Approximately how many new melanomas are diagnosed each year and roughly how many patients die from melanoma annually?
There are approximately 75,000 new cases of melanoma diagnosed each year and between 9,000 and 10,000 patients die from melanoma annually.
 What are the ABCDEs of melanoma?
What are the ABCDEs of melanoma?
A: Asymmetry
B: Border irregularity
C: Color variegation or change
D: Diameter greater than 6 mm
E: Evolutionary changes in color, symmetry, size, shape, or symptoms
 What are some of the common known risk factors for the development of melanoma?
What are some of the common known risk factors for the development of melanoma?
Environmental:
1. Exposure to ultraviolet radiation (UVR)
2. History of sunburns, particularly in childhood or sunburns that induce severe pain/blistering
Personal:
1. Red hair
2. Skin type
3. Sun sensitivity
4. Family history
5. Number of moles present (risk increases as number of moles increases)
6. Personal history of melanoma
7. Female sex
8. Immunosuppression
9. Diagnosis of xeroderma pigmentosum
10. History of dysplastic nevi
11. Inherited genetic mutations (e.g., mutations in CDKN2A, CDK4, and TERT)
 What is the most common type of melanoma?
What is the most common type of melanoma?
Superficial Spreading Melanoma (SSM)
Accounting for approximately 60% to 70% of all melanomas, SSM is the most common type. SSM is most frequently diagnosed in the fifth, sixth, and seventh decades of life and is most commonly found on the legs of females and the trunk of males. Nodular melanoma accounts for approximately 15% to 30% of all melanomas and is the second most common type of cutaneous melanoma in light-skinned individuals. Lentigo maligna melanoma makes up approximately 10% of all melanomas and is found most commonly on the face. Nevoid and Spitzoid melanomas are uncommon variants of melanoma.
 What are the recommended surgical margins for melanoma in situ (MIS)?
What are the recommended surgical margins for melanoma in situ (MIS)?
NCCN guidelines for resection margins for MIS recommend a measured margin of 0.5 to 1 cm around the clinically visible lesion. They state that certain types of MIS, for example, lentigo maligna melanoma, may require resection margins beyond 5 mm. No definitive resection recommendations beyond the current recommendations of 5 mm have been given. Published recurrence rates for wide local excision (WLE) in the literature range from 8% to 20%. Despite this, WLE remains the gold standard treatment for MIS although a number of published stage excision protocols have shown recurrence rates ranging from 0% to 7.3%.
 What are the recommended surgical resection margins for a 2.1 mm thick primary cutaneous melanoma?
What are the recommended surgical resection margins for a 2.1 mm thick primary cutaneous melanoma?
2.0 cm.
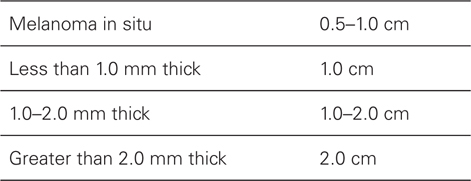
The current recommended margins for surgical resection of primary melanoma:
 What is the overall rate of local recurrence following surgical excision of melanoma with appropriate margins?
What is the overall rate of local recurrence following surgical excision of melanoma with appropriate margins?
The rate of local recurrence approaches 4%.
 What are the current recommended surgical resection margins for recurrent or in transit melanoma?
What are the current recommended surgical resection margins for recurrent or in transit melanoma?
True local scar recurrence, which most likely represents locally persistent disease after inadequate initial excision, is treated similarly to the primary tumor. Following confirmatory biopsy, re-excision to the appropriate margins based on Breslow thickness is recommended. In contrast, there are no definitive data to guide management at this time for local recurrences (defined as regrowth within 2 cm of the surgical scar after definitive excision) or disease in transit (any skin or subcutaneous metastases that are >2 cm from the primary lesion and distal to the regional nodal basin). These lesions (local recurrence and in transit disease) are thought to represent dermal lymphatic disease and impart a prognosis similar to regional nodal disease; whereas, there are no conclusive data that true local scar recurrence negatively affects outcome. National Cancer Comprehensive Network (NCCN) guidelines recommend complete surgical excision to clear margins if feasible.
 What are the indications for sentinel lymph node biopsy in melanoma patients?
What are the indications for sentinel lymph node biopsy in melanoma patients?
1. Patients with lesion thickness greater than 1.0 mm and no evidence of metastatic disease nor clinical lymph node involvement should be offered SLNB.
2. SLNB should be discussed and offered to patient’s with lesions that are 0.76 to 1.0 mm thick with either ulceration or mitotic rate ≥1 per mm2.
The 2015 NCCN guidelines state that in general, SLNB is not recommended for lesions 0.75 mm or less, regardless of other characteristics. It does state, however, that in the rare event that a high-risk feature is present (e.g., ulceration, high mitotic rate, and/or lymphovascular invasion), the decision to perform an SLNB should be left to the physician and patient.
3. Patient request. This is highly controversial due to the lack of definitive guidelines regarding the use of sentinel lymph node biopsy in melanoma. Patients must be aware of the complication rate of sentinel node biopsy (approximately 6%) in comparison to their chance of having a positive node (between 5% and 8% in patients with melanomas less than 1.0 mm thick).
 Assign the following primary melanoma lesions with the corresponding American Joint Committee on Cancer (AJCC) stage.
Assign the following primary melanoma lesions with the corresponding American Joint Committee on Cancer (AJCC) stage.
1. 0.76 mm thick lesion, with evidence of ulceration, no clinical LAD
2. 2.2 mm thick lesion, no evidence of ulceration, no clinical LAD
3. 2.9 mm thick lesion, no ulceration, one clinically enlarged lymph node, that is confirmed positive on lymphadenectomy
4. 3.1 mm thick lesion, no ulceration, positive SLNB, positive metastasis in the liver
5. 0.56 mm thick lesion, no evidence of ulceration, no clinical LAD
The current AJCC staging system is set up such that stages 1 and 2 represent local disease, stage 3 is regional metastasis, and stage 4 is distant metastasis. Please see the chart below for the complete staging system.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


