(1)
Swanson Center, Leawood, KS, USA
Abstract
Vertical mastopexy and breast reduction are the same operation, differentiated only by the resection weight. The vertical technique converts an elliptical defect to a straight-line closure. The length dividend increases projection and produces conical lower poles. Breast shape is improved, with less scarring than the Wise pattern. Nonvertical mammaplasties have geometric limitations, including nipple overelevation, boxiness, and reduced breast projection.
A medially based pedicle and intraoperative nipple siting are recommended. A short, inverted-T modification is used when the vertical scar extends below the level of the new (elevated) inframammary fold. A mosque dome often creates an inverted teardrop deformity.
Surprisingly, in 60% of women with ptotic breasts, both nipples are located at or above the breast apex, suggesting that the nipple slides with the breast in most cases rather than on it.
Vertical breast reduction effectively inverts the breast parenchymal ratio. The mean increase in breast projection after vertical mastopexy is 1.2 cm. Upper pole projection increases 0.5 cm. The increment in breast projection is about half as much after breast reduction – 0.6 cm on both sides. These modest increases confirm the clinical impression that mastopexy and reduction cannot duplicate the effect of a breast implant.
Nipple transposition on long pedicles is unnecessary. Using the vertical method, 80% of the upward nipple movement derives from breast mound elevation; only 20% comes from nipple repositioning on the breast mound. Short pedicles reduce the incidence of nipple loss to almost none. Persistent ptosis is the most common indication for reoperation. Adequate lower pole parenchymal resection is needed to prevent persistent ptosis. Skin-only mastopexies are usually ineffective.
Vertical mammaplasties facilitate combination (“mommy makeover”) procedures. Operating times for vertical mammaplasties, typically 1–2 h, are about an hour shorter than for inverted-T procedures, with less blood loss. Outpatient surgery is the norm.
Keywords
Vertical mastopexyVertical breast reductionMedially based pedicleIntraoperative nipple sitingMosque-domeNipple repositioningNipple transpositionMommy makeoversPersistent ptosisSkin-only mastopexyBreast augmentation , mastopexy, augmentation mastopexy, and reduction are all cosmetic procedures [1], notwithstanding the physical benefits of breast reduction and mastopexy [2]. Mastopexy and augmentation/mastopexy deserve close evaluation because these procedures have been a source of patient and physician dissatisfaction [3–5]. The author evaluated mastopexy and breast reduction as part of a comprehensive evaluation of cosmetic breast surgery that included a prospective outcome study [2], measurement studies [6–8], clinical study [9], and a study of published methods [10].
Failure to remove breast tissue from the lower pole – relying on tightening the skin envelope alone – is likely to provide no significant elevation of the lower pole, making the efficacy of a “skin-only” mastopexy questionable [6].
Today we recognize an overlap in indications for these procedures and even in physical benefits [2]. When a vertical technique is used, the mammaplasties are essentially the same, differentiated only by the resection weight [2, 6]. Recognizing that any cutoff is arbitrary, the author defines a breast reduction as a resection weight of 300 g or more from at least one breast [2, 6, 8, 9].
“Breast Lift”
Measurements confirm that the inframammary crease level moves up after a vertical mammaplasty [7]. Both vertical and inverted-T techniques can elevate the lower pole [10]. An underappreciated benefit of elevation of the lower breast pole is the appearance of a longer torso [9]. With the emphasis on fitness in our culture, and the frequent display of the midriff, this anatomic area takes on greater importance. However, upward mobilization of the superior border of the breast is more challenging [11]. “Autoaugmentation ” has not lived up to its billing (see Chap. 5) [10]. Breast implants are needed to substantially boost breast projection and upper pole projection [6, 12–14], providing the appealing illusion of breast mound elevation.
An underappreciated benefit of elevation of the lower breast pole is the appearance of a longer torso.
Mastopexy
The word mastopexy is derived from the Greek “mastos”, for breast, and “pexy,” for fixation. Commonly, mastopexy is understood to be synonymous with “breast lift.” Among plastic surgeons, a mastopexy has been traditionally understood to mean a skin tightening procedure [15], certainly for a “skin-only mastopexy .” However, the goal of a mastopexy is improvement in the shape of the breast, not simply tightening of its (elastic) envelope. In ptotic breasts, the lower pole needs to be reduced (i.e., parenchymal resection) to provide an aesthetic lower pole [6, 9, 16, 17] and avoid a “mastopexy wrecking bulge” [18].
No one denies that a breast reduction is also a mastopexy [10]. However, the reverse is true too. Measurements show that an effective mastopexy is also at least a small breast reduction [6]. Therefore, any distinction between mastopexy and breast reduction is arbitrary [10]. Indeed, mastopexy techniques evolved directly from reduction procedures [15]. We recognize the goals in optimizing breast shape are the same. Many authors acknowledge this false dichotomy and use the more inclusive term “mammaplasty.” [10] These procedures treat the same problem – breast sagging – with the only variable being the resection weight [10]. Therefore, mastopexy and breast reduction may be considered together.
Any distinction between mastopexy and breast reduction is arbitrary.
Fascial Sutures
The concept of using sutures [19, 20] in an attempt to suspend the breast on the pectoralis fascia and prevent descent is not new. Maliniac [21] used dermal strips. Almost half (42%) of the publications on the topic of mammaplasty advocate fascial sutures [10]. However, their efficacy has never been established and several surgeons recommend against their use [10, 22–25]. McKissock, in 1980 [25], observed: “The thought that suturing the inferior pedicle to the chest wall will suspend the breast for a prolonged period of time is naïve. It is a continuously recurring concept perpetuated by wishful thinking rather than unbiased observation.” Fascial sutures offer no advantage in breast projection or upper pole projection [10].
Mesh
One approach that has received renewed attention is the Góes procedure [26], a deepithelialized central mound dissection with an onlay of a mixed permanent/absorbable mesh. This technique does not produce an increase in breast projection or upper pole projection [10]. This method has been popularized recently with the introduction of longer-lasting absorbable mesh [27].
Periareolar Technique
The shortcomings of skin-only mastopexies are well-recognized [15, 28, 29]. Reports of “skin-only” periareolar mastopexies, including the “crescent mastopexy” [30], typically include patients treated simultaneously with implants [10]. Such patients are likely to benefit from the augmentation alone, making the benefit of the periareolar mastopexy questionable. The areola is often distorted [10]. A survey among board-certified plastic surgeons found periareolar techniques had the highest rate of surgeon dissatisfaction [5]. Furthermore, the periareolar operation has been disproportionately represented in malpractice lawsuits [31], accounting for 62% of mastopexy claims [32], despite being used as a single technique by only 6% of surgeons surveyed [5]. Measurements confirm that women treated with the periareolar technique have no significant benefit in breast projection, upper pole projection, lower pole elevation, breast convexity, or breast parenchymal ratio [10]. A conceptual problem with the periareolar technique is that it is usually a skin-only resection [33]. There is no glandular resection. Parenchymal resection is needed for lasting improvement in shape [10]. Not only is the wrong tissue being removed in a periareolar mastopexy, but it is also being removed from the wrong place – around the areola rather than from the lower pole.
Not only is the wrong tissue being removed in a periareolar mastopexy, but it is also being removed from the wrong place – around the areola rather than from the lower pole.
“No Vertical Scar” Method
The appeal of a periareolar or “donut” mastopexy is avoidance of a vertical scar. Generally, plastic surgeons prefer to avoid vertical scars on the face and body because vertical scars run against natural creases and are not concealed by them. The “no vertical scar” mammaplasty makes use of horizontal elliptical resection, similar to the Wise pattern, and a buttonhole for the new nipple/areola site [34, 35]. The Wise pattern produces a wide lower pole [10, 36]. This effect is exaggerated when no keyhole resection is used, producing a boxy breast shape (Fig. 6.1) [10, 36].
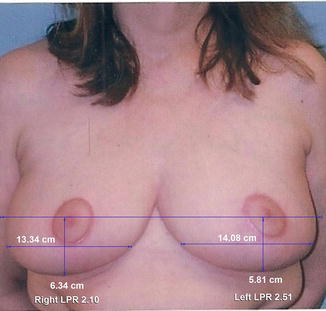
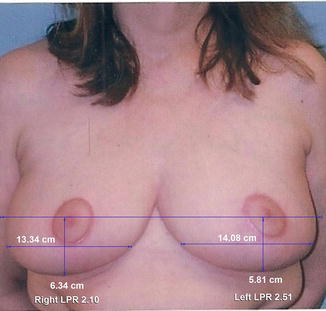
Fig. 6.1
Measurements of lower pole ratios in the example of a horizontal breast reduction provided by White et al. [36]. The patient is reportedly 50 years old and is shown 3 months after surgery. The mean lower pole ratio is 2.26, reflecting a boxy shape. LPR, lower pole ratio (Reprinted from Swanson [36]. With permission from Oxford University Press)
Regional Differences in Methods
It has been suggested that Brazilian and European surgeons, using “novel concepts,” perform better mastopexies and reductions than their North American colleagues [37, 38]. Indeed, mastopexy is a subject of particular interest in Latin America, particularly Brazil, and notable advances have come from Brazilian plastic surgeons [39, 40]. Pioneering European surgeons, particularly from France, Belgium, and Germany, are responsible for many of the innovations still in use today [16, 41–48]. However, in comparing results in terms of the measured variables, there appears to be no geographical advantage [10].
Significant regional differences in technique include [10]:
- 1.
Latin American and European surgeons prefer superior pedicles.
- 2.
American surgeons use the inferior pedicle more frequently and Europeans use it less often.
- 3.
North American surgeons use fascial sutures less often; Latin American and European surgeons use them more often.
- 4.
North American procedures usually do not incorporate autoaugmentation; Latin American surgeons use the concept more.
Measurements of Published Studies
Despite the authors’ claims , evaluation of 82 mastopexy and reduction articles reveals no significant increase in breast projection for any method (Fig. 6.2) [10]. On the contrary, nonvertical mammoplasties reduce breast projection. The mean change in breast projection for all procedures is a 0.7 cm decrease [10].
Fig. 6.2
Mean values for breast projection in 82 published studies. Preoperative (green) and postoperative (blue) (Reprinted from Swanson [10]. With permission from Wolters Kluwer Health)
Similarly, no published mastopexy/reduction technique significantly increases upper pole projection (Fig. 6.3). The Wise pattern with a superior or medial pedicle decreases upper pole projection by 0.8 cm, on average.
Fig. 6.3
Mean values for upper pole projection in 82 published studies. Preoperative (green) and postoperative (blue) (Reprinted from Swanson [10]. With permission from Wolters Kluwer Health)
Although the differences did not reach significance in the author’s study of combined results from numerous surgeons, several individual studies did achieve a boost in breast projection and upper pole projection [17, 49–51]. All used the vertical technique.
The breast parenchymal ratio (upper pole area/lower pole area) increases significantly for Wise pattern, superior or medial pedicle mammaplasties, and for vertical mammaplasties. This ratio is not increased significantly by inverted-T, central pedicle, and periareolar mammaplasties (Fig. 6.4) [10].
Fig. 6.4
Mean values for breast parenchymal ratio in 82 published studies. Preoperative (green) and postoperative (blue) (Reprinted from Swanson [10]. With permission from Wolters Kluwer Health)
All mammaplasty methods, with the exception of the periareolar and inverted-T, central mound dissections, significantly elevate the lower pole (the lowest point on the breast) and nipple (Figs. 6.5 and 6.6). Nipple overelevation was found in 42% of publications, with no significant difference between open and closed nipple siting techniques. None of the photographs showed a patient with a postoperative nipple level below the level of maximum postoperative breast projection [10].
Fig. 6.5
Mean values for lower pole level (the lowest point on the breast) in 82 published studies. Preoperative (green) and postoperative (blue) (Reprinted from Swanson [10]. With permission from Wolters Kluwer Health)
Fig. 6.6
Mean values for nipple level in 82 published studies. Preoperative (green) and postoperative (blue). Positive values indicate distances below the breast apex and negative values represent distances above the breast apex (Reprinted from Swanson [10]. With permission from Wolters Kluwer Health)
Shape Advantages of the Vertical Technique
The vertical technique lengthens the lower pole distance (the length along the lateral curve from the plane of maximum postoperative breast projection to the posterior breast margin [52]), a measure of breast constriction [8], by converting an elliptical defect to a vertical straight-line closure (Fig. 6.7) [6, 9, 10, 22, 40, 53]. The lower pole is elevated and the length dividend increases projection [6, 8, 9]. By comparison, constriction of the lower pole, reduced breast projection, and increasing frontal boxiness, consequences of the inverted-T technique, are aesthetic problems that do not resolve [6, 8, 10].
Fig. 6.7
Illustration of resection patterns for the inverted-T, vertical, periareolar, and inframammary techniques . The breast dimensions are drawn to the actual mean values determined from a study of 82 publications [10]. The arrows depict the movement of skin flaps and the nipple. (Above) In the inverted-T technique, the horizontal tissue resection causes lengthening in a horizontal direction at the expense of projection. Nipple transposition is used to counter the downward movement of the skin flaps. (Second row) In the vertical technique, the vertical limb length is increased, pushing the nipple up, with simultaneous reduction of width. (Third row) The periareolar technique does not significantly affect breast shape. (Below) Without a keyhole resection, the widening effect is more pronounced in techniques that avoid a vertical scar (Reprinted from Swanson [10]. With permission from Wolters Kluwer Health)
The vertical technique lengthens the lower pole distance (the length along the lateral curve from the plane of maximum postoperative breast projection to the posterior breast margin), a measure of breast constriction, by converting an elliptical defect to a vertical straight-line closure.
Surgery
The surgical approach for a mastopexy or breast reduction is the same as for an augmentation mastopexy or breast reduction plus implants, without the implant insertion. A vertical mammaplasty is performed using a medially based pedicle [24] and intraoperative nipple siting [6, 8, 9]. A mosque-dome or keyhole preoperative pattern is not used. A vertical resection is performed. The nipple/areola site is determined after creation of the new breast mound. An inverted-T modification is used in patients in whom the vertical scar extends below the level of the new (elevated) inframammary crease. Videos demonstrating a vertical breast reduction in combination with implant insertion are available at the Plastic and Reconstructive Surgery Global Open website: http://journals.lww.com/prsgo/Pages/videogallery.aspx?videoId=23&autoPlay=true. The videos include preoperative marking, details of the surgery and anesthesia, and follow-up 24 h after surgery.
The author performs surgery on outpatients in a state-licensed ambulatory surgery center using total “SAFE” (spontaneous breathing, avoid gas, face up, extremities mobile) intravenous anesthesia [54]. No muscle relaxation is used so as to preserve the calf muscle pump [55]. Patients are also monitored for venous thromboembolism using ultrasound surveillance as part of a clinical trial in progress [56]. The mean operating time for a vertical mastopexy is 106 min, versus 121 min for a breast reduction [9]. The videos include preoperative marking, details of the surgery and anesthesia, and follow-up 24 h after surgery.
Measurements of Vertical Mastopexy and Reduction: Author’s Patients
Preoperative Nipple Level
Surprisingly, in women with ptotic breasts who undergo mastopexy, augmentation mastopexy, or reduction procedures, the overall mean preoperative nipple displacement (the vertical distance between the nipple and the level of maximum breast projection [52]) is <1 cm on both sides [6]. In 75% of breasts the right nipple is positioned within 1 cm or above the level of maximum preoperative breast projection (Fig. 6.8), and in 60% of women with ptotic breasts both nipples are located at or above the breast apex before surgery [6]. These findings suggest that with breast hypertrophy and ptosis the nipple slides with the breast in most cases rather than on it. The nipple goes along for the ride, so to speak. It is, after all, an ectodermal appendage with the same embryonic origin as the rest of the breast [57]. The pathology is thought to be a weakening of the fascial ligamentous support system of the breast [51], with descent of the parenchyma in an elastic skin envelope, not a skin “brassiere” at all [6].
Fig. 6.8
Illustration of the distribution of right nipple levels relative to the level of maximum preoperative breast projection (nipple displacement) in 162 women with ptosis presenting for a mastopexy, augmentation mastopexy, or reduction. The right nipple was located within 1 cm of the level of maximum preoperative breast projection (MPre) in 75% of patients (Reprinted from Swanson [6]. With permission from Wolters Kluwer Health)
With breast hypertrophy and ptosis the nipple slides with the breast in most cases rather than on it. The nipple goes along for the ride, so to speak.
Comparisons
Vertical mastopexy and reduction reduce breast areas approximately 12.5% and 25% respectively (Fig. 6.9). Vertical breast reduction increases the upper pole area 15% and decreases the lower pole area 50%, on average. Volume varies as the square of area. Therefore, breast reduction reduces volume 44% on average. Vertical breast reduction effectively inverts the breast parenchymal ratio (upper pole area/lower pole area). Most of the gain in breast parenchymal ratio derives from lower pole reduction as opposed to upper pole filling [6].
Fig. 6.9
Right breast area before (green) and after (blue) surgery. Volume changes vary as the square of area changes (Reprinted from Swanson [6]. With permission from Wolters Kluwer Health)
Most of the gain in breast parenchymal ratio derives from lower pole reduction as opposed to upper pole filling.
The mean increase in breast projection after vertical mastopexy is about 1.2 cm (Fig. 6.10). Upper pole projection increases about 0.5 cm. The increment in breast projection is about half as much after breast reduction – 0.6 cm on both sides, likely because of the greater reduction in volume (Fig. 6.11). Upper pole projection increases are similar to mastopexy (<1 cm). These modest increases confirm the clinical impression that mastopexy and reduction cannot duplicate the effect of an implant in creating upper pole fullness [12, 13].
Fig. 6.10
Breast shape before (left) and after (right) vertical mastopexy with a medial pedicle. Breast projection and upper pole projection are modestly increased. The elliptical shape of the lower pole is tightened to a semicircle on both frontal and lateral views. The lower pole is elevated. The lower pole ratio (LPR) measures less than 2.0 on both sides. The upper pole contour remains linear after surgery. The areola diameter is reduced approximately 1 cm. These mammographs were created based on mean breast measurements among study patients. MPost maximum postoperative breast projection, BPR breast parenchymal ratio, BME breast mound elevation (Reprinted from Swanson [6]. with permission Wolters Kluwer Health)
Fig. 6.11
Breast shape before (left) and after (right) vertical breast reduction. Breast projection and upper pole projection are modestly increased (<1 cm). The lower pole level is elevated 5 cm. The breast parenchymal ratio is effectively inverted, from 0.65 to 1.60. On average, the nipples are slightly (and not ideally) overelevated. The areola diameters are reduced over 2 cm, to a diameter <5 cm deemed desirable by patients. The upper pole contour describes a mild ogee curve before surgery and is linear after surgery. These mammographs were created based on mean breast measurements among study patients. MPost maximum postoperative breast projection, LPR lower pole ratio, BPR breast parenchymal ratio, BME breast mound elevation (Reprinted from Swanson [6]. With permission from Wolters Kluwer Health)
These modest increases confirm the clinical impression that mastopexy and reduction cannot duplicate the effect of an implant in creating upper pole fullness.
The lower pole ratio (lower pole width divided by length) is a measure of the boxiness of the lower poles, with values much over 2.0 appearing boxy [52]. The mean postoperative lower pole ratio after vertical mammaplasty (combining mastopexy and reduction) is slightly under 2.0, measuring 1.97 on the right and 1.95 on the left [6].
Areola Diameter
Breast reduction patients tend to have large areolae, averaging 7.1 cm in diameter [6]. The areolar diameter decreases approximately 1.0 cm after mastopexy and 2.4 cm after breast reduction [6]. At least one nipple was overelevated in 30% of the author’s patients. Patients do not favor wide areolae [6]. Despite using a 39 mm areola marking ring and an intraoperative positioning technique that theoretically reduces skin tension around the areola [10], areola diameters for the combined group of vertical mastopexies and reductions averaged approximately 5 cm after surgery, at the outside margin of the range deemed “okay” by patients [6]. For this reason, an areola marking device with a diameter ≤39 mm is recommended, allowing for a 1 cm stretch after surgery [6].
An areola marking device with a diameter ≤39 mm is recommended, allowing for a 1 cm stretch after surgery.
Both vertical mastopexy and reduction significantly elevate the lower pole level, about 3 cm after mastopexy and 5 cm after breast reduction [6]. Vertical mammaplasty effectively elevates the breast mound (level of maximum breast projection), about 4.7 cm after mastopexy and 5.6 cm after reduction [6]. The nipple moves up on average 5.8 cm after mastopexy and 7.5 cm after breast reduction. These measurements suggest that 80% of the upward nipple movement derives from breast mound elevation; 20% is from nipple repositioning on the breast mound (Fig. 6.12) [6]. This figure is calculated by dividing breast mound elevation by nipple elevation.
Fig. 6.12
Comparison of inverted-T, inferior pedicle reduction (above) and vertical, medial pedicle reduction (below) techniques . The inverted-T, inferior pedicle technique relies completely on transposition of the nipple with respect to the surrounding breast tissue, with no assist from breast mound elevation because the pedicle remains attached at the level of the inframammary crease. The nipple is overelevated despite limiting the vertical limb length to 5 cm. The vertical, medial pedicle technique benefits from breast mound elevation caused by closure of the vertical ellipse, which raises the pedicle, including its base. On average, breast mound elevation provides 80% of the superior nipple movement in vertical breast reduction . Pedicle length is minimized. Diagrams are drawn to actual mean measurements for these procedures (Reprinted from Swanson [6]. With permission from Wolters Kluwer Health)
These measurements suggest that 80% of the upward nipple movement derives from breast mound elevation; 20% is from nipple repositioning on the breast mound.
Comparison of Inverted-T, Inferior Pedicle and Vertical Breast Reduction: Author’s Patients
The author’s study of published mammaplasties revealed shape deficiencies of the Wise pattern, regardless of pedicle orientation [10]. However, this study combined results from many different surgeons. It also evaluated only published photographs, which are likely to represent favorable results.
In order to compare these methods in the absence of confounders, the author undertook a comparative study of his own breast reduction patients [8]. The author performed all mammaplasties using the inverted-T, inferior pedicle method before 2002, and all subsequent mammaplasties with the vertical method, making possible a Level 3 study comparing a historical cohort with a prospective cohort. This study design avoided selection bias based on breast size or other considerations. An inclusion criterion was at least 3 months’ follow-up. Longer follow-up times are preferred. However, they come at the cost of lower inclusion rates [8]. At 3 months, swelling has sufficiently resolved so as not to represent an important confounding factor [6]. Subsequent shape changes are usually minimal [58].
In order to select most representative patients, those patients from each group with the lowest z-scores were chosen for publication (Figs. 6.13 and 6.14). These patients had, overall, the most average measurements among the patients in each study group. Figures 6.15 and 6.16 compare mean shape values depicted in mammographs for the two methods [8].
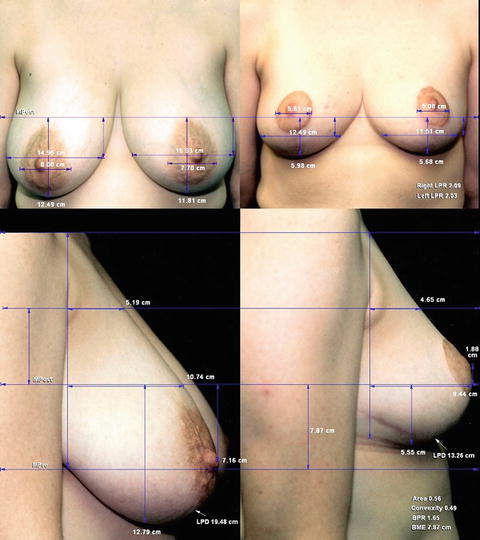
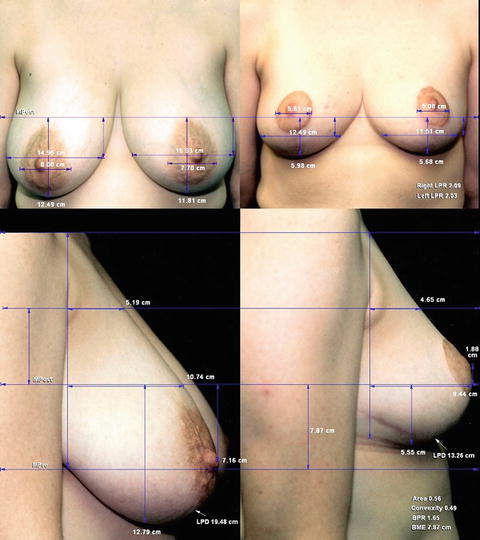
Fig. 6.13




Orientation-matched views of the inverted-T reduction patient with the most average (lowest z-score) breast measurements, a 37-year-old woman before (left) and 22 months after (right) an inverted-T, inferior pedicle breast reduction. Resection weights: right breast, 440 g; left breast, 510 g. Breast projection and upper pole projection are decreased. The lower pole distance is 6.2 cm shorter after surgery. The upper pole contour is linear before surgery and slightly concave after surgery, with an upturned nipple. MPost maximum postoperative breast projection, MPre maximum preoperative breast projection, LPD lower pole distance, LPR lower pole ratio, BPR breast parenchymal ratio, BME breast mount elevation (Reprinted from Swanson [8]. With permission from Wolters Kluwer Health)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree