Fig. 13.1
External jugular vein in blue, sternocleidomastoideus muscle in red schematically drawn on the patient’s neck. Reproduction of a lithograph plate from Gray’s anatomy (Henry Gray, Anatomy: Descriptive and Surgical)
13.2 Pitfalls
Neck examination and identification of the major superficial vessels of the neck, external and anterior jugular vein, is important to avoid neck hematomas. The existence of a great anatomic variety commands nevertheless to introduce the needle just some millimeters under the skin plane.
Avoid too superficial injections, in particular in the epidermidis: In this case, small lumps might form that will disappear in a few days.
13.3 Bio-rejuvenation Technique for the Treatment of Neck and Décolleté
Bio-rejuvenation is a technique that uses generally low-viscosity hyaluronic acid to induce deep hydration of the skin and to stimulate the dermis to produce new matrix, improving skin structure and elasticity. The production of endogenous HA decreases drastically with age contributing to wrinkles formation. Injection of low-viscosity hyaluronic acid in the dermis enhances attraction of fibroblasts, macrophages, endothelial cells, and scavengers against radical-free damaged dermal proteins, thus inducing rejuvenation of the dermal layer.
13.3.1 Indications
Bio-rejuvenation can be used to improve skin trophism, texture, and elasticity of dermis of every anatomic area, but is usually practiced on the skin of the face, neck, décolleté, and hands.
Rejuvenation is particularly indicated in people who smoke and are exposed to sunlight for long periods of time.
13.3.2 Contraindications
In patients with coagulation defects or on current anticoagulant therapy the treatment is relatively controindicated. As with all injections in fact these subjects are at increasing risk of bleeding and Hematoma formation.
The filler should not be injected in areas that lack sufficient blood supply or have an infection or inflammation.
No injection should be done if the area has been previously treated with liquid silicone or other permanent fillers because a new injection could lead to inflammation or infection of the implants.
Any hypersensitivity to any components of the filler obviously constitutes a contraindication for the treatment.
Hypertiroidism for Grave’s Disease is a relative contraindication.
13.3.3 Operating Time
The procedure usually takes from 5 to 10 min.
13.3.4 Materials
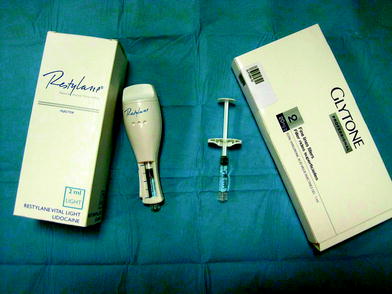
Examples of low viscosity HA are shown in the pictures.
13.3.5 Material Choice
In Europe
Glytone 1.
Belotero Soft.
Hydrate.
Jalupro.
Restylane vital light lidocaine 1 ml.
Restylane vital light lidocaine injector 2 ml.
Newest
Ialest
In Asia
Restylane vital light lidocaine 1 ml.
Restylane vital light lidocaine injector 2 ml.
In America
Restylane vital light lidocaine 1 ml.
Restylane vital light lidocaine injector 2 ml.
13.3.6 Methods
The procedure is described in Figs. 13.4, 13.5a, b, 13.6, 13.7, 13.8, 13.9a, b, 13.10a, b, and 13.11a, b.
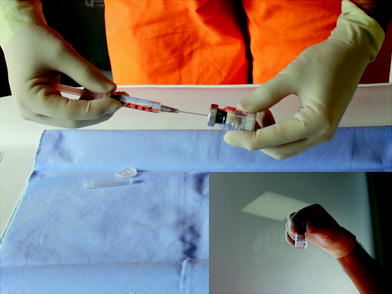
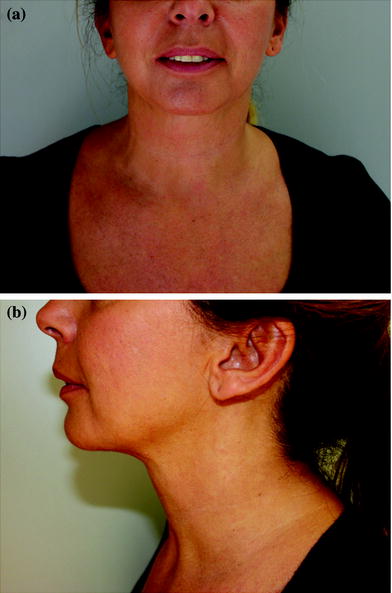



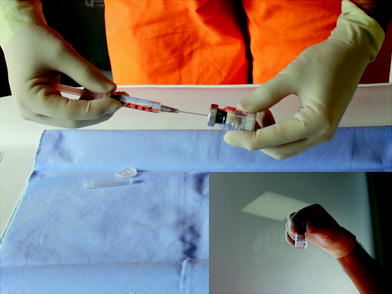
Fig. 13.4
Some products (i.e., Jalupro) are sold as sterile powders and need to be diluted. Here is shown the method of dilution of Jalupro. The sterile powder is diluted with 2.5 ml of the included solvent
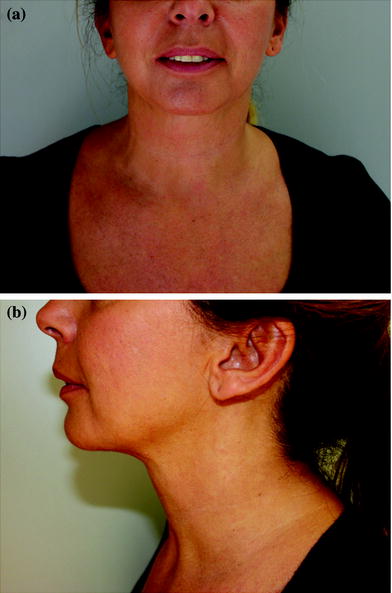
Fig. 13.5
a, b The patient neck and décolleté before the treatment

Fig. 13.6
The injection points on the patient’s skin are demonstrated. No local anesthesia is needed, except for a mild local anesthetic gel that could be applied 10–20 min before the treatment. Depending on the product, HA may or may not be mixed with an anesthetic solution. The presence of the anesthetic makes the treatment slightly more acceptable by the patient

Fig. 13.7
The ideal distance between different points of injection is 1 cm

Fig. 13.8
The HA solution is injected in the neck according with the picottage technique; pinching the skin between thumb and index of the free hand allows injection in the correct plane, i.e., superficial dermis and reduces the sensation of pain. The needle is inserted for 2–3 mm; the quantity of product injected is really small, about 0.05 ml or less