Microvascular Transfer of A Scapular/Parascapular Flap to The Cheek
T. BENACQUISTA
B. STRAUCH
EDITORIAL COMMENT
The use of scapular/parascapular flaps in this area is quite effective, not only for the correction of cheek skin deformities but also for the augmentation of subcutaneous tissue, especially in patients with Romberg’s disease or hemifacial microsomia.
The use of scapular and parascapular microvascular free flaps in cheek reconstruction is gaining more popularity (1, 2). These fasciocutaneous flaps have great versatility, allowing for good contour in many types of cheek defect and in cases of facial asymmetry. The flaps also have been used in the lower extremity and hand.
INDICATIONS
When used as fasciocutaneous flaps, these free-tissue transfers can fill in large cheek defects after trauma or tumor ablation. When deepithelialized, the flaps can be used in the correction of facial asymmetry. Advantages in these cases include reliability, appropriate bulk for the cheek, and lack of atrophy; the latter characteristic is not found in muscle flaps (1, 2). The color match of scapular and parascapular flaps may be troublesome when they are used with skin to fill in cheek defects, but the excellent contour that can be achieved may outweigh this shortcoming.
These free flaps not only provide sufficient bulk for cheek defects but have a quite constant and reliable pedicle, with a long pedicle length (7-8 cm) and wide-caliber vessels (2-3 mm). If bone is required in the reconstruction, the flap can be taken with the lateral border of the scapula. About 10 to 14 cm of bone can be harvested, depending on the amount required by the individual patient (3).
The major disadvantage is patient positioning during flap harvesting and closure of the donor site. Dissection of the vascular pedicle can be tedious because of the numerous muscular and bony branches that must be divided. Also, the donor site does not have a cutaneous sensory nerve, and there is no possibility for a sensate flap.
ANATOMY
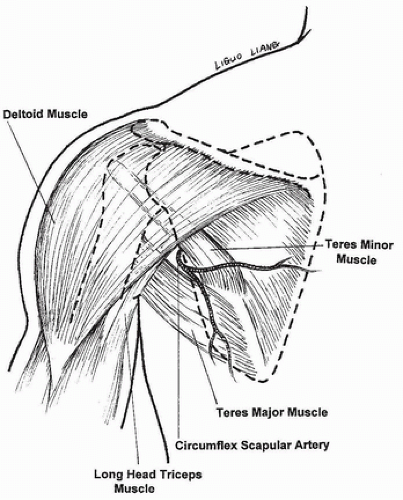
The cutaneous flaps are supplied by the circumflex scapular artery, which emerges from the scapular artery about 4 cm from its origin from the axillary artery (4). The circumflex
scapular artery emerges from the triangular fossa on the back at the edge of the lateral border of the scapula. This space is formed by the long head of the triceps and the teres major and minor muscles (5) (Fig. 139.1). The artery then terminates into two fasciocutaneous branches, one oriented transversely (scapular flap [6]) and one oriented vertically (parascapular flap [7]).
scapular artery emerges from the triangular fossa on the back at the edge of the lateral border of the scapula. This space is formed by the long head of the triceps and the teres major and minor muscles (5) (Fig. 139.1). The artery then terminates into two fasciocutaneous branches, one oriented transversely (scapular flap [6]) and one oriented vertically (parascapular flap [7]).
Before dividing into terminal branches, the circumflex scapular artery gives off several branches to the lateral border of the scapula in its superior portion. These branches supply the periosteum of the lateral border of the scapula and the attached muscles, thus allowing bone to be harvested with the flap.
FLAP DESIGN AND DIMENSIONS
Because of the orientation of the fasciocutaneous branches, the flaps can be designed as an ellipse, either horizontally (scapular flap) or vertically (parascapular flap). More commonly, the flap is designed in an oblique configuration between these two orientations to allow easier primary skin closure of the back and a better cosmetic result (Fig. 139.2).
Depending on the laxity of the skin, up to 10 cm of skin width can be harvested and closed primarily. Much larger widths can be harvested with a good blood supply; however, the resultant defect must be skin grafted, or preoperative skin expansion must be planned. The length that can be harvested depends on the patient’s size and can be up to 30 cm. Combinations of cutaneous flaps are possible for larger defects. Even the latissimus dorsi muscle, with or without a cutaneous paddle, may be harvested on the thoracodorsal pedicle if more bulk is necessary; this is rare for defects limited to the cheek. A combination of the two cutaneous territories as two separate paddles can be useful in through-and-through defects to provide both external skin coverage and inner-mouth lining.
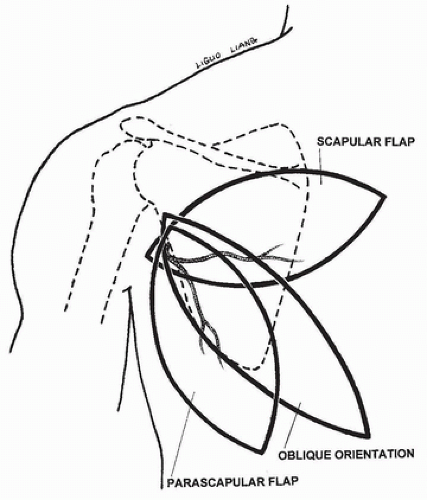 FIGURE 139.2 Dorsal aspect of the scapular area with schematic outlining of the various technical possibilities: scapular or parascapular flaps, oblique orientation or in combination.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|