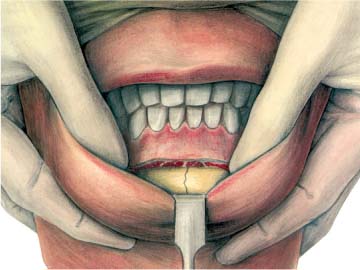
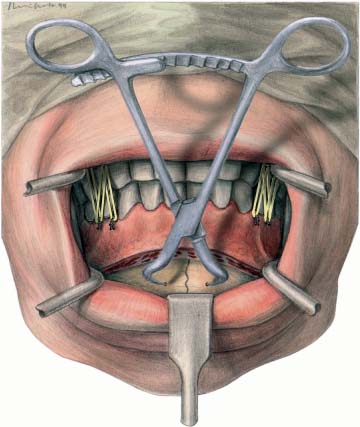
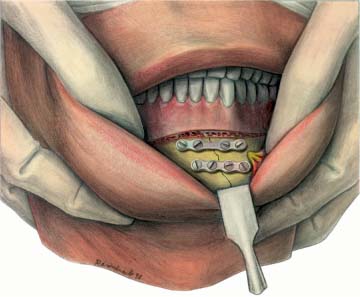
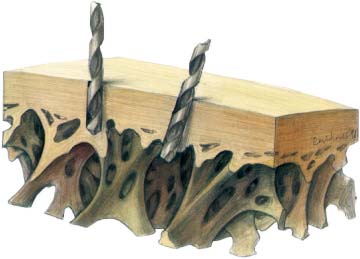
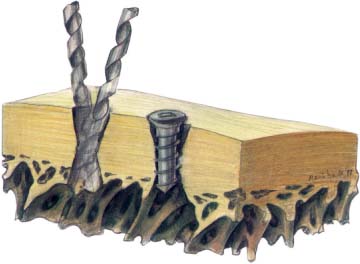
7 Mandibular Fractures Including Atrophied Mandible The experimental and clinical investigations of Champy et al. (1976a, b, 1977) established the biomechanical preconditions and the surgical basis for successful miniplate osteosynthesis. The most important result of Champy’s investigations was the determination of an ideal osteo-synthesis line in the biomechanically favorable region at the base of the alveolar process. The strength of the plate and the diameter of the monocortical screws were adapted to the biomechanical demands of the mandible. Using these results, many companies developed osteosynthesis systems. The use of miniplate osteosynthesis in fractures of the horizontal mandible has become a generally accepted procedure. Nevertheless, the mechanical characteristics of the miniplate systems produced by different firms can vary widely. The technical procedure is the same for all fractures of the mandible; the following points should be observed. The treatment of all mandibular fractures should take place, if at all possible, during the first 12 hours after the accident (Champy and Lodde, 1976). There are various reasons for this recommendation, in particular the relationship between delayed treatment and increase in the rate of infection (Gerlach and Pape, 1988). Most mandibular fractures require intubation anesthesia. Our own experience showed that miniplate osteosynthesis under local anesthesia with premedication is also possible and saves staff time. The main indication for the use of local anesthesia is a simple or double fracture in the front part of the mandible or in the area of the wisdom teeth. Local anesthesia may also be favored in patients who have a poor general medical condition that is prejudicial to intubation anesthesia. Approximately 40 % of patients can be operated on using local anesthesia (Walz et al., 1996). Fig. 7.1 Manual repositioning of the fracture parts. The feasibility of manually repositioning dislocated mandible fragments should be checked. If correct occlusion to the upper jaw can be achieved without difficulty, inter-maxillary fixation is not required. However, where problems arise, for instance in multiple fractures, preoperative splinting and intermaxillary fixation are necessary. With the help of a capable assistant, the experienced surgeon should be able to reposition many simple fractures manually (Fig. 7.1). An inexperienced surgeon, however, should certainly start with splinting of the upper and lower jaw by the eyelet method of intermaxillary fixation (Ivy, 1922; Obwegeser, 1952; Stout, 1942). Remember that each fractured fragment should be fixed individually to the upper jaw. A splint bridging the fracture makes correct occlusal reduction impossible. Fig. 7.2 Fractured jaw. Fixation with a bone clamp and intermaxillary fixation (for details of treatment, see Figs. 7.15, 7.16). Fig. 7.3 Fractured jaw. Reposition and fixation by two four-hole plates. To avoid dehiscences, the rules for incisions, as described in Chapter 5 on Surgical Approaches, must be observed. The incision line should be 5 mm below the level of the attached gingiva (Champy and Lodde, 1976). Occasionally, a marginal rim incision is indicated. The length of the incision must allow free access to the fracture line and the surrounding area. If two plates are to be applied in the front area, an extension of the incision is necessary. The normal four-hole plate with screws of 5–7mm diameter is preferred in most cases. Alternatively, four-hole plates with bar or six-hole plates with or without bar may be indicated for anatomical reasons (e. g., where there is involvement of the foramen mentale, danger of injury to root tips, or there are comminuted fractures). After exposing the fracture line, the fragments are reduced manually. In difficult cases, a bone hook may be applied to the proximal fragment and countertraction applied simultaneously to the anterior fragment to facilitate reduction and interdigitation of the fracture ends. The use of bone clamps for the temporary immobilization of fragments simplifies the adaptation and fixation of a miniplate (Fig. 7.2). Following reduction, the occlusion is checked and secured by hand adaptation or through simple intermaxillary wiring. With modeling pliers and modeling lever, the osteosynthesis plate has to be precisely adapted to the outer cortical surface at the level of the osteosynthesis line. After drilling a hole, the screw is inserted and only then is the next hole drilled. After the plate has been fixed with two screws on one side of the fracture, care has to be taken before drilling the first hole in the other fragment, so that an optimal adaptation of the fragments can be achieved. Every plate must be fixed with at least two screws in each fragment. After inserting one or more screws, no attempts should be made to improve the adaptation of the plate, since this would result in the loosening of screws already inserted. Instead, the plate should be removed and adapted correctly. If a screw fails to gain a secure grip close to the fracture line, the position of the plate should be altered; alternatively, a plate with bar can be used (Fig. 7.3). In comminuted fractures or where there are detached triangular pieces of bone, longer plates with six or more screws should be used (see Fig. 7.20). The drill should, if possible, be held perpendicular to the bony surface (Fig. 7.4). An angulation up to 30° is allowed (Champy and Lodde, 1976), but it must be strictly monoaxial. Any change in the drilling angle during the drilling procedure results in a conical drill hole that fails to guarantee a firm grip on the screws (Fig. 7.5). The normal thickness of the cortical layer is 3 mm, and since the screw threads lie approximately 1 mm apart, screw fixation depends on three screw threads. A conical drill hole might reduce the grip of the screw to one or two threads. Excessive tightening of the screw produces microfractures within the drill hole (Fig. 7.6). When the osteosynthesis has been completed, stability and occlusion should be checked with the lower jaw in motion. After replacing the loosened soft tissue, the mucosa should be sutured, together with the periosteum. Fig. 7.4 Drill position. Fig. 7.5 Excentric drill.
Introduction
Technique
Time of Treatment
Anesthesia
Re-establishment of Occlusion
Gingiva Incision
Miniplate Choice
Miniplate Osteosynthesis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree