Microvascular Transfer of Anterolateral Thigh Flaps for Reconstruction of Head and Neck Defects
R. S. ALI
F.-C. WEI
EDITORIAL COMMENT
The ALT flap has become a workhorse flap because of its donor site, which is easily covered by clothing, and its flap tissue pliability. The reader must be aware of the variability of the blood supply.
The anterolateral thigh (ALT) flap was first described as a free cutaneous flap from the anterolateral aspect of the thigh, based on a septocutaneous perforator. In fact, the majority of ALT flaps are based on musculocutaneous perforators. As surgical techniques to dissect musculocutaneous perforators have developed, the ALT flap has been at the forefront of the “perforator flaps.” Rapid assimilation of the ALT flap into multidisciplinary head and neck practices attests to its versatility, based on characteristics such as: (a) a large cutaneous surface area; (b) multiplicity of tissue components that can be included in the flap (skin, fat, fascia, muscle, nerve, tendon); (c) freedom with which the tissue components can be separated on individual musculocutaneous perforators or septocutaneous vessels; (d) a long, wide-caliber pedicle; and (e) minimal donor morbidity.
INDICATIONS
General
The ALT flap, first described by Song et al. (1), is an ideal soft-tissue flap and is used in the reconstruction of many soft-tissue defects, including those following tumor resection, lower-limb trauma, or congenital deficiency.
Head and Neck
Indications for ALT flap use in head and neck surgery include the following: external face resurfacing, intraoral mucosal lining, soft-tissue volume replacement, palate and maxillary reconstruction, filling of dead space/sinus/cavity, reconstruction of the floor of the mouth, reconstruction of the tongue, reconstruction of the pharyngoesophagus, and scalp and skull-base reconstruction.
Buccal Mucosa
The cutaneous or fasciocutaneous ALT flap is a moderately thin, pliable flap that is ideal for resurfacing intraoral defects (Fig. 146.1). The long pedicle allows suitable inset of the ALT flap intraorally, with tunneling of the pedicle, to allow comfortable microvascular anastomosis to facial or cervical recipient vessels. The greater surface area of the ALT flap, compared
with the radial forearm flap, along with versatility in tissue design due to the often multiple perforators supplying the skin paddle, permits the resurfacing of larger defects, multiplanar defects (2), and bilateral defects (3).
with the radial forearm flap, along with versatility in tissue design due to the often multiple perforators supplying the skin paddle, permits the resurfacing of larger defects, multiplanar defects (2), and bilateral defects (3).
 FIGURE 146.1 Thin fasciocutaneous anterolateral thigh (ALT) flap, to resurface extensive defect of right buccal mucosa. Note large surface area and excellent contour of flap. |
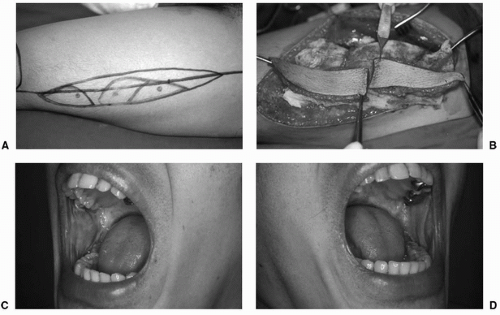
An ALT flap with more than one tissue paddle, based on widely separated perforators, is invaluable in the reconstruction of intraoral defects located in nearby but different sites or on different axial planes (2) (Fig. 146.2). More recently, the double-paddled ALT flap has evolved into harvesting two separate ALT flaps from one thigh, based on a single source vessel (3). This offers infinite degrees of freedom when positioning the flaps but requires the preparation of additional recipient vessels and additional microvascular anastomoses (Fig. 146.3).
Tongue Reconstruction
A thin fasciocutaneous or cutaneous ALT flap is ideal for reconstructing the partial glossectomy defect. The large cutaneous paddle permits resurfacing of an extensive surface area, and the relatively pliable flap can be molded to the three-dimensional contours of the tongue (Fig. 146.4).
Total glossectomy requires reconstruction with a flap of large cutaneous surface area and sufficient soft-tissue volume; the musculocutaneous ALT flap is excellent for reconstructing such defects. Incorporation of vascularized nerve in the ALT flap (anterior branch of the lateral femoral cutaneous nerve) confers the additional option of sensory reinnervation (4).
Pharyngoesophageal Reconstruction
A rapidly developing indication for use of the ALT flap is in pharyngoesophageal reconstruction. A wide fasciocutaneous or musculocutaneous ALT flap is raised with supplementary vascularized fascia and tubed to form a wide-bore, relatively rigid cylinder. The fascial layer augments the water-tight closure requisite to preparing the neo-pharyngoesophagus. The ALT flap can be raised simultaneously with tumor resection and recipient-site preparation; furthermore, the neo-pharyngoesophagus may be tubed and prepared with the flap still in situ on the thigh (Fig. 146.5). The free ALT flap can withstand extended ischemia time, compared with the free jejunal flap. There is growing evidence that postoperative complications are reduced by using the ALT flap, with concomitant superior functional outcome (5, 6).
Maxillary and Palatal Defects
Maxillary tumor resection often results in complex three-dimensional defects requiring multiple skin paddles, in addition to soft-tissue volume replacement and/or the need to separate compartments or pack sinuses/dead spaces. The ALT flap harvested with additional vascularized fascia and/or muscle is ideal for reconstructing such multidimensional defects alone or in combination with a bone flap (Fig. 146.6).
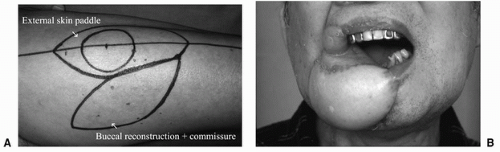
Through-and-Through Cheek Defects
A musculocutaneous ALT flap incorporating a portion of vastus lateralis provides excellent approximation of the bulk required to reconstruct a full-thickness cheek defect. The musculocutaneous ALT flap may be used to provide tissue bulk and external skin cover only. If the commissure is involved, the ALT flap may be folded around the commissure, to provide soft-tissue bulk and intraoral and extraoral skin cover (Fig. 146.7). If the commissure is not involved, an area of the ALT flap may be deepithelialized, and the flap “posted” into the oral cavity to provide intraoral coverage. Alternatively, a multiple-paddled ALT flap may be designed, which can be divided between widely separated perforators, and the separated tissue paddles inset to provide both intraoral and extraoral coverage (2).
Mandibular Defects
Oromandibular resections, resulting in significant volume loss, require a large bulky flap for adequate soft-tissue reconstruction. It has become established practice to reconstruct major oromandibular defects with a combination of two flaps: a bone/internal lining flap and a soft-tissue/external skin flap (7, 8). The ALT musculocutaneous flap has been extensively used in conjunction with the fibula osteoseptocutaneous (OSC) flap (Fig. 146.8). Both flaps can be harvested from the same lower limb, simultaneously with recipient-site preparation, in a multidisciplinary two-team approach. In recurrent or complex cases with limited local recipient vessels, the ALT perforator flap may be raised with a length of distal vessel, for use as a flow-through flap (9) or to “piggy back” a distal flap.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree