38
Mallet Fractures
Kevin D. Plancher
History and Clinical Presentation
A 45-year-old left hand dominant professional squash player was lunging for a shot and fell, landing on his hand. He had sudden pain in his long finger with the inability to extend the tip of his finger. The patient reported no other injuries. He has no history of arthritis.
Physical Examination
The patient is unable to extend the tip of his finger. There is swelling around the injury. The tip of the fingers is sitting at a 45-degree dropped position (Fig. 38–1). The finger has full vascular flow.
Diagnostic Studies
Anteroposterior (AP), splay lateral, and oblique radiographs of the injured digit were obtained. The joint was assessed for joint dislocation, subluxation, and fractures (Fig. 38–2).
Differential Diagnosis
Soft tissue mallet
Dislocated distal interphalangeal (DIP) joint
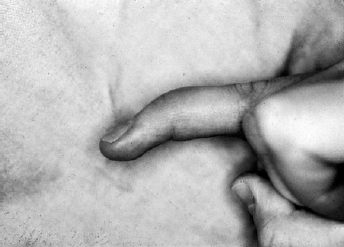
Figure 38–1. Attitude of a finger with the inability to extend the tip sitting at 45 degrees.

Figure 38–2. Radiograph, splay lateral, demonstrating a mallet of the ring finger of a different patient.
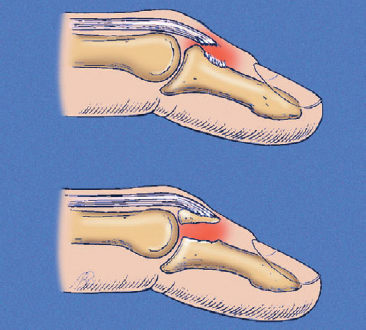
Figure 38–3. A type A mallet finger.
PEARLS
- Patient expectations of a straight finger upon healing is unrealistic. It is important to tell patient that half the “droop” will be a goal.
- Do not underestimate the cosmetic emotional effect of a mallet finger on individual personalities.
PITFALLS
- ORIF of a distal phalanx (P3) mallet is a technically demanding exercise. One drill hole is permitted with one pass only to avoid infection and damage to the articular surface.
- Nonoperative treatment may lead to a splint that is too tight. Dorsal skin ulceration and maceration.
Diagnosis
Mallet Fracture with Subluxation
Mallet finger injuries range from pure tendon rupture to tendon rupture with a fracture of the base of the distal phalanx. A type A mallet finger is a tendon rupture (Fig. 38–3), a type B is a chip fracture, a type C is an avulsion fracture without displacement, a type D is an avulsion fracture with displacement of the fragment (Fig. 38–4), and a type E has displacement of the avulsion fracture with subluxation of the distal phalanx. Type E fractures often require operative intervention. Forceful hyperflexion usually results in pure tendon ruptures or tendon ruptures with a small bone fracture.
In fractures involving articular surfaces, accurate anatomic reduction by surgery is usually required. For mallet fractures, satisfactory finger function may be regained despite mild arthrosis.
Nonoperative Management
Nonoperative management is indicated for mallet fractures when the distal articular surface is congruous with the condyles of the middle phalanx and volar subluxation is not present (Fig. 38–5). However, in patients seen with acute injuries involving more than one third to one half of the joint space with volar subluxation present, open reduction and internal fixation (ORIF) have obtained good results.
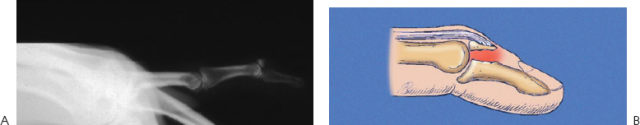
Figure 38–4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








