Maculae
DEFINITION
Lichen planus is an inflammatory disease of unknown cause that may involve skin and mucosal surfaces.
GENERAL FEATURES
It is uncommon to see a patient with lichen planus in a gynecologic practice. More frequently these patients present to dermatologists for evaluation of their papular skin lesions or to oral surgeons and dentists for evaluation of their desquamative and ulcerative buccal lesions.
CLINICAL PRESENTATION
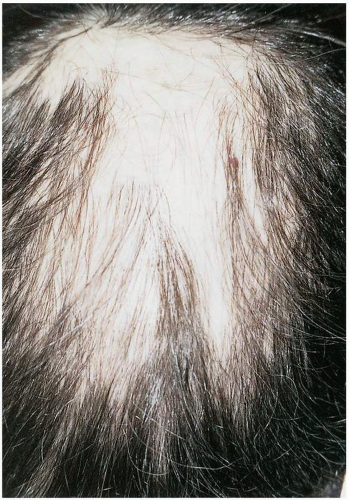
With involvement of the vagina the patient may complain of uncomfortable intercourse and a sensation that vaginal depth is diminishing. There may be a vaginal discharge, which may be tinged with blood. Questioning the patient who presents with these symptoms about skin or oral lesions may be informative. Physical examination may reveal the presence of oral lesions, which may be present without symptoms. Patients may complain of hair loss. There may also be a history of papular lesions on skin surfaces (ankles, dorsal surfaces of the hands, and flexor surfaces of the wrists and forearms). These may be pruritic.
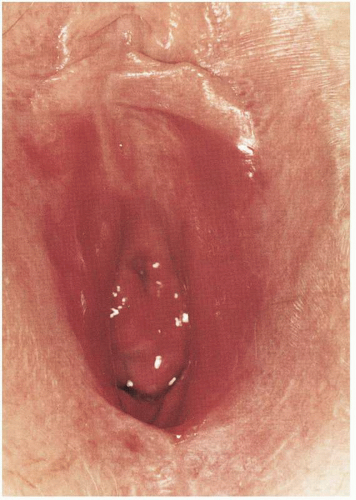
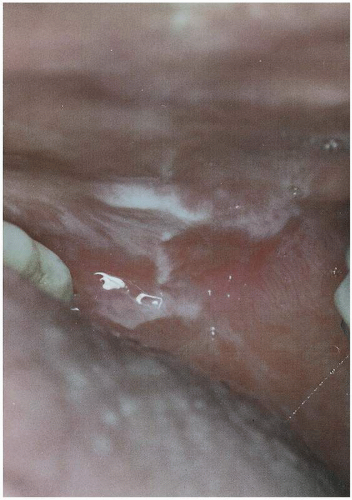
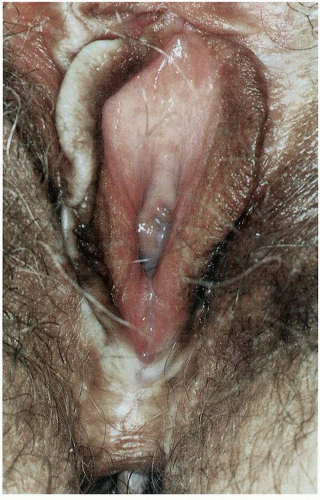
Although lichen planus is an uncommon disease, it should be considered in the differential diagnosis of desquamative vaginitis. It typically involves the vestibule and vagina. The vestibule may demonstrate a reticular pattern known as Wickham striae. The vagina may be markedly erythematous, and a serosanguineous discharge may be present. With progressive disease, the walls of the vagina may adhere to one another and the vaginal vault may be lost. As with lichen sclerosus, vulvar architecture may be obscured with fusion of the labia minora and labia majora, resulting in obliteration of the clitoris. It is feasible to misdiagnose lichen planus as lichen sclerosus. Patients with lichen sclerosus do not
have reticular patterns in the vestibule and do not have a desquamative vaginitis. To evaluate the patient completely, one must perform a careful general dermatologic review, including examination of the scalp and oral mucous membranes. The occurrence of the typical papular lesions on the skin and the reticular pattern in the mouth would further support a diagnosis of lichen planus. Ultimately, biopsy will be the most definitive method of arriving at the appropriate diagnosis. Biopsies are most productive when taken from intact skin or mucous membranes. Ulcerative lesions are difficult to assess histologically and will demonstrate inflammation. A biopsy from a reticulate lesion at the vestibule will be most helpful and is readily obtained.
have reticular patterns in the vestibule and do not have a desquamative vaginitis. To evaluate the patient completely, one must perform a careful general dermatologic review, including examination of the scalp and oral mucous membranes. The occurrence of the typical papular lesions on the skin and the reticular pattern in the mouth would further support a diagnosis of lichen planus. Ultimately, biopsy will be the most definitive method of arriving at the appropriate diagnosis. Biopsies are most productive when taken from intact skin or mucous membranes. Ulcerative lesions are difficult to assess histologically and will demonstrate inflammation. A biopsy from a reticulate lesion at the vestibule will be most helpful and is readily obtained.
MICROSCOPIC FINDINGS
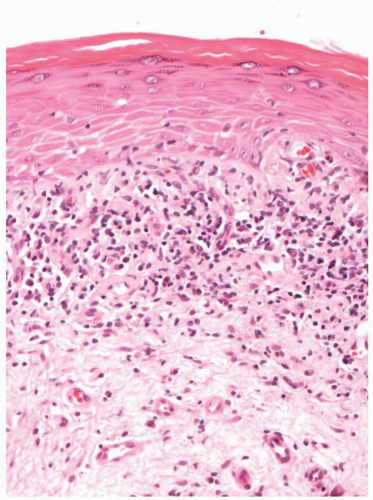
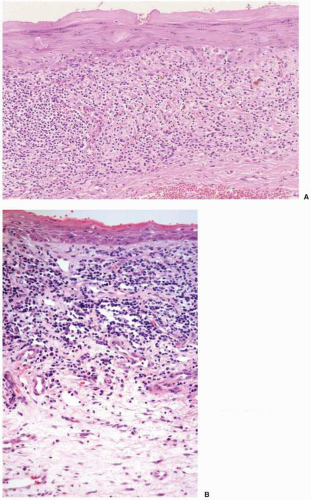
Lichen planus may have a variety of histopathologic features within the vulva, depending on whether or not the lichen planus involves hair-bearing, keratinized skin or non-hair-bearing, nonkeratinizing vulvar vestibule.
Within hair-bearing and keratinized epithelium, lichen planus is characterized by a lichenoid interface chronic inflammatory cell infiltrate, which consists predominantly of lymphocytes, without plasma cells. The inflammation is lichenoid in that it involves the superficial dermis, immediately beneath the epithelium, and extends into the basalar and parabasalar epithelium. The basal epithelial cells have liquefaction necrosis; colloid bodies are present secondary to degeneration of keratinocytes. The inflammatory infiltrate obscures the interference at the epidermaldermal junction. The epithelium may have prominent acanthosis, with a prominent granular layer and hyperkeratosis. In older lesions, acanthosis may be absent and the epithelium thinned, with loss of the
rete ridges. Ulceration and bullae may occur in severe lesions.
rete ridges. Ulceration and bullae may occur in severe lesions.
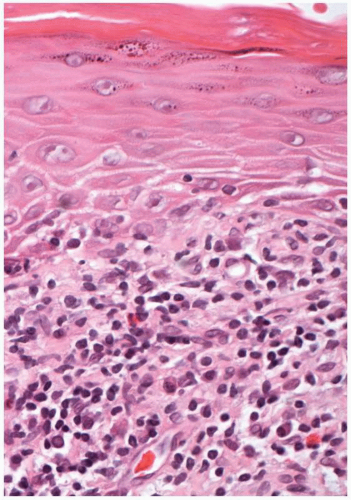
When lichen planus involves the nonkeratinized epithelium of the vestibule, the interface inflammatory infiltrate is present; however, the inflammatory cell population may contain plasma cells within the predominantly lymphocytic infiltrate. Thinning of the epithelium, with inflammatory cell exocytosis, is common. Hyperkeratosis and a prominent granular layer usually are not present. Colloid bodies with keratinocyte liquefaction necrosis, bullae, and ulceration are evident in severe cases. Silver and periodic acid-Schiff stains for bacteria, fungi, and spirochetes are negative.
ADJUNCTIVE STUDIES
Indirect and direct immunohistology may be necessary for confirmation of diagnosis if the possibility of pemphigus or pemphigoid exists. Pemphigus and pemphigoid (most commonly cicatricial pemphigoid) may result in desquamative changes in the vagina and should be included in the differential diagnosis of desquamative vaginitis. Interestingly, lichen planus and bullous pemphigoid may occur in the same patient.
CLINICAL BEHAVIORS
The management of patients with vulvovaginal lichen planus is difficult. The mainstay of therapy consists of topical application of low- to moderate-strength steroid preparations. These preparations are applied readily to the vulvar and vestibular regions, but intravaginal insertion poses a problem. Suppositories containing 25 mg of hydrocortisone may be inserted into the vagina once or twice daily for control of vaginal symptoms. However, most patients do not experience significant long-term response to the intravaginal steroids. The vaginal vault may continue to scar. To keep the vault patent and prevent adhesions it will be necessary, in selected cases, to use vaginal dilators. Vaginal maintenance may be accomplished with daily use of Lucite dilators. The dilator may be lubricated with a hydrocortisone cream. An alternative approach in patients who suboptimally respond to topical steroids is topical application of the T-cell inhibitor tacrolimus. Applied locally twice daily, the 0.1% ointment may afford significant relief; however, untoward symptoms such as burning and tingling may be observed. Also, after discontinuation of tacrolimus use the disease process has a tendency to recur. Tacrolimus is a T-cell inhibitor, and thus the potential exists for activating latent vulvovaginal infections such as condylomata acuminata or herpes simplex virus. Anecdotal reports concerning the successful use of oral griseofulvin, 250 mg twice a day, would warrant a trial of this rather innocuous medication. Immunosuppressant therapy with cyclosporine has been used to manage oral LP, either as a mouthwash or administered systemically. Vaginal douching with cyclosporine has been considered, but may result in unacceptably high serum concentrations resulting from vaginal absorption. Although success is noted with immunosuppressant therapy, recurrence of the disease is observed typically after discontinuation of immunosuppression. Dapsone, a pharmacologic agent used to treat leprosy, has on occasion demonstrated an ameliorative effect and may be considered, but only after performing a screen for glucose-6-phosphate dehydrogenase (G6PD) deficiency. Patients with G6PD deficiency may develop a profound anemia when exposed to dapsone. Patients treated with dapsone should be observed closely for evidence of anemia (weekly complete blood cell counts). Dosage is 50 to 100 mg daily.
PROGRESSIVE THERAPEUTIC OPTIONS
Progressive therapeutic options are as follows:
Topical steroids
Betamethasone 0.1% ointment to vulva twice daily. Clobetasol 0.05% ointment to vulva twice daily if higher potency steroid is indicated.
Hydrocortisone 25-mg suppository every day in vagina; augment with vaginal dilators to maintain vault patency. If low-potency suppositories are ineffective, try a short course of vaginal 0.1% betamethasone cream daily (2 weeks).
Topical 0.1% tacrolimus ointment twice daily to vulva. (Warn about painful burning and risk of HSV and HPV activation; avoid long-term use.)
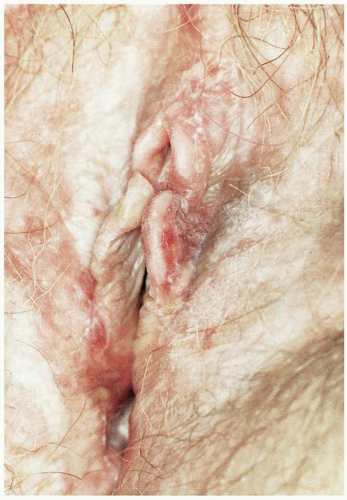 Figure 3.11. Excoriation due to scratching. Biopsy confirmed lichen sclerosus. Testosterone had been of no benefit; topical Valisone 0.1% ointment resolved the pruritus. |
 Figure 3.12. Clitoromegaly developing in a patient with lichen sclerosus after 18 months of topical testosterone. |
DEFINITION
Lichen sclerosus is a chronic dermatologic condition associated with epithelial thinning, distinctive dermal changes, and inflammation.
GENERAL FEATURES
The prevalence of lichen sclerosus is unknown; however, it is one of the most common conditions treated in vulvar clinics. Likewise, the etiology is unknown, although various mechanisms have been proposed, including immunologic, genetic, androgen receptor inactivity or deficiency, and epidermal growth factor deficiency.
CLINICAL PRESENTATION
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree