Impact of Advances in Breast Cancer Management on Reconstructive and Aesthetic Breast Surgery
Keywords
• Breast cancer • Breast reconstruction • Prophylactic mastectomy • Skin sparing and nipple-areola sparing • Stem cells for breast reconstruction
Introduction
It is difficult to find an example of a multidisciplinary clinical niche showing more rapid growth and greater diversity than breast cancer care.1 In the 1980s, indications for breast reconstruction were liberalized as a result of increasing experience with various procedures, including microsurgery; development of implants, including tissue expanders designed for breast reconstruction; recognition of the beneficial psychological effects of breast reconstruction; and, most importantly, because of the clinical evidence that reconstructive procedures did not negatively affect the result of mastectomy (at that time the mainstay of the primary breast cancer treatment). Breast reconstructive procedures seem not to worsen the incidence of local and distant disease-free or overall survival in patients subjected to either mastectomy or different forms of breast conservation surgery (BCS) that were established in the 1990s. However, the natural evolution of breast cancer development risk assessment, the advances in diagnostic and surveillance methods, and the changes in the design of comprehensive breast cancer management necessitate the ongoing evaluation of reconstructive approaches to ensure that they do not hinder cancer detection or treatment. Similar concerns are shared in the context of aesthetic breast procedures. Many advances stem from past controversies; whether or not to reconstruct was itself recently a controversy. Practice guidelines for the management of breast cancer do not include detailed recommendations regarding aesthetic or reconstructive approaches.2,3 Without knowledge of controversies and recognition of advances in oncological breast care, plastic surgery would not be on par, both conceptually and technically, with quality medicine and surgery.1,4 This article shows how current diagnostic and therapeutic advances affect plastic surgery and how advances in plastic surgery affect breast care.
Impact of preventive, diagnostic, and breast management advances on reconstructive and aesthetic breast surgery
Prophylactic Mastectomy
One of the most effective options in preventing breast cancer is prophylactic mastectomy (PM). In high-risk patients, PM may be performed as a bilateral procedure; for women undergoing surgical treatment of unilateral breast cancer, there remains much debate about the role of contralateral PM (CPM). Supporters of CPM cite general statistics showing that CPM identifies occult malignancy in approximately 5% of cases and that CPM also decreases the risk of future contralateral breast cancer in more than 90% of cases.4 A woman is considered to be at high genetic risk for the development of breast cancer if she has a BRCA1 or BRCA2 gene mutation or her family history suggests an autosomal dominant pattern of inheritance.5 A woman with breast malignancy who presents at a young age or has relatives affected by breast cancer should consider testing for BRCA1 and BRCA2 mutations. Plastic surgeons counseling patient candidates for breast reconstructive or aesthetic surgeries have to be familiar with breast cancer risk assessment and recommend appropriate work-up (genetic testing, imaging).3,6 Breast cancer reducing strategies, other than PM or CPM, include ovarian ablation, endocrine treatment (eg, tamoxifen), and lifestyle adjustments.6 It is a difficult decision whether to undergo PM or CPM and, from the technical standpoint, timing of these procedures also matters (discussed later). Skeptics point out that the risk of breast cancer in the contralateral breast is overestimated and that breast cancer prevention strategies other than CPM are underappreciated. However, improvements in outcomes of breast reconstruction (BR) and high patient satisfaction rates from both PM and BR (90% range) boost plastic surgeons’ confidence and lower the threshold for PM/BR recommendation as an option.7,8 Furthermore, in arguing for PM or CPM, it could be claimed that risks and consequences of ovarian ablation and other breast cancer risk–reducing strategies are underestimated.9
Because plastic surgeons are increasingly involved in both PM and CPM, it is imperative that they can offer all technical variants of PM to match patient oncological needs and understand the implications of the technical choice for future risks and surveillance requirements. Regarding the simple or skin-sparing type of PM, because all types of mastectomy leave some breast tissue behind, subcutaneous mastectomy (in which nipple-areola complex [NAC] is preserved along with a minuscule layer of supporting breast tissue and terminal ducts segments) is associated with a greater risk of development of breast cancer than total mastectomy. More invasive forms of PM should therefore be recommended to high-risk women; however, strict selection criteria have not been established for the patients with breast cancer who are the best candidates for NAC-sparing mastectomy with an acceptably low risk of NAC tumor involvement.10 Total mastectomy, which includes the removal of breast tissue, NAC, and the axillary tail, is generally considered the preferred procedure for PM and is often followed by immediate BR.11,12
Skin and Nipple-Areola–Sparing Mastectomy
Skin sparing, skin reducing, and NAC sparing are key technical issues in BCS. They are important considerations in either prophylactic or therapeutic setting. Skin-sparing mastectomy is typically defined as the removal of the breast, NAC, previous biopsy incisions, and skin overlying superficial tumors (in therapeutic mastectomy). The cosmetic outcome significantly improves with the preservation of the skin envelope and the inframammary crease in particular.2,13 Skin-sparing therapeutic mastectomies are predominantly performed in patients with in situ T1 or T2 lesions. Skin-sparing mastectomy and immediate autologous tissue reconstruction is an common method of managing primary malignancies (in particular multifocal lesions) with good aesthetic outcomes.
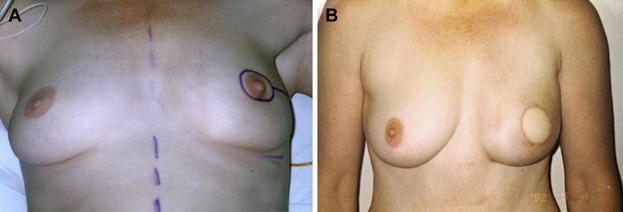
Could this approach be used for the previously irradiated breast? Observations indicate that skin-sparing mastectomy (SSM) and immediate autologous BR or a combination of flaps and implants give satisfactory cosmetic outcomes and oncological outcomes. Even when SSM and immediate BR are applied for the treatment of recurrent lesions, the rate of further recurrences is acceptably low (approximately 10%, comparable with salvage mastectomy) (Fig. 1).14
The next step in improving aesthetic outcomes is to preserve the NAC. However, whether the NAC SSM should be an option is questionable.10,15,16 In properly selected patients with lesions away from distal ducts, results of NAC sparing in the therapeutic setting would be oncologically acceptable if cancerous or high-risk lesions were histologically contiguous, but this has not been shown.17,18 The study examining the incidence of malignant areolar and nipple involvement separately concluded that, because the areola is less frequently involved than the nipple with terminal ducts (approximately 10% of nipples harbored cancerous tissue), only the areola should be spared.19 Subareolar tissue biopsy and extirpation of ducts distant from the nipple may not ensure oncological safety: approximately 6% to 7% of PM specimens harbored occult malignant lesions.20,21
It was stated earlier that the next step in improving aesthetic outcomes of BCS, is to preserve the NAC; however, there is no evidence from comparative studies that patient satisfaction from the NAC-sparing mastectomy technique is higher than from NAC reconstruction and that the nipple-areola–sparing option is cosmetically superior to de novo reconstruction, outweighing the oncological risks of nipple preservation, so the effort to spare nipples is a technical advancement.10 Unavoidable problems such as loss of nipple volume and tone, likely loss of sensitivity, and loss of erectile capability, and healing problems secondary to ischemia (at least 6% in both prophylactic and therapeutic settings) as the result of the nipple-areola–sparing technique, support a bias toward simply offering NAC reconstruction as the primary option for a mastectomy candidate.10,17,18 In patients with a significant ptosis (eg, a patient who had a history of significant body weight loss after bariatric surgery), a premastectomy surgical delay of NAC has been suggested, even with mastopexy.17,22
Other New Technical Issues in Breast Surgery: Oncoplasty
The concept of BCS put new demands on surgeons who had to abandon the concept of 1 size fits all and mastectomy as the universal answer to a breast cancer problem.1 With the customization of ablative approaches to ensure the best possible cosmetic result and the development of oncoplasty, surgical protocols ensuring adequate mastectomy and the integration of the cancer risk–reducing surgeries into overall breast care became diversified.2,23 The treatment of breast cancer (except lobular carcinoma in situ) conceptually includes the treatment of local disease with surgery and/or radiation therapy and the treatment of systemic disease with hormonal and cytotoxic chemotherapy. The trend in surgical ablation is toward less radical and disfiguring procedures that do not compromise the treatment of cancer. Configuration of incisions, as long as they provide a negative and adequate margin (at least 2 mm for most primary lesions) and include the lesion biopsy site, should not influence the outcome. Positive margins are more frequently associated with higher stage, positive nodes, lymphovascular invasion, younger age, positive estrogen receptors, and neoadjuvant chemotherapy.23 Positive margins are managed by local reexcisions or completion of mastectomy.
BR may vary from tissue rearrangements to locoregional flaps or free flaps. Tissue rearrangements and locoregional flaps are conceptually different types of mastopexy and are not new to plastic surgeons. Appropriate technical guides addressing repair guidance for different anatomic requirements are available.2,13,24 Small, centrally located breast cancers can be removed using Wise-pattern breast reduction incisions with a tumor-directed segmental mastectomy (Fig. 2). Lower quadrant tumors can be easily removed via vertical mammoplasty techniques. Both of these techniques allow large tumors in large breasts to be removed with good cosmetic results. In addition, upper outer quadrant tumors can be removed by a single axillary incision for quadrantectomy, axillary clearance, and, if needed for volume restoration, reconstruction with a latissimus dorsi flap.2,23–25
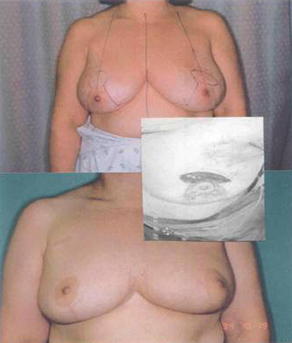
Fig. 2 Simple reconstructive scenario: T1 breast cancer with the lesion cranial to the NAC. Following excision, the defect was repaired using a Wise-pattern, inferior pedicle breast reduction technique. However, a major consideration when choosing the repair is the extent of excision volume and the need to provide breast symmetry.22 Therefore, the patient underwent breast reduction on the contralateral side.
In BCS, challenges will lead to technical advances beyond different types of mastopexy. The ability to determine adequate margins, in particular after presurgical radiation or neoadjuvant chemotherapy (resulting in tumor shrinkage); experience in reconstruction in cases with intraoperative or accelerated partial irradiation (both affecting the healing pattern); ability to manage breast cancer in patients with previous breast aesthetic surgery (with and without implants); and ability to supplement tissue rearrangement repairs with small, well-vascularized local flaps (Fig. 3) or alloplastic implants will be the trait of oncoplastic surgeons who are comfortable with all aspects of breast cancer management and who have mastered advanced (ie, diverse and customized) techniques.2,4,17,24,25 Many think that the technical challenges of partial BR frequently exceed those of complete mound reconstruction. Specifics of the technical advances of partial BR are presented by Dr M. Hamdi elsewhere in this issue.26
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree