Here we provide a concise, updated overview of non-invasive procedures for periorbital rejuvenation, including regenerative medicine modalities. We discuss managing periorbital rejuvenation with resurfacing lasers, vascular lasers, thermo-mechanical fractional injury treatment, radiofrequency, focused ultrasound, chemical peels, neurotoxin, dermal fillers, and finally, regenerative medicine, such as autologous fat transfer, platelet rich plasma, platelet rich fibrin, polynucleotide, and exosomes. By examining the benefits and limitations of each therapy, we aim to assist clinicians with the insights needed to choose the most effective treatment strategy for preriorbital rejuvenation.
Key points
- •
Periorbital age-related issues can be managed with non-invasive procedures such as high-intensity focused ultrasound, radiofrequency microneedling, botulinum toxin, fillers, chemical peels, laser resurfacing, and regenerative medicine.
- •
Comprehensive treatment plans may be designed per each periorbital area of defects after addressing underlying etiologies.
- •
While regenerative medicine, such as fat transfer, platelet-rich concentrate, exosomes, and polynucleotides, is promising for periorbital rejuvenation, it is limited by small subject study sizes, a lack of standardized protocols, and regulatory challenges.
| BoTN | botulinum toxin |
| CaHA | calcium hydroxyapatite |
| CO2 | carbon dioxide |
| Er:YAG | Erbium:Yttrium Aluminum Garnet |
| HA | hyaluronic acid |
| HIFU | high-intensity focused ultrasound |
| IPL | intense pulse light |
| KTP | potassium-titanyl-phosphate |
| MFU | microfocused ultrasound |
| PDGF | platelet-derived growth factor |
| PDL | pulse dye laser |
| PLLA | Poly- l -Lactic acid |
| PRF | platelet rich fibrin |
| PRP | platelet rich plasma |
| RF | radiofrequency |
| SOOF | sub-orbicularis oculi fat |
Introduction
The periocular region is often the first to exhibit signs of aging due to its delicate skin, thin underlying muscles, and frequent facial expressions. Factors such as genetic predisposition, sun exposure, repetitive movements, and smoking accelerate the loss of hyaluronic acid, collagen, and elastin resulting in various age-related changes, such as tear trough deformities, fat pad protrusion, rhytides, dermatochalasis, brow descent, temple hollowing, pseudoherniation of eyelid fat, involutional ptosis, elongation of the lower eyelid, photoaging, and hyperpigmentation. While surgical procedures like blepharoplasty have been the gold standard for periorbital rejuvenation, concerns about downtime, general anesthesia, and surgical anxiety often deter patients. As a result, non-surgical treatments have surged in popularity, including the growing interest in and advancements of regenerative medicine. While existing reviews on nonsurgical periorbital rejuvenation primarily focus on lasers and energy-based devices, this article expands on the topic by including an overview of regenerative medicine modalities, providing a broader presepective on emerging treatments in the field. We aim to provide a concise review of current non-invasive periorbital rejuvenation techniques, outlining their benefits and limitations to assist clinicians in selecting appropriate therapeutic approaches.
Resurfacing lasers
Overview
Resurfacing lasers deliver energy, instigating thermal reactions that promote dermal remodeling and collagen and elastin production.
- •
Based on the degree of epithelial disruption, these technologies can be broadly classified as:
- 1.
Ablative lasers
- 2.
Nonablative lasers
- 1.
- •
Depending on the uniformity of the treatment, they can also be categorized as:
- 1.
Fractionated
- 2.
Non-fractionated
- 1.
Ablative resurfacing devices vaporize the epidermis and part of the dermis to stimulate collagen production, dermal contraction, and tissue remodeling [ , ]. Full epithelial vaporization leads to significant tightening of the epidermis and dermis but is associated with prolonged downtime. Examples of ablative resurfacing lasers include the 10,600 nm carbon dioxide (CO2) laser and the 2940 nm Erbium:Yttrium Aluminum Garnet (Er:YAG) laser.
Although ablative laser resurfacing offers superior results for facial skin rejuvenation in improving texture, tone, and the appearance of wrinkles compared to other laser treatment modalities, rare but serious side effects such as lower lid ectropion along with scarring, hypopigmentation, or hyperpigmentation can occur, especially with non-fractionated CO2 lasers [ ]. Increased risk of hyperpigmentation in darker skin is another limitation of fully ablative laser non-fractionated resurfacing.
Fractional laser treatments are a suitable alternative for patients with darker skin tones. Fractional ablative resurfacing utilizes fractional photothermolysis, delivering energy in a gridline-patterned of microablative columns, creating microthermal zones. This technology induces thermal injury in these zones, facilitating heat shock protein formation around the dermis and stimulating collagen formation. Meanwhile, the surrounding skin around the zones is preserved, mitigating adverse effects like scarring or prolonged downtime [ ]. A study of 12 volunteers with Fitzpatrick skin types III to V and class II to IV on the Glogau wrinkle scale compared the effects of fractional Er:YAG (4 sessions, 2 weeks apart) with a single session of ablative Er:YAG laser. Both treatments showed comparable clinical improvement, though the ablative laser slightly outperformed the fractional laser. Histologic analysis revealed a significant decrease in elastin concentration and increased tropoelastin levels in both groups, with greater improvement observed after the ablative treatment. However, the fractional group experienced fewer side effects and milder erythema, with healing occurring within 2 to 4 days, whereas for the ablative group, complete re-epithelialization took 2 weeks, and erythema resolved within 1 to 3 months [ ].
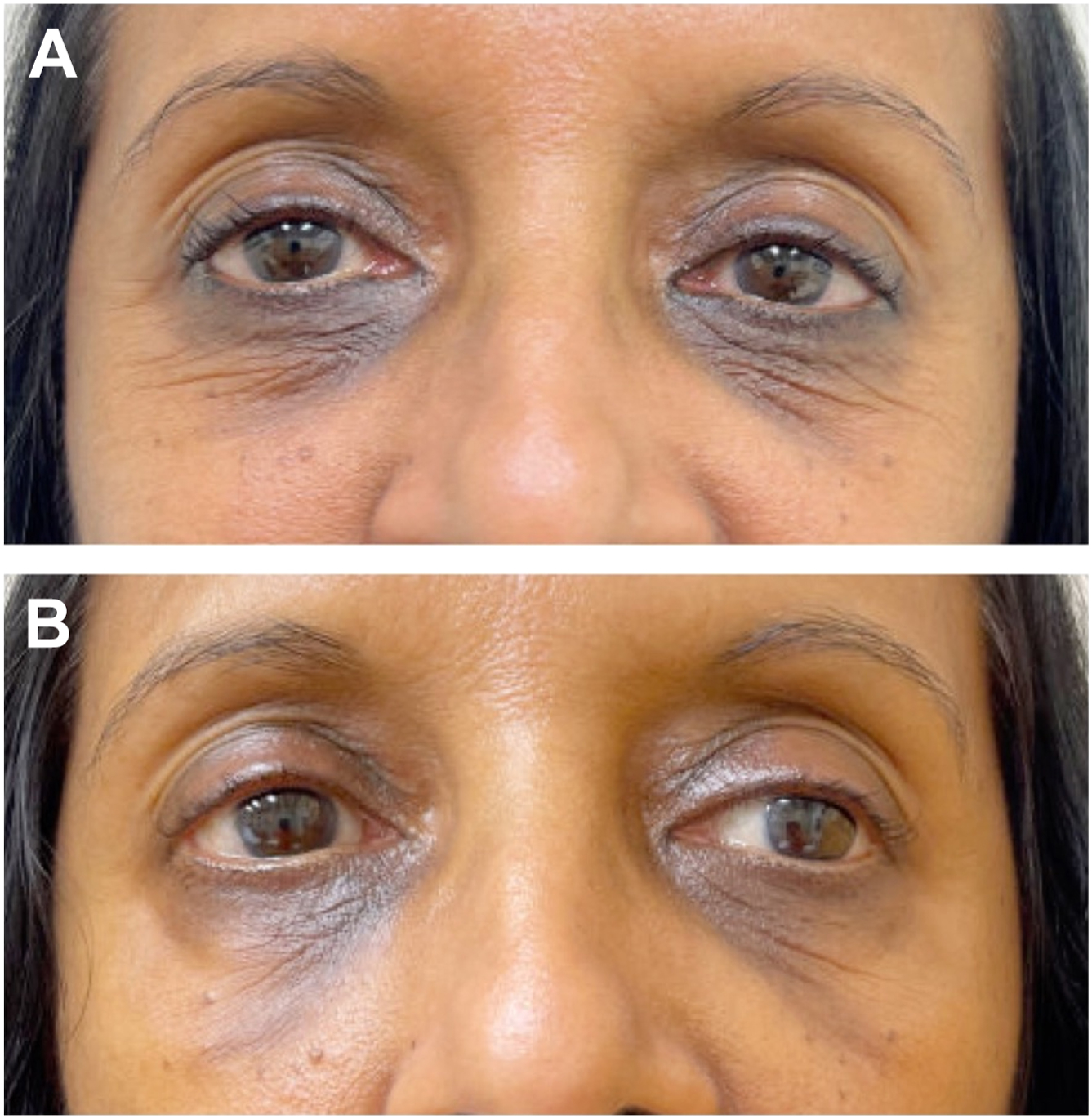
Nonablative resurfacing lasers induce thermal tissue coagulation without epithelial ablation and penetrate tissue deeper due to their lower water absorption coefficient than ablative lasers [ ]. Thermal injury from this treatment is confined to the dermis, typically resulting in fewer side effects and a shorter recovery than ablative lasers. However, these non-ablative approaches are generally less effective than their ablative counterparts for treating rhytides [ ]. Some examples of nonablative resurfacing laser devices include the 1927 nm thulium-doped laser ( Fig. 1 ), 1565 nm, 1540 nm, and 1550 nm erbium-doped lasers, the 1540 nm Er:Glass laser, the 1440 nm Nd: YAG, and 1410 nm diode nonablative fractional laser (NAFL) [ ]. Sukal and colleagues showed that 3 to 7 treatments with a 1550 nm NAFL, applied in 2 to 3 passes per area at 3 to 4 weeks intervals, resulted in eyelid tightening in all 31 patients, as assessed by 3 physicians using a 4-point evaluation scale, 3 to 4 weeks after the final treatment; additionally, 56% of the patients had increased eyelid aperture compared to their baseline [ ].

Hybrid Resurfacing Lasers
Integrating ablative and nonablative fractional technologies, hybrid resurfacing lasers allow energy delivery at multiple depths, thus improving both superficial skin texture and deeper rhytides. Applying deeper penetrating wavelengths tightens skin laxity, while the superficial wavelengths are efficacious in addressing pigmentary and textural alteration linked to the aging process [ ].
A study of 1 single-pass treatment with a CO2 and 1570-nm hybrid laser demonstrated significant periorbital rejuvenation. Mild-to-moderate erythema and crusting were seen, with an average downtime of 5.9 days [ ].
Vascular lasers
Various lasers can address periocular cutaneous vascular lesions by targeting the hemoglobin within the vessels, allowing for the destruction of blood vessels without epidermal changes.
Pulse dye laser (PDL), 585 nm and 595 nm, can treat the appearance of infraorbital bluish discoloration caused by vascular changes within the eyelid skin [ ]. While less frequently utilized for this purpose, PDL may have unintended benefits in mild to moderate periorbital rhytides and skin rejuvenation through a heating effect in deeper skin layers that stimulates collagen remodeling and tightening through the release of growth factors [ ].
Potassium-titanyl-phosphate, KTP, laser treatment can improve vascularity and pigmentation, even after a single treatment [ ]. A study showed a series of long-pulsed KTP laser treatments, ranging from 3 to 6 sessions, demonstrated significant improvements in redness and pigmentation, as assessed by investigator, subject, and observer scores [ ]; the treatments also showed mild to moderate improvement in skin tone and texture, with a mild improvement in rhytides, when compared to baseline photographs in a study [ ].
Nd:YAG lasers also demonstrate effectiveness in periorbital rejuvenation [ ].
- •
Q-switch Nd:YAG lasers target melanin due to their short pulse duration, reducing melanin and thus improving infraorbital hyperpigmentation [ ]. Significant enhancements in skin color, erythema, melanin pigment, and lightness were seen in a photo-analysis study, following 6 sessions of fractional Q-switch Nd:YAG laser treatment administered at 2-week intervals [ ].
- •
One to 2 treatments of long-pulsed Nd:YAG can improve the appearance of periorbital veins and is considered superior to KTP or PDL for treating periorbital veins [ ]. Contact cooling and post-procedure ice packs can mitigate the risks of scabbing, minor burns, and skin darkening [ ].
Q-switched ruby laser (694 nm) has also proven effective in treating infraorbital dark circles. A study observed improvement in 93% of patients treated with 8 fractional Q-switched ruby laser sessions at weekly intervals, as evidenced by before-and-after photo comparisons [ ].
Intense pulse light
Intense pulse light (IPL) therapy shows variable effectiveness in improving periorbital hyperpigmentation and rhytides [ ]. Due to its inconsistent efficacy around the eyes, other modalities are generally preferred for periorbital rejuvenation.
Thermo-mechanical fractional injury therapy
Non-laser, fractional, non-ablative, thermomechanical therapy (Tixel, Novoxel, Israel) applies up to 400°C of thermal energy to targeted tissue using a titanium handpiece tip. This tip utilizes brief pulses to achieve tissue coagulation in the dermis without disrupting the epidermis, thus resulting in little to no downtime. An ocular shield is also unnecessary during treatment as no chromophore is targeted. A study involving 3 to 5 sessions of the thermo-mechanical fractional injury therapy, spaced 3 to 5 weeks apart, showed improvement in mild to moderate periorbital rhytides, comparable to the outcomes achieved with 3 to 5 sessions of 1565 nm NAFL treatment, 3 to 5 weeks apart [ ].
In addition, the combination of thermomechanical therapy and topical application of 1% liquid tetracycline resulted in significant improvement in festoons, with a mean of 5.0 ± 1.9 treatments performed at intervals of 5.4 ± 1.2 weeks [ ].
Radiofrequency
Radiofrequency (RF) devices emit a rapidly alternating electromagnetic current to tissue and generate heat deep in the dermis and subcutaneous fat. The lower moisture content in the epidermis increases impedance, resulting in minimal surface ablation. This makes RF devices a suitable choice for the periorbital region, especially for darker skin tones, due to the reduced risk of hyperpigmentation and scarring [ ]. This energy generates thermal effects that trigger tissue remodeling, collagen contraction, and elastin production, with resultant enhancements in skin laxity, fine rhytides, skin reflectance, and hyperpigmentation.
RF devices can be subcategorized into monopolar, bipolar, or multipolar depending on electrode configuration.
The first monopolar RF device, Thermage (Solta, California, USA), was approved by the Food and Drug Administration in 2002 for periorbital rhytides and remains the only device with an indication for eyelid rejuvenation [ ]. Due to considerable pain and the rare side effect of lipolysis, low-energy techniques with multiple passes were adopted [ ].
For safety and tolerability in the periorbital region, transcutaneous, temperature-controlled, monopolar RF devices have been developed. These devices have automatic temperature feedback control of energy deposition at a targeted range of 40 to 45° Celsius to stimulate collagen remodeling and tightening [ ].
Bipolar and multipolar transcutaneous RF methods also offer controlled, well-tolerated superficial dermal injury through selective thermal coagulation. A significant improvement in periorbital skin texture was seen in patients over 50 years old compared to those below age 50 at 6-month follow-up after 3 treatments [ ].
RF with microneedling devices have been developed to deliver current through an array of needles into the skin, allowing for controlled heat penetration [ ]. A fractional modification permits the electric current to be exerted only at the distal tips of the needles in the dermis or subcutaneous fat by insulating the proximal portions. The resultant sparing of the epidermis further minimizes the potential side effects of post-inflammatory pigment alteration [ ].
Thus, RF devices can offer effective periorbital tightening with quick recovery and favorable side effect profiles. Full results typically appear in 4 to 6 weeks post-treatment, although multiple treatments are often needed [ ].
Focused ultrasound
- •
Microfocused ultrasound (MFU) uses high-frequency acoustic waves to produce microthermal zones of injury at specific depths within the dermis, resulting in dermal tightening through neocollagenesis, while sparing the epidermis. Approved for eyebrow lifting and tightening by the Food and Drug Administration (FDA) in 2009, intense MFU with visualization (Ulthera, Mesa, Arizona) has demonstrated its efficacy and safety for eyelid rejuvenation [ ].
- •
High-intensity focused ultrasound (HIFU) single treatment with 2.0-mm focal depth demonstrated significant improvement in periorbital rhytides, particularly in younger patients who tend to have more heat-labile collagen bonds, as opposed to the irreducible collagen multivalent cross-links found in older patients [ , ]. Upper and lower eyelid tightening using HIFU (ULTRAFORMER III, Classys, Seoul, Korea) was also observed in another study [ ]. However, caution is advised to avoid delivering excessive energy to the deep subcutaneous tissue since HIFU lacks real-time imaging during treatment [ , ].
- •
A high-intensity, high-frequency ultrasound device (Sofwave, Tel Aviv, Israel), has been designed to deliver acoustic energy via Synchronous Ultrasound Parallel Beam technology at an approximate depth of 1.5 mm, thereby eliminating the need for depth visualization during treatment [ ]. A newer hand-piece applicator with 3 ultrasound transducers allows for targeted treatments in hard-to-reach areas such as around the eyes. Approved by the FDA in 2019 for reducing fine lines and wrinkles, this device can achieve periorbital rejuvenation by delivering energy through an array of parallel, geometric, 3D cylindrical-shaped thermal zones, resulting in thermal coagulation and subsequent collagen and elastin remodeling in mid-dermis [ ].
Ocular safety
Improper eye shield usage can lead to complications like ectropion, visual disturbances, pain, and severe outcomes such as corneal injuries and retinal burns [ ].
Longer wavelength lasers such as Er:YAG and CO2 lasers have stronger water absorption and can cause corneal injury, whereas shorter wavelength lasers (400–1200 nm) such as PDL, Alexandrite, Nd:YAG, and IPL can have retinal absorption as they predominantly target melanin [ ]. Macular holes, a type of retinal damage, have been associated with 1064 nm lasers [ ].
While pulling the skin away from the orbit may help reduce ocular risks, patients need to wear metal shields for resurfacing and vascular lasers when treating around the eyelid margins. However, when using RF devices around the eyelid margins, plastic protective lens shields are more appropriate, as metal eye shields can overheat and cause potential corneal damage [ ].
Chemical peels
Depending on the type of peel, chemically ablating the epidermis with or without dermal injury results in varied levels of collagen production, dermal remodeling, and epithelial regeneration ( Fig. 2 ). This process can effectively rejuvenate the eyelids and address periocular hyperpigmentation ( Table 1 ).