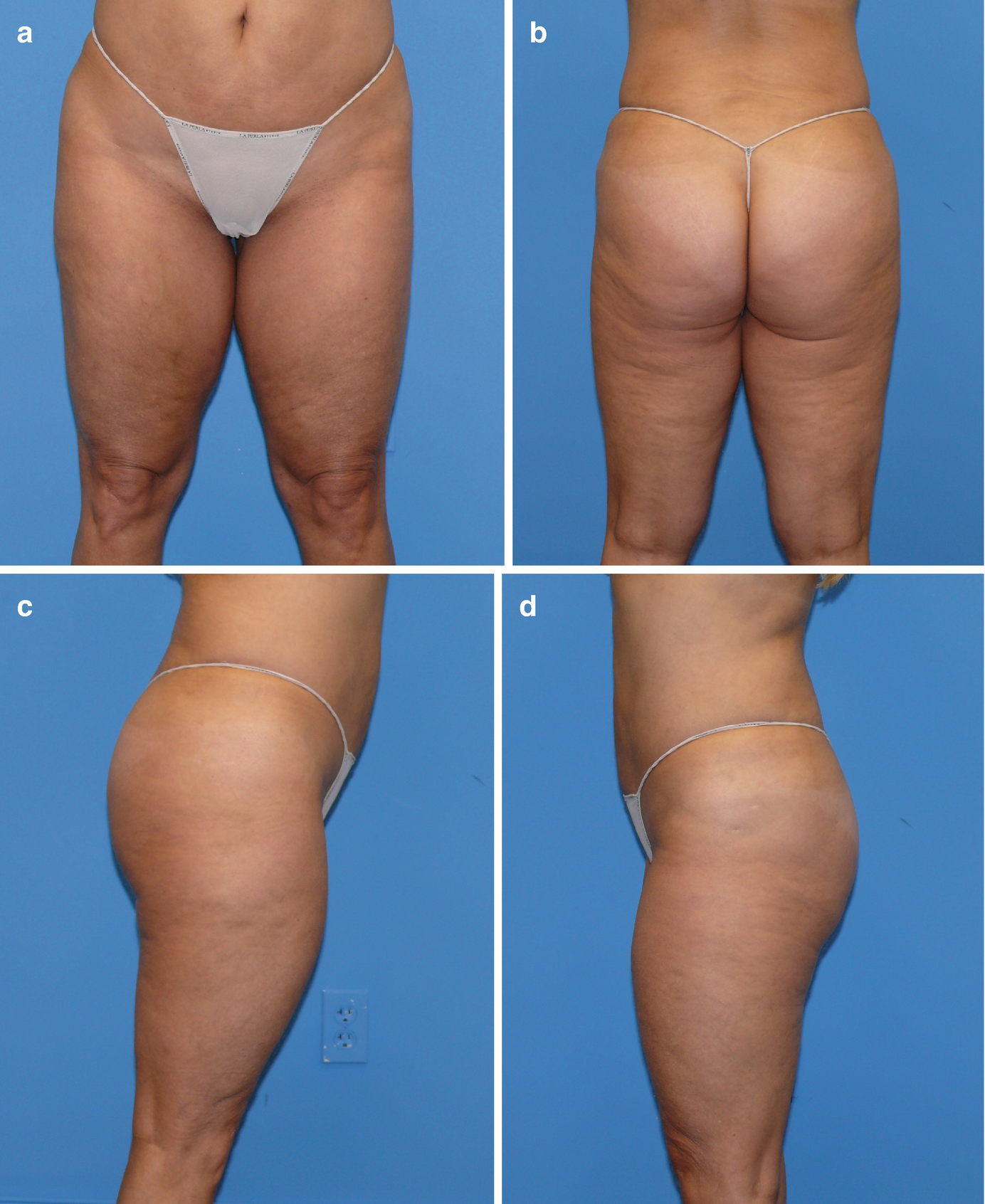
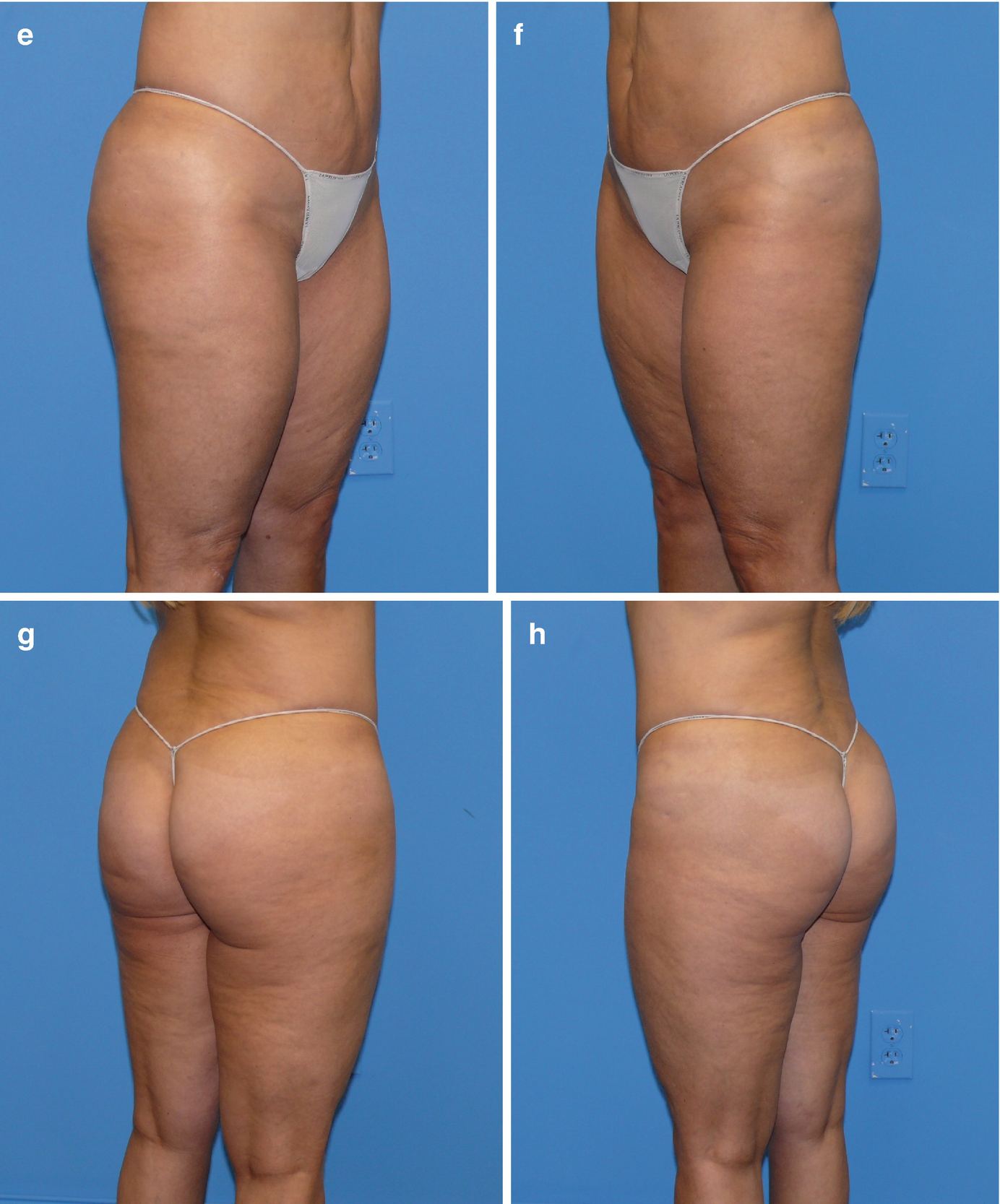
(a–h) Preoperative photography lower extremities
Planning and Preparation
When planning body contouring procedures, consistent photographic standards are of paramount importance. In order to ensure accurate preoperative and postoperative photographic comparisons, it is important to pay attention to details such as focal distances, positioning, lighting, and backdrops.
The proper procedure for informed consent requires that the patient is provided enough pertinent information about the proposed surgery in a manner that allows them to make an informed decision about the surgery. In addition to the universal risks of undergoing surgery under anesthesia, patients are informed of surgical risks pertinent to SAL and VAL: contour deformities or asymmetry necessitating secondary revisionary surgery, infection, bleeding, scarring, skin discoloration, sensory changes, seroma, fluid overload (pulmonary edema), severe dehydration (hypovolemic shock), chronic pain, peritoneal perforation with injury to deep structures, and possible skin and soft tissue burns as a result of UAL or VAL. Fortunately, major complications are rare in liposuction and the most common typically consist of minor contour deformities and asymmetries. As expected, the complication rate is higher in high-volume liposuction cases.
Prospective patients considering liposuction should undergo an extensive consultation that includes a thorough medical history and physical examination. It is important to discontinue any medications which may affect clotting mechanisms or platelet function in advance of the surgery. It is also important to examine for any risk factors that could potentially lead to deep vein thrombosis (DVT) and possibly progress to pulmonary emboli (PE). A survey of members of the American Society for Aesthetic Plastic Surgery (ASAPS) by Grazer and de Jong [10] reported a mortality rate of 19/100,000 for patients undergoing liposuction with approximately 25% of the deaths being the direct result of PE. Temourian and Rogers reported on more than 75,000 major liposuction procedures and found the incidence of DVT to be 33/100,000 and confirmed diagnosis of PE to be 12/100,000 [11]. Sequential pneumatic compression devices should be part of the routine protocol for major liposuction procedures. Although the protocol for patients at high risk for DVT during excisional body contouring procedures should include prophylactic doses of low molecular weight heparin, many plastic surgeons do not use pharmacologic prophylaxis for routine liposuction procedures mainly because of the increased risks of bleeding complications and excessive postoperative bruising. Liposuction patients are seldom immobile in the same position since they are frequently turned to different positions on the operating table during the surgery. These procedures are also associated with early postoperative ambulation and the patients are also encouraged to continue ambulate frequently during the first 2–3 weeks after surgery.
Surgical Technique
Whenever possible, it is the author’s preference to perform the preoperative markings in the office the day prior to surgery. The markings are performed with waterproof markers, are photographed, and are reviewed with the patient while pointing out asymmetries or contour irregularities that may be present preoperatively. This procedure helps the patient have a better understanding of the surgical plan and avoids misunderstandings regarding the extent of the planned contouring or the placement of the incisions. During the preoperative marking session the surgeon must pay close attention to the placement of the access incisions since ultrasonic liposuction surgery requires a greater number of access incisions of slightly longer length to accommodate the skin protectors. It is imperative that the ultrasound probes have direct lineal access to the treatment areas since the probes do not bend and the surgeon should avoid placing torque on the probes.
The author performs the majority of the major liposuctions under general anesthesia using a wetting solution that consists of 1 ml of epinephrine 1:1000 added to a liter of Ringer’s lactate solution at room temperature [12]. Omitting lidocaine from the wetting solution in high-volume liposuction safely allows for high-volume infiltrations of the solution without the concern of lidocaine toxicity. Both UAL and VAL should be performed with high amounts of wetting solution well dispersed throughout the tissues. Ultrasonic liposuctions involving smaller surface areas can be safely performed under local tumescent anesthesia. In these cases, the author adds 30 ml of 1% lidocaine to each liter of his standard wetting solution. The safest recommendation regarding the use of lidocaine in liposuction is to not exceed 35 mg/kg although some authors have reported on the routine use of lidocaine doses exceeding 50 mg/kg without complications [13].
Mild hypothermia in major liposuction cases is a common occurrence as a result of a number of factors encountered during the surgery such as large body surface areas exposed, large volume of wetting solution dispersed within the subcutaneous space, and thermoregulatory changes induced by prolonged general anesthesia. Employing a Bair Hugger over the head and all other nonoperative areas while using a fluid warmer for the intravenous fluids is helpful in maintaining core body temperature and is an efficient method for combating hypothermia in liposuction patients.
It was once common to cover the operating table with sterile sheets and have the patient stand for the prepping which would be performed with povidone-iodine (Betadine) solution in a circumferential fashion. The patient would then lie on the sterile, draped operating table and the rest of the draping completed. Currently the preference of many plastic surgeons (including the author) is to prep and drape the patient already in the proper surgical position and under anesthesia. Betadine gel is the preferred prep. Appropriate access for circumferential VAL of the lower extremities requires repositioning of the patient on the operating table.
(a, b) Supine and lateral decubitus positions for VAL contouring of the lower extremities
Access incisions for UAL or VAL should be of sufficient length to accommodate the skin protectors. The wetting solution is infused at a rate of 400–500 ml/minute using a power infusion pump. The ultrasound energy is delivered to the medial knees and medial thighs by a five-ring, 3.7 mm diameter VASER probe (Solta Medical, Bothell, WA) at 70% energy level in VASER (pulsed) mode. Total ultrasound time for medial thighs and knees should be approximately 45 seconds per 100 ml of expected aspirate from these areas [14]. Ultrasound application to the lateral thighs, anterior thighs, hips, and infra-gluteal areas is delivered with a 3.7 diameter 5-ring probe at 80% energy level in VASER (pulsed) mode. Ultrasound times for these areas are approximately 1 minute per 100 ml of expected aspirate. Contouring of the calves is not nearly as common as thigh contouring. In this area the author recommends using relatively high amounts of wetting solution, about a 4:1 ratio of solution to expected aspirate. A five-ring, 3 mm diameter probe is used at 60–70% energy level in VASER (pulsed) mode for 45 seconds for every 100 ml of expected aspirate.
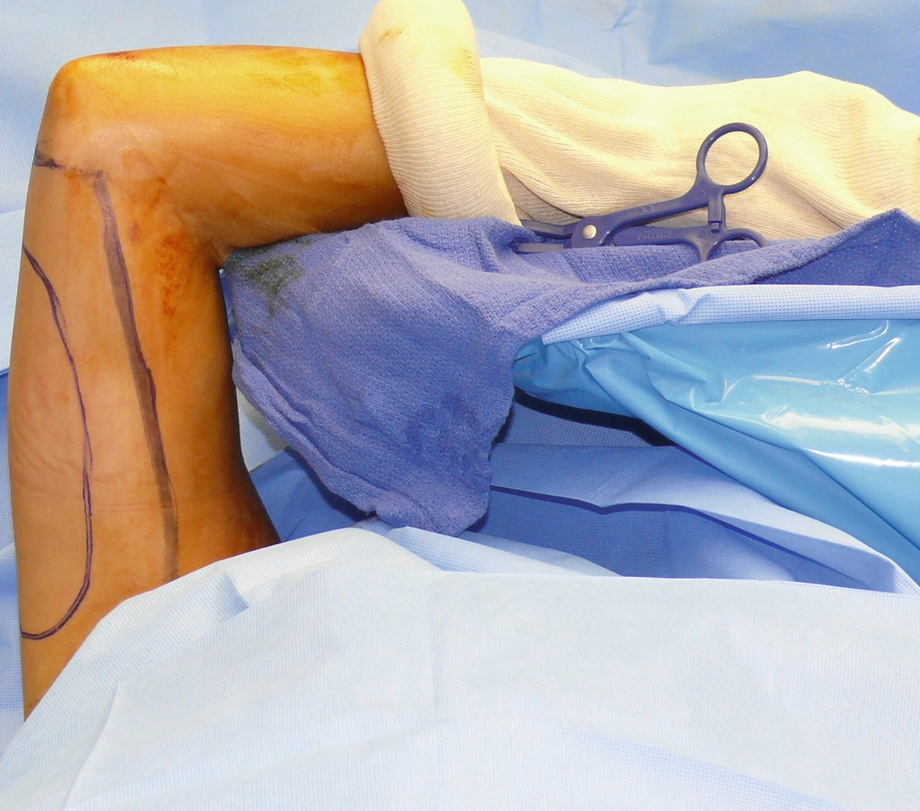
Intraoperative positioning for VAL contouring of the upper extremity. The arm is circumferentially prepped to allow free movement
It used to be commonplace during VAL procedures to deliver the ultrasound energy for 1 minute for every 100 ml of wetting solution infused. That formula may have been adequate when using a “superwet” technique with a 1:1 ratio of wetting solution to expected aspirate. However the current recommendation for VAL employs much higher volumes of wetting solution (at least 3:1 ratio of solution to expected aspirate) and the previous formula would deliver a higher dose of ultrasound energy to the tissues than what would be necessary to achieve adequate fat fragmentation.
VASER-assisted liposuction of the extremities: recommended ultrasound settings
Area | Energy (%) | Mode (V,C) | Probe | Exposure time |
|---|---|---|---|---|
Arms | 60–70 | V | 3.7 mm, 5-ring | 45 seconds/100 ml expected aspirate |
Medial knees | 70 | V | 3.0 mm, 3-ring | 45 seconds/100 ml expected aspirate |
Medial thighs | 60–70 | V | 3.7 mm, 5-ring | 45 seconds/100 ml expected aspirate |
Lateral thighs | 70–80 | V | 3.7 mm, 5-ring | 45–60 seconds/100 ml expected aspirate |
Infra-gluteal | 70–80 | V | 3.7 mm, 5-ring | 45–60 seconds/100 ml expected aspirate |
Hips | 80 | V | 3.7 mm, 5-ring | 60 seconds/100 ml expected aspirate |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








