This article presents an overview of the literature regarding treatments for keloid disease, hypertrophic scars, and striae distensae in dark pigmented skin. Striae, keloid, and hypertrophic scarring present a challenging problem for both the clinician and patient. No single therapy is advocated for hypertrophic scars, keloid scars, or striae distensae. New therapies have shown promise in the treatment of hypertrophic and keloid scars, and in patients with dark pigmented skin. This article provides guidance on the assessment and determination of patients’ suitability for certain treatment options, as well as advice on the follow-up of patients affected with problematic scarring and striae.
Key points
- •
Management of hypertrophic scars, keloid disease, and striae distensae in dark pigmented skin remains a clinical challenge.
- •
There are various treatment modalities; however, there is no single therapy that is advocated for hypertrophic scars, keloid disease, or striae distensae.
- •
Clinical risk scoring of abnormal scarring and striae distensae may allow those with high risk to be offered prophylactic therapies and preventive measures in advance.
- •
A focused history involving patient’s symptoms, signs, and quality of life/psychosocial well-being should be used in order to define goals and direct treatment options.
- •
Regular follow-up should be undertaken in order to assess whether treatment is effective, needs continuation for prevention of recurrence, or should be stopped.
Introduction
Cutaneous dermal injury inevitably leads to scar formation. The reparative process involves inflammation, granulation tissue formation, and matrix remodeling, which can result in varying degrees of dermal fibrosis ( Fig. 1 ). In certain individuals and anatomic sites, excessive fibrosis may lead to hypertrophic scar or keloid disease (KD) formation ( Fig. 2 ). In contrast, endogenous factors including mechanical stretching and hormonal influences can lead to dermal dehiscence, which can result in the development of striae distensae (SD) (see Fig. 2 ).

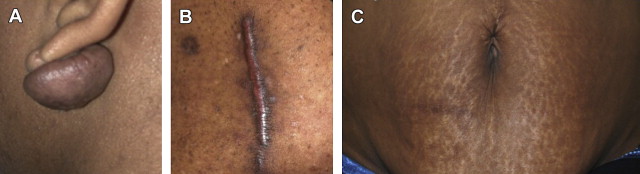
Keloid scars are raised reticular dermal lesions that spread beyond the confines of the original wound and invade the surrounding healthy skin ( Table 1 ). They can develop up to, or even beyond, 1 year after the injury and do not tend to regress spontaneously. Scars are erythematous, raised, firm areas of fibrotic skin that are limited to the original wound site. Hypertrophic scars (HTS) tend to form within the first month after the injury but can become flatter and more pliable over time and often resolve within a year. Both KD and HTS tend to be pruritic and painful and can be cosmetically unsightly. Their prevalence ranges from 4.5% to 16% of the population and they are thought to be most common in individuals with dark pigmented skin. KD and HTS are considered to be an important clinical problem in certain ethnic populations, because there is a higher prevalence in individuals with dark pigmented skin. KD, in particular, is reported to be especially high in individuals of African, Asian, and Hispanic descent.
| Hypertrophic Scars | Keloid Scars | Striae Distensae (Striae Rubrae) | Striae Distensae (Striae Albae) | |
|---|---|---|---|---|
| Onset | Develop soon after injury | Can develop months after injury | Usually occur during pregnancy, adolescence and obesity | Usually occur during pregnancy, adolescence and obesity |
| Physical characteristics | Remain within the confines of the wound | Spread beyond the boundaries of the wound | Early stage striae, raised red linear lesions | Pale, depressed and finely wrinkled lesions |
| Recurrence | Reduced risk of recurrence following treatment including surgery | High risk of recurrence following treatment including surgery | No risk of recurrence, although difficult to treat | No risk of recurrence, although difficult to treat |
| Occurrence | Usually located in high tension areas | Usually occur in areas including the earlobes and high tension areas such as the sternum | Common locations include the abdomen, breasts, thighs, hips | Common locations include the abdomen, breasts, thighs, hips |
| Skin Type | Associations with fair skin types | High association in dark pigmented skin | Due to mechanical stretching of the skin and hormonal imbalance. Skin type can affect treatment choice | Due to mechanical stretching of the skin and hormonal imbalance. Skin type can affect treatment choice |
| Permanent | Can regress spontaneously | Do not regress | Temporary form of striae | Permanent form of striae |
| Histological characteristics | Increased fibroblast density | Increased fibroblast density and proliferation rates | Thin epidermis, fine collagen bundles arranged in straight parallel lines | Thin epidermis, fine collagen bundles arranged in straight parallel lines |
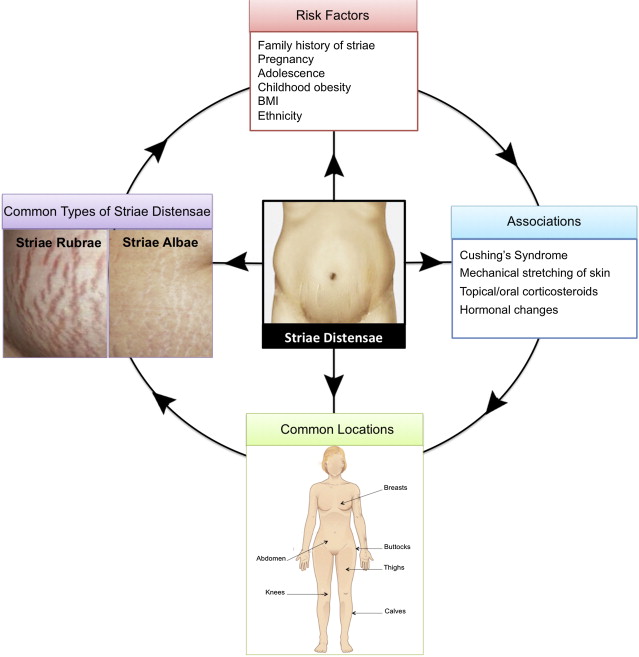
SD are linear bands of atrophic skin that occur following excessive dermal stretching (see Table 1 ). Most SD have been reported in pregnant women and adolescents and in long-term steroid use ( Fig. 3 ). SD often exhibit scarlike features because early striae (striae rubrae) appear erythematous and late striae (striae albae) show hypopigmentation and dermal fibrosis. There are also 2 additional types of SD: striae nigrae and striae caerulea, which occur in people with dark skin because of increased melanization. Striae nigrae appear as black bands of atrophic skin, whereas striae caerulea have a blue appearance. SD severity has been noted to be more severe in black African women compared with white people within the same geographic region.
Many different treatment modalities exist that claim to improve HTS, KD, and SD. Nevertheless, these lesions are difficult to eradicate using commonly available treatments. There is no single therapy that can effectively eradicate abnormal skin scars and SD. No single treatment plan has been advocated for both scars and SD, and the literature provides no gold standard therapy, which is hampered by a paucity of level 1 evidence. Therefore, this article summarizes a management strategy and provides an overview of the most current and available treatment options for managing KD, HTS, and SD in patients with dark pigmented skin.
Introduction
Cutaneous dermal injury inevitably leads to scar formation. The reparative process involves inflammation, granulation tissue formation, and matrix remodeling, which can result in varying degrees of dermal fibrosis ( Fig. 1 ). In certain individuals and anatomic sites, excessive fibrosis may lead to hypertrophic scar or keloid disease (KD) formation ( Fig. 2 ). In contrast, endogenous factors including mechanical stretching and hormonal influences can lead to dermal dehiscence, which can result in the development of striae distensae (SD) (see Fig. 2 ).
Keloid scars are raised reticular dermal lesions that spread beyond the confines of the original wound and invade the surrounding healthy skin ( Table 1 ). They can develop up to, or even beyond, 1 year after the injury and do not tend to regress spontaneously. Scars are erythematous, raised, firm areas of fibrotic skin that are limited to the original wound site. Hypertrophic scars (HTS) tend to form within the first month after the injury but can become flatter and more pliable over time and often resolve within a year. Both KD and HTS tend to be pruritic and painful and can be cosmetically unsightly. Their prevalence ranges from 4.5% to 16% of the population and they are thought to be most common in individuals with dark pigmented skin. KD and HTS are considered to be an important clinical problem in certain ethnic populations, because there is a higher prevalence in individuals with dark pigmented skin. KD, in particular, is reported to be especially high in individuals of African, Asian, and Hispanic descent.
| Hypertrophic Scars | Keloid Scars | Striae Distensae (Striae Rubrae) | Striae Distensae (Striae Albae) | |
|---|---|---|---|---|
| Onset | Develop soon after injury | Can develop months after injury | Usually occur during pregnancy, adolescence and obesity | Usually occur during pregnancy, adolescence and obesity |
| Physical characteristics | Remain within the confines of the wound | Spread beyond the boundaries of the wound | Early stage striae, raised red linear lesions | Pale, depressed and finely wrinkled lesions |
| Recurrence | Reduced risk of recurrence following treatment including surgery | High risk of recurrence following treatment including surgery | No risk of recurrence, although difficult to treat | No risk of recurrence, although difficult to treat |
| Occurrence | Usually located in high tension areas | Usually occur in areas including the earlobes and high tension areas such as the sternum | Common locations include the abdomen, breasts, thighs, hips | Common locations include the abdomen, breasts, thighs, hips |
| Skin Type | Associations with fair skin types | High association in dark pigmented skin | Due to mechanical stretching of the skin and hormonal imbalance. Skin type can affect treatment choice | Due to mechanical stretching of the skin and hormonal imbalance. Skin type can affect treatment choice |
| Permanent | Can regress spontaneously | Do not regress | Temporary form of striae | Permanent form of striae |
| Histological characteristics | Increased fibroblast density | Increased fibroblast density and proliferation rates | Thin epidermis, fine collagen bundles arranged in straight parallel lines | Thin epidermis, fine collagen bundles arranged in straight parallel lines |
SD are linear bands of atrophic skin that occur following excessive dermal stretching (see Table 1 ). Most SD have been reported in pregnant women and adolescents and in long-term steroid use ( Fig. 3 ). SD often exhibit scarlike features because early striae (striae rubrae) appear erythematous and late striae (striae albae) show hypopigmentation and dermal fibrosis. There are also 2 additional types of SD: striae nigrae and striae caerulea, which occur in people with dark skin because of increased melanization. Striae nigrae appear as black bands of atrophic skin, whereas striae caerulea have a blue appearance. SD severity has been noted to be more severe in black African women compared with white people within the same geographic region.
Many different treatment modalities exist that claim to improve HTS, KD, and SD. Nevertheless, these lesions are difficult to eradicate using commonly available treatments. There is no single therapy that can effectively eradicate abnormal skin scars and SD. No single treatment plan has been advocated for both scars and SD, and the literature provides no gold standard therapy, which is hampered by a paucity of level 1 evidence. Therefore, this article summarizes a management strategy and provides an overview of the most current and available treatment options for managing KD, HTS, and SD in patients with dark pigmented skin.
Patient evaluation overview
A thorough clinical assessment should be performed in order to tailor the appropriate management strategy to an individual affected with abnormal scarring or SD. This assessment should include a full medical history of the individual; any family history of KD, HTS, or SD; and presence of any psychosocial issues. In addition, the assessment should include a detailed history of the scar or striae, noting the size, contour, location, pliability, color, and any associated symptoms such as pruritus and pain. Furthermore, it is essential to take digital photographs before and after treatments to monitor any physical changes.
A range of instruments exist to monitor and quantify the physical and physiologic characteristics of KD and HTS by objective measures. Devices are used to measure the color of a scar such as spectrophotometric intracutaneous analysis, which provides a pigmentary status of the first 2 mm of the skin through reflectance and absorption of light. This device provides quantitative measurements of hemoglobin, melanin, and collagen levels. Epiluminescence colorimetry has also been used to identify the color of SD. Because this technique provides visualization of melanin, this may help in the visualization of SD in darker skin types.
Furthermore, full-field laser perfusion imaging provides quantitative measurements of vascularity that can evaluate the blood flow at the scar site. Scar volume is an important characteristic when assessing a lesion. Three-dimensional imaging devices are available for analyzing the volume, planimetry, and texture of skin scars and SD. Furthermore, ultrasonography techniques, such as the tissue ultrasound palpation system and DermaScan systems, can be used to quantify the total depth of a scar. Tools such as the tissue tonometer have been shown to be useful in assessing skin scar pliability. Techniques such as optical coherence tomography (OCT) have recently been used in assessing KD and HTS to visualize skin morphology and measure dimensions in the skin layers. In addition, in vivo confocal microscopy has been used in assessing KD, HTS, and SD by performing optical horizontal sectioning within human tissue, allowing a view of sections of the skin.
Because each patient is unique, it is important to create a tailored treatment protocol guided by evidence observed in effective therapies, remembering always to address the patient’s individual needs. A direct approach incorporating the patient’s symptoms, signs, quality of life, and well-being should be of paramount importance in order to target treatment effectively. In addition, regular follow-up is essential to ensure that treatment is effective, to identify any side effects, and to cease treatment in cases with successful outcomes.
Management goals
It is important to treat the patient’s clinical problems by first addressing the presenting complaints. A focused approach in targeting the individual’s symptoms, such as pain, pruritus, and inflammation, should take priority before aiming to reduce the lesion (in the case of keloid and HTS). Most of the therapeutic approaches are used indiscriminately for management of both HTS and keloids. However, clinical differentiation between HTS and keloid scars is vital before the initiation of any treatment, because of increased recurrence rates with keloids. For SD, goals of therapy are to provide long-lasting improvements in both pigmentation and texture of striae, with minimal side effects. Furthermore, it is important to evaluate the patients continuously following each treatment intervention, record progress and compare with the condition using a digital photograph, assess for side effects, evaluate objectively treatment, prevent complications, and cease therapy when indicated.
Pharmacologic treatment options
There are various pharmacologic treatment options that are available to treat KD, HTS, and SD. The most current and commonly used treatments are discussed later ( Table 2 ).
| Treatment | Indication | Dosage | Duration | Side Effects |
|---|---|---|---|---|
| Corticosteroids | KD + HTS | 1–40 mg/mL | Maximum dosage of 3 injections every 3–4 wk | Telangiectasia, atrophy, hypopigmentation, pain |
| 5-Fluorouracil | KD + HTS | 50 mg/mL | Weekly doses. Variable duration depending on response | Ulceration, hyperpigmentation, pain |
| Tretinoin | SD | 0.025%–0.1% | Daily application with variable duration depending on response | Mild skin irritation |
| Glycolic acid | SD | 10%–35% | 1–2 min repeated monthly for up to 6 mo | Stronger concentrations can lead to irreversible scar formation |
Intralesional Injections
Intralesional injections of corticosteroids are considered, by the International Clinical Recommendations on Scar Management, the standard first-line treatment of KD and a secondary treatment of HTS. There are several corticosteroids used for raised dermal scarring in dark pigmented skin, such as dexamethasone, hydrocortisone acetate, and methyl prednisolone, and the most common type of injection is triamcinolone acetonide. Injection of corticosteroids leads to the regression of KD and HTS by reducing the inflammatory process, altering collagen gene expression, and inhibiting collagen and glycosaminoglycan synthesis. The effectiveness of single or multiple injections can be variable and recurrence rates range from 9% to 50%. Triamcinolone acetonide can be used in a combination of doses (1–40 mg/mL). Three to 4 injections of triamcinolone acetonide (10–40 mg/mL) every 3 to 4 weeks are generally sufficient, although occasionally injections continue for 6 months or more. A recent case series conducted by our team evaluated the response rate of triamcinolone acetonide injections in 65 patients with KD including patients with dark pigmented skin. Triamcinolone acetonide was injected at a concentration of 10 mg/1 mL. The dose was 2 to 3 mg, with a maximum of 5 mg at any one site. A total dose of 30 mg was administered in line with British National Formulary (BNF) guidelines. The results showed that there was a 77% positive response rate, which was defined by an improvement in signs (color, height, contour) and symptoms (pain, pruritus) associated with raised dermal skin scarring. This finding shows level 4 evidence (level of evidence [LOE]-4) of the positive effects of triamcinolone acetonide for the treatment of KD and in patients with dark pigmented skin.
Berman and colleagues conducted a randomized controlled study (LOE-1) involving 20 patients of varying skin types, comparing intralesional steroid with etanercept in KD. Triamcinolone acetonide improved 11 out of 12 parameters assessed compared with etanercept, which improved 5 out of 12. The investigators reported that scar evaluations were blinded; however, it is unclear how this was achieved, because assessments were completed by the same investigator.
Darzi conducted a randomized controlled trial (RCT) (LOE-1) and compared 100 scars (KD and HTS) in 65 patients. Each received either beta radiation alone, or in combination with surgery, or triamcinolone acetonide. They showed that the scar symptoms improved (72%) and flattening of the scars were noted (64%) after receiving this therapy. This treatment can be painful and associated side effects include telangiectasia, atrophy, and pigmentary changes ( Fig. 4 ). Hypopigmentation often continues for years after treatment and is more highly visible in dark pigmented skin.
5-Fluorouracil (5-FU) is a pyrimidine analogue that is converted to a substrate that causes the inhibition of DNA synthesis. 5-FU is administered via intralesional injection either in single or multiple doses or at the time of surgery, and it is thought to reduce scarring by suppressing fibroblast proliferation. It has been advocated that intralesional injections of 5-FU should be administered once weekly at doses of 50 mg/mL for approximately 7 sessions. A comparative study (LOE-2) of 5 patients comparing various treatment regimes of 5-FU showed that the therapy was effective for HTS, as well as KD. Scars that were inflamed, firm, and symptomatic responded more significantly to 5-FU monotherapy or polytherapy.
A prospective study (LOE-4) conducted in India investigated the use of intralesional 5-FU and surgical excision in 28 patients, some with dark pigmented skin and with earlobe keloid scars. 5-FU was a useful method of reducing the recurrence of KD, because 27 of the patients required no further treatment in 22 months.
A double-blind RCT (LOE-1) recently tested the effects of 5-FU and topical silicone in 50 patients who were split into 2 groups, 1 treatment and 1 control group. The sample group included patients with dark pigmented skin as well as white people. The treated group had less recurrence (4% treated, compared with 22% control) and a greater number of patients who were keloid free (75% treated, compared with 43% control) compared with the control group. Furthermore, Sadeghinia and Sadheginia compared 5-FU with intralesional steroid injections in 40 patients with KD. This double-blind RCT showed that the 5-FU group had significantly better results in the treatment of KD than the intralesional steroid group. There can be significant side effects, such as ulceration, and pain. Hyperpigmentation can also occur, although this has been reported to improve after discontinuation of treatment.
Tretinoin
Tretinoin is a vitamin A–derived, nonpeptidic, small lipophilic molecule and has been used in the treatment of SD. This molecule works by inducing collagen synthesis and encouraging fibroblast activity. Dosage and duration of tretinoin cream varies in the literature, but the common doses used are 0.1%, 0.05%, or 0.025%, and it has been advocated this should be applied daily. There have been positive responses using this topical agent in striae rubrae and poor responses noted in striae albae. Mild irritation has been the most common side effect noted but this ceases when treatment ends. A double-blind, placebo controlled study (LOE-1) investigated the response of pregnancy-related abdominal striae to tretinoin cream (0.025%) applied for 7 months in 11 patients of varying ethnicities, including in dark pigmented skin. However, no differences were noted between the groups and no improvement in the SD in the treated group compared with the placebo group. The small sample size in this study may have contributed to these results.
A double-blind RCT (LOE-1) investigated the efficacy of topical tretinoin 0.1% compared with a vehicle cream on 26 white patients with SD. At 24 weeks, 80% of patients in the tretinoin group had an improvement in their SD compared with the vehicle group (8%). However, it is possible that these results should not be generalized to the population because only white patients were included, therefore this treatment may not be as effective for dark pigmented skin. Further trials are necessary in order to determine the effects of tretinoin on dark pigmented skin.
Acid Peels
Acid peel treatments are used to improve and smooth the texture of the skin using a chemical solution that causes the skin peel to stimulate dermal fibroblasts and enhance collagen synthesis. A concentration of 10% to 35% has been advocated as the optimal level because concentrations stronger than this can cause irreversible scar formation. In addition, hyperpigmentation can be a side effect following this treatment. Treatment can be applied for 1 to 2 minutes at each application and repeated monthly for up to 6 months. Glycolic acid has been used to enhance collagen synthesis. An increased epidermal thickness, elastin content, and reduced SD width following the use of glycolic acid has also been noted. Furthermore, a more recent double-blind controlled study (LOE-2) by Mazzarello and colleagues investigated the effect of glycolic acid on 40 patients of mixed ethnicities with SD. Striae rubrae were decreased in SD width and hemoglobin levels. Striae albae also showed an increase in melanin levels. However, there is no report of randomization or blinding, and explanation of how patients were allocated to each group is lacking. There is limited evidence for the effect of acid peels on SD, especially in dark pigmented skin.
Nonpharmacologic treatment options
There are various nonpharmacologic treatment options that are available to treat KD, HTS, and SD. The most current and commonly used treatments are discussed here ( Table 3 ).




