56 Maximizing Graft Survival in Follicular Unit Excision: Incision and Extraction Phase
Summary
Keywords: FUE graft survival graft excision graft incision graft extraction FUE instruments
Key Points
•The physician should become knowledgeable and proficient in the device he or she selects to perform follicular unit excision (FUE) with.
•The incision process requires special attention to be paid to the follicle transection rate and graft quality.
•The graft extraction process is impacted by the depth of incision, and all extractions should be performed with the minimal amount of force exerted upon the follicle group.
56.1 Introduction
The incision aspect of follicular unit excision (FUE) is inherently a “blind” procedure, meaning once the process is initiated, there is very little the surgeon can do to alter the course and success of the individual incision. The process is also iterative, that is, feedback from previous incisions can be used to alter the approach for subsequent incisions. The follicular group has to be removed from the skin and this is usually performed by technicians. Their skill and adherence to the principles that decrease graft trauma can impact graft integrity and survival. The judgment and experience of the physician and staff, along with the chosen instrumentation and technique, will influence the risk of damage to the targeted follicles during the graft incision and extraction phases.
The first step to successful FUE is the adherence to principles specific to the basic incision instrumentation, that is, sharp, blunt, flat, etc., that allow for the greatest margin of safety to the follicles, which will minimize transection rates. The second is to separate the targeted follicles from the surrounding skin to the greatest degree possible that will minimize the force, and therefore trauma, required to remove the graft from the donor area. These two principles are at odds with each other as the goal of follicle protection implies a shallow incision and the goal of complete incision requires a deeper incision. It is in striking the balance between these goals using the incision instruments of his or her choice that the surgeon will be most successful.
This chapter will examine the variables in the incision and graft extraction process that impact graft survival, and suggestions for optimizing survival will be offered.
56.2 Incision Phase Factors
56.2.1 Proper Magnification
After teaching physicians for the past 14 years how to perform FUE, it is apparent that one of the most important factors in performing the procedure is the ability to properly visualize the target follicular group and to center the punch over the emerging hairs. If the operator cannot adequately perform this initial step, the chances of successfully performing FUE are greatly diminished. It is the author’s recommendation that high-quality surgical telescopes with a minimum of 4.5× magnification and a working distance of 18 to 25 cm be considered. Some physicians are using and prefer magnification as high as 6× or even 8×.
56.2.2 Follicle Transection
The most visible and obvious indication of follicle damage is the frank disruption of follicle integrity. The International Society of Hair Restoration Surgery (ISHRS) FUE Research Subcommittee has defined various forms of follicle disruption;1 for the purposes of this chapter, the term “transection” will include all forms of follicle disruption.
Follicle transection is a visible indication of follicle damage and reflects the need to adjust the incision technique. There is no absolute transection rate that is necessarily acceptable or unacceptable; however, it is generally felt that the operator should strive to minimize the rate, and rates less than 10% are acceptable. There are some physicians who attempt to cause a transection rate greater than 10 to 15% during an FUE procedure. The theory is that by leaving transected follicles behind in the donor area, some will grow back and camouflage the donor scars and create a more natural, homogeneous appearance.
Follicular transection and damage can directly impact follicle survival as shown in the study by Kim and Choi,2 indicating that when two-thirds of the lower follicle was intact and the upper two-thirds, the lower half, and the upper half were intact, the survival rates are 83, 65, 27, and 40%, respectively. In a more recent study by Devroye,3 in situ transections whereby the upper 40 to 70% of the follicular unit was removed, only 60% of the follicles grew back. This correlates with the study by Kim and Choi.
The fundamental difficulty of the FUE procedure is the uncertainty of the subcutaneous course, including angulation and direction, of the targeted follicles. Fig. 56.1 illustrates the follicle course variables. These uncertainties are mitigated differently based upon whether one is using a sharp or blunt incision system.
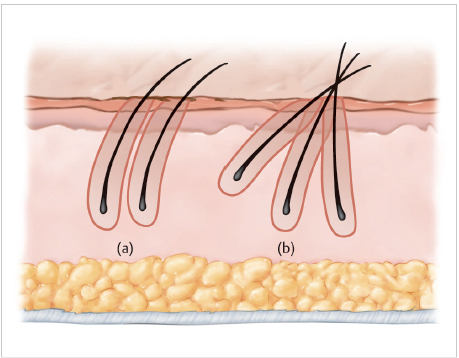
Fig. 56.1 The subcutaneous course of the follicles in the target group can be characterized by various degrees of (a) curl and (b) splay as seen in these illustrations.
Before discussing the details of the incision process, let us simplify matters by assuming there are two basic incision systems, sharp punch systems (SPS) and blunt punch systems (BPS). There are of course characteristics of each type that can change the performance characteristics. Examples of these in SPS are the location of the cutting edge (inner, outer, middle) or the configuration of the tip such as Cole’s Serrounded punch (Fig. 56.2). The common attribute of all SPS is a leading edge that can easily incise tissue.
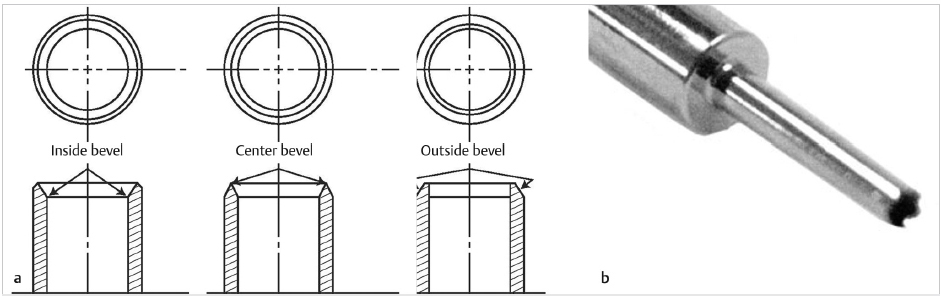
Fig. 56.2 (a) The cutting edge of sharp punches can be located in the outer, middle, or inner aspects of the punch wall. (b) The Cole Instruments Serrounded punch has a unique shape to the leading edge of the punch.
In the BPS category, there are two basic current types of punch configuration. The first is the Surgically Advanced Follicular Extraction (S.A.F.E.) System, first introduced in 2002, now with a flat, unsharp, tapered-tip design developed in 2011 and demonstrated in at the Second Mediterranean FUE Workshop in 2013. There is also a flat, nontapered tip introduced in 2016 by Dr. Jean Devroye,4 which features a “fluted” internal configuration. The common feature of both systems is a blunt or nonsharp leading edge.
Surgeons utilizing SPS, manual or powered, minimize transection rates by limiting the depth of punch penetration to the level at which the attachments of the epidermis and upper dermis (including the arrector pili muscle) have been severed and before significant follicle spay or curvature is encountered. This depth can be determined by sampling follicle groups from various locations on the scalp and measuring the levels at which either curvature or splay is encountered (Fig. 56.3) and then limiting the depth of incision to the appropriate level in that area. The limitation can be accomplished with either an adjustment in the chuck mechanism or a spacer/collar of some sort placed over the punch to limit insertion depth (Fig. 56.4). The primary goal of depth limitation is to prevent contact between the punch tip and the portion of the follicle that is at risk.
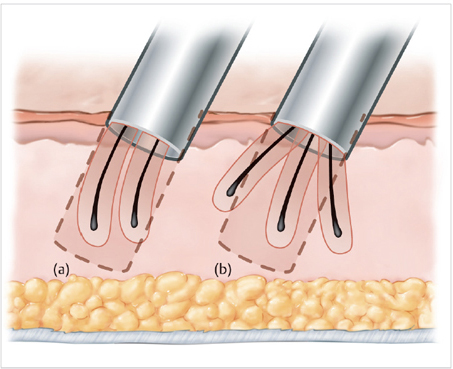
Fig. 56.3 (a, b) The determination of punch depth involves the analysis of the location where curl or splay will occur and adjusting the mechanism accordingly.
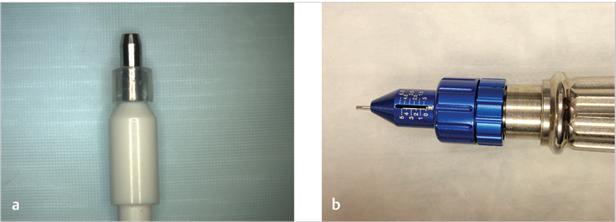
Fig. 56.4 Examples of depth limiting methods. Limitation can be accomplished (a) by spacers placed onto the punch or (b) by an adjustable mechanism on the device.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








