© Springer Nature Singapore Pte Ltd. 2018
Ichiro Katayama, Hiroyuki Murota and Takahiro Satoh (eds.)Evolution of Atopic Dermatitis in the 21st Centuryhttps://doi.org/10.1007/978-981-10-5541-6_2121. Management: Drug Therapy—Ointment
(1)
Department of Dermatology, National Defense Medical College, 3-2 Namiki, Tokorozawa 359-8513, Japan
Abstract
Atopic dermatitis (AD) is an allergic inflammatory skin disease etiologically associated with disrupted skin barrier function. Topical treatment is a fundamental approach for the management of AD. This includes various kinds of emollients/moisturizers as skin care and anti-inflammatory drugs, such as corticosteroids and tacrolimus. Improvement of barrier function could lead to reduced risk for the development and/or exacerbation of AD and reduces the chance for epicutaneous sensitization against environmental allergens, which may induce systemic allergy. Anti-inflammatory drugs are used for controlling flare-up of skin inflammation during the course of the disease. Proactive therapy, comprising continuous or periodical use and gradual tapering of anti-inflammatory drugs with emollients/moisturizers even when clinical symptoms improve, has been found to be useful for obtaining long-term remission. Patient adherence to external application is essential for reaching successful treatment outcomes with topical drugs.
Keywords
Barrier functionCorticosteroidsProactive therapyTacrolimus21.1 Introduction
Atopic dermatitis (AD) is a chronic eczematous skin disease. Patients are commonly complicated by repeated exacerbation and remission. Skin inflammation is closely associated with dry skin and barrier dysfunction. Topical therapies are the principal therapeutic approaches for AD. Basically, these consist of two components: emollients/moisturizers and topical anti-inflammatory drugs.
21.2 Emollients/Moisturizers
Rectification of dry skin and disrupted barrier function by emollients/moisturizers is a fundamental treatment for AD. Continuous use of moisturizers has been found to be effective for maintaining remission of AD [1]. In addition, a recent study conducted in Japan elegantly demonstrated that daily application of moisturizer to neonates prevented the development of AD [2].
The pharmaceutical effects of emollients/moisturizers appear to be determined by the composition of agents and constituents. Physicians should also consider the skin condition of the patient, weather (temperature and humidity), and patient preferences.
Olive oil and camellia oil are simple agents for increasing water content in the stratum corneum by inhibiting water evaporation through occlusion of skin surface. Petrolatum is also commonly used in emollients. A thick layer of petrolatum has been found to not only increase skin hydration but also improve transepidermal water loss (TEWL) [3]. Classical topical agents, such as hydrophilic ointment (cream) and zinc oxide ointment (10, 20%), are also useful.
Moisturizing agents actively keeping water include 10–20% urea cream and 0.3% heparinoid ointment/cream/lotion (Hirudoid®). A recent study demonstrated that topical urea application normalized skin barrier function and promoted antimicrobial peptide generation [4]. Many other types of moisturizers that include glycerin, hydrolyzed collagen, chondroitin sulfate, ceramides, free fatty acids, squalene, and/or cholesterol are available as clinically exclusive cosmetics, OCT (over-the-counter) products, or general cosmetics/products.
21.3 Topical Anti-inflammatory Drugs
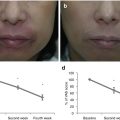
Topical corticosteroids and an immunosuppressant, tacrolimus, represent a highly recommended therapeutic option as a topical therapy for AD. Since repeated exacerbation of symptoms is common, topical anti-inflammatory drugs are generally used to obtain remission at the time of flare (reactive therapy). Recently, an alternative method, proactive therapy, has been recommended for patients with repeatedly relapsing eruptions [5, 6]. Anti-inflammatory drugs are used for obtaining remission of exacerbated lesions, followed by periodical application instead of cessation of topical drugs, even when skin inflammation is clinically improved; this could lead to the maintenance of long-term remission. Serum TRAC levels have been reported as a useful marker for determining the dose, application frequency, and/or time of cessation of anti-inflammatory drugs [5]. Concomitant use of emollients/moisturizers with anti-inflammatory drugs during proactive therapy is recommended. A randomized, investigator-blinded study demonstrated that proactive therapy, but not reactive therapy, with corticosteroids in children with AD prevented sensitization against aeroallergens in addition to decreased clinical severity and serum TARC levels [6]. Apparently, physicians should take care of adverse reactions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree