Chapter 58 Management of burn injuries of the perineum
![]() Access the complete reference list online at http://www.expertconsult.com
Access the complete reference list online at http://www.expertconsult.com
Introduction
Burns of the perineal area are quite uncommon even though the lower trunk and the lower extremities are vulnerable to burn injury. Alghanem et al. reported the incidence of perineal burns to be about 12/1000 admissions, more than 20 years ago.1 While the occurrence of perineal burns has remained fairly consistent at 1.0–1.5% at our hospital, 35 children underwent genito-perineal reconstruction, out of 1133 presentations between 2002 and 2009. An increase in the number of children who have survived extensive burns of a total body surface area (TBSA) involvement of more than 40%, could account for the increase in the number of children requiring secondary reconstruction.
Management of burns of the perineum during acute phase of injury
A conservative approach is used to manage perineal burns.1,2 The perineal area is cleansed daily and the wound is covered with antibiotic dressing. The urethral tract is stented with an indwelling Foley catheter as it is also used to decompress the urinary bladder. The perineal area is neither splinted nor braced. The thighs are maintained at 15 degrees of abduction using a wedge splint to minimize contracture of the hip joint. The extent of burns is allowed to demarcate in time and the wound is often left to heal spontaneously. A non-healing wound is managed with the use of a partial-thickness or a full-thickness skin graft. On rare occasions, a skin flap may be mobilized from the area adjacent to reconstruct defects consequential to full thickness skin loss of the penis and the scrotum.
Burns of the penis
Burn injuries limited to the penis, though possible, are quite rare (Fig. 58.1). Concomitant involvement of the penis with burn injuries of the lower trunk and the perineal area, on the other hand, is quite common. The initial regimen of patient management, in addition to resuscitative measures, consists of wound care and urethral stenting. An indwelling Foley catheter of appropriate size is inserted into the urinary bladder to stent the urethral tract and at the same time, to monitor the urinary output. The catheter is removed once the swelling around the penile shaft has subsided and status of the wound becomes delineated. No attempt is made to debride the burned wound early. Instead, it is allowed to demarcate and is often allowed to heal spontaneously.
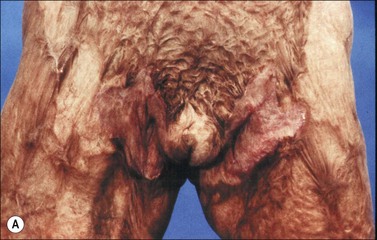
Loss of skin over the penile shaft and the scrotum
Spontaneous healing is expected in most instances with burn injuries of the penis and scrotum, since full thickness injury of the penile and scrotal skin is relatively uncommon. Skin grafting, a partial thickness or a full thickness graft could be used to cover the wound if healing is delayed (Fig. 58.2).
In rare instances, a skin flap may be needed to reconstruct structures such as urethral tract and/or scrotal sac because of loss of skin coverage. An inguinopudendal skin flap mobilized from the inguinal crease area may be used if the use of skin graft is judged not to be feasible.3 The use of muscle-skin flap such as a gracilis MC flap is not recommended because of subsequent high tissue temperature evolving in a skin flap that may interfere with spermatogenesis.
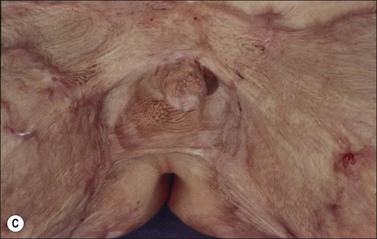
Burn wound of labia majora
Isolated burns of the labial structures are rare. Instead, labial burns are often associated with injuries of surrounding areas such as abdomen and inguinal folds. As in the management of burns of male genitalia, the injured areas are allowed to heal spontaneously (Fig. 58.3). Distortion of the labial structures mostly due to contraction of scar tissues in the pubic and inguinal areas is left for later reconstruction.
Perineal wound coverage
An isolated burn injury of the perineal area is extremely rare. On the other hand, the area will become involved if the lower trunk/buttock is injured. The extent of scar contracture varies depending upon the depth of burns. While it may heal spontaneously with minimal scarring, contracture of the perineal area is a common sequela, regardless of methods used to care for the wound (Fig. 58.4). The natural inclination to keep the thighs together and hip adducted during the recovery phase of acute burn injuries seems to aggravate scar contraction.
Rectal prolapse
Rectal prolapse occurs occasionally in young children with extensive burn injuries with or without perineal involvement. The exact reasons for rectal prolapse occurring in burned infants remain unclear. Redundant rectal mucosa, structural relationship of the rectum to other pelvic organs such as sacrum and coccyx, urinary bladder and uterus, and lack of muscular support provided by the pelvic musculature, anatomical features unique to infants of 1–3 years of age could account for the incident. Sudden increase in intra-abdominal pressure and malnutrition and constipation due to response to the burn injuries could conceivably aggravate the magnitude of the rectal mucosa descending through the anal opening.4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree