53. Mastopexy
Joshua Lemmon, Smita R. Ramanadham, James Christian Grotting
NATURAL HISTORY AND CLASSIFICATION1,2
BREAST CHANGES: MULTIFACTORIAL
■ The amount of breast parenchyma changes with age, body weight, pregnancy, and hormonal changes.
• The skin envelope is stretched when the parenchyma enlarges.
• Supporting ligaments and ductal structures are also stretched.
• Ptosis results when the parenchymal volume decreases, and the skin envelope and supporting structures do not retract.
► As a consequence, the breast assumes a lower position on the chest wall, and the youthful breast contour is lost.
REGNAULT CLASSIFICATION1 (Fig. 53-1)
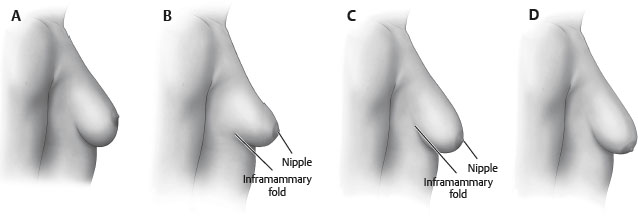
Fig. 53-1 Regnault classification of breast ptosis. A, Pseudoptosis. B, Grade I ptosis. C, Grade II ptosis. D, Grade III ptosis.
■ Describes ptosis by the relative position of the nipple-areola complex (NAC) and the inframammary fold
• Grade I ptosis (mild ptosis)
► NAC is at the level of the inframammary fold.
• Grade II ptosis (moderate ptosis)
► NAC lies below the level of the inframammary fold, but remains above the most dependent part of the breast parenchyma.
• Grade III ptosis (severe ptosis)
► NAC lies well below the inframammary fold and at the most dependent part of the breast parenchyma along the inferior contour of the breast.
• Pseudoptosis or glandular ptosis
► NAC is above or at the level of the inframammary fold, but most of the breast parenchyma has descended below the level of the fold.
► Nipple-to-inframammary fold distance has increased.
INDICATIONS AND CONTRAINDICATIONS3–5
INDICATIONS
■ Women who desire an improvement in breast contour without a change in volume ■ Women who seek a more lifted, “perky,” youthful breast appearance and aim to correct upper pole deflation, ptosis of the areolar complex and breast tissue, and laxity of skin envelope
CONTRAINDICATIONS
■ Active smoking
■ Women who desire volume change
PREOPERATIVE EVALUATION2, 6
HISTORY
■ Age: Involution of breast after menopause
■ Breast history: Lactation, pregnancy changes, size changes with weight loss/gain, tumors, previous procedures, family history of breast cancer, recent mammogram
■ Patient goals
■ Medications, including psychotropic, oral contraceptive, and hormone replacement6
MEASUREMENTS
■ Sternal notch-to-nipple distance: Allows detection of asymmetry in nipple position
■ Nipple-to-inframammary fold distance: A measurement of the redundancy of the lower pole skin envelope
■ Classification of ptosis severity (see Fig. 53-1)
OTHER CONSIDERATIONS
■ Breast position on chest wall: Patients with low breast position without significant ptosis will not benefit from mastopexy.7
■ Skin quality and amount: Presence of striae reflects the inelastic quality of affected skin; degree of skin laxity
■ Parenchymal quality: Fatty, fibrous, or glandular parenchyma and overall volume
■ Areolar shape and size: Areola are often stretched and large with asymmetries.
PHOTOGRAPHS
■ AP, lateral, and oblique photographs should be obtained (see Chapter 3).
PATIENT EXPECTATIONS
■ Breast size
• Mastopexy techniques combine small amounts of parenchymal resection (<300 g traditionally in literature3) and redistribution with reduction of the skin envelope— this can result in a reduction in breast size.
► Average decrease of one cup size postoperatively: Important in patient counseling.3
• Many patients desire restoration of upper pole fullness, which may necessitate the placement of an implant simultaneously.
► Mastopexy, augmentation-mastopexy, and reduction all increased breast and upper pole projection with significantly greater boost when implants were combined with mastopexy.8
• Volume-deficient patients may often require augmentation-mastopexy as well7 (see Chapter 54).
■ Scar position
• Mastopexy procedures trade scars for improved contour.
• Patients should be informed in detail preoperatively about scar placement and scar quality.
■ Other considerations
• Thorough patient education regarding procedural complications, use of drains, and recurrence of ptosis are essential components of preoperative preparation.
INFORMED CONSENT
Recommend items to be included in the informed consent:
■ A general description of the procedure and location of incisions and the potential need for placement of drains
■ A sufficient description of potential risks
• Bleeding and hematoma
• Infection
• Delayed healing and wound separation
• Change in nipple and skin sensation
• Potential changes in breast-feeding
• Asymmetry and poor cosmetic result
• Poor scar quality
TIP: Postoperative scars are a frequent source of litigation; therefore they are an essential component of the informed consent process. However, breast shape should not be compromised to reduce the scar burden.
MASTOPEXY TECHNIQUES
■ Historically, mastopexy was based on primary skin excision; however, since the mid-1990s, internal shaping of tissue using various supportive materials or parenchymal pillars has also been emphasized.4
■ Technique depends on degree of ptosis.
PERIAREOLAR TECHNIQUES
GENERAL
■ Incisions are made and closed around the areola.
■ Scars are therefore camouflaged at the areolar-skin junction.
PATIENT SELECTION
■ Useful with mild and moderate ptosis
■ Skin quality should be reasonable without striae, and parenchyma should be fibrous or glandular.
TECHNIQUES
■ Simple periareolar deepithelialization and closure
• Breast parenchyma is not repositioned; therefore only useful with mild ptosis
• Permits nipple repositioning
• Limited ellipitical techniques can elevate the NAC approximately 1-2 cm.2
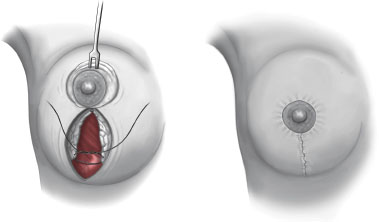
■ Benelli technique9 (Fig. 53-2)
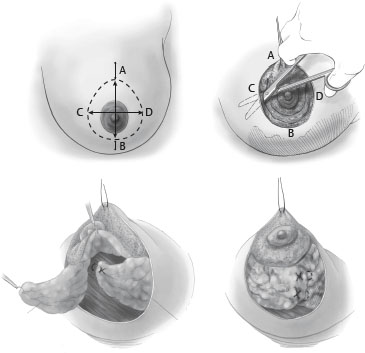
Fig. 53-2 Benelli periareolar mastopexy. Markings, undermining, and parenchymal coning.
• A periareolar technique that can be applied to patients with larger degrees of breast ptosis
• Allows parenchymal repositioning
• Areolar sizers are used to mark the new areolar diameter, and a wider ellipse is marked to reposition the NAC and resect redundant skin envelope.
• Undermining separates the breast gland from the overlying skin.
• The breast parenchyma is then incised leaving the NAC on a superior pedicle.
• Medial and lateral parenchymal flaps are mobilized and crossed or invaginated in the midline, narrowing the breast width and coning the breast shape.
• The periareolar incision is closed in a purse-string fashion with permanent suture.
■ Other periareolar techniques
• Variations on the technique discussed above include use of mesh to support the parenchyma10 or routine use of breast implants to reduce the amount of skin resection required.11,12
ADVANTAGES
■ Short scar
■ Scar position camouflaged at border of pigmented areola and nonpigmented skin
DISADVANTAGES
■ Scar and areolar widening occur frequently.
■ Breast projection can be flattened.
■ Purse-string closure results in skin pleating that takes several months to resolve.
SENIOR AUTHOR TIP: If periareolar purse-string suture remains palpable, it can be removed in a simple office-based procedure after 6 weeks.
VERTICAL SCAR TECHNIQUES
GENERAL
■ Vertical mastopexy techniques are variations of vertical reduction mammaplasty techniques.
■ Incisions are closed around the areola and inferiorly toward the inframammary fold.
■ Techniques rely on parenchymal support inferiorly to narrow and cone the breast.
PATIENT SELECTION
■ Techniques can be applied to patients with all degrees of ptosis. TECHNIQUES
■ Vertical mastopexy without undermining (Lassus)13 (Fig. 53-3)