33
Lupus Erythematosus
General
• A multisystem AI-CTD disorder that prominently affects the skin.
• Broadly divided into systemic lupus erythematosus (SLE), cutaneous lupus erythematosus (CLE), and drug-induced lupus erythematosus (DI-LE) (Fig. 33.1).
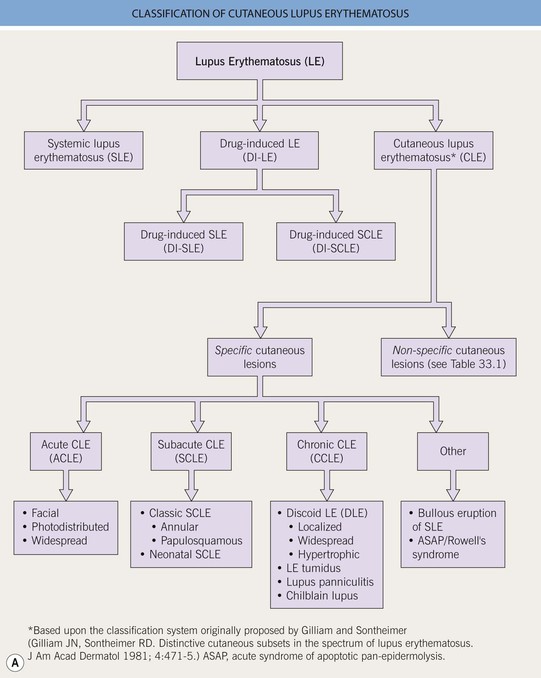
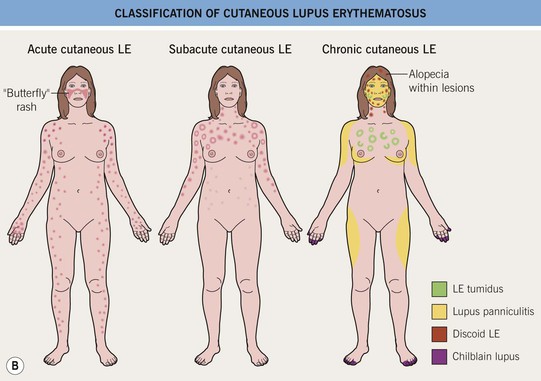
Fig. 33.1 Classification of cutaneous lupus erythematosus (LE). A Spectrum of LE. B Major forms of cutaneous LE.
• CLE is further classified into specific and nonspecific skin lesions, based on the histopathologic presence (specific) or absence (nonspecific, Table 33.1) of an ‘interface dermatitis’; however, this is not a perfect classification scheme because some specific entities (e.g. LE tumidus, lupus panniculitis) do not demonstrate an ‘interface dermatitis’ and other, non-lupus entities may display an ‘interface dermatitis’ on histopathology (e.g. dermatomyositis).
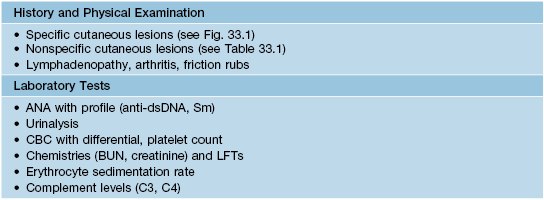
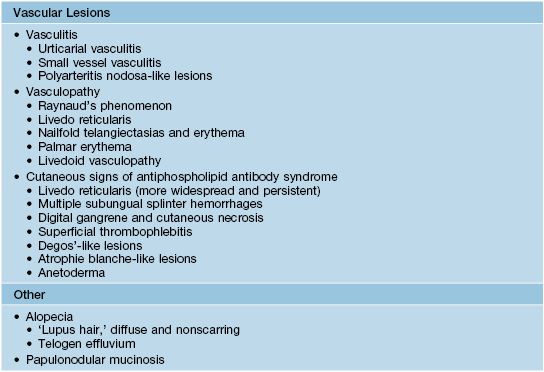
Table 33.1
Cutaneous findings (nonspecific) that suggest the diagnosis of systemic lupus erythematosus.
These cutaneous lesions are associated with LE but are not specific to LE itself. The presence of nonspecific LE skin lesions raises the possibility of SLE and may signify more significant internal disease. The presence of these nonspecific lesions should prompt an evaluation for SLE (see Tables 33.2 and 33.3).
• Classically, the three major forms of specific skin lesions are chronic cutaneous LE (CCLE), subacute cutaneous LE (SCLE), and acute cutaneous LE (ACLE), with CCLE being subdivided into four different entities (see Fig. 33.1).
• Once a diagnosis of CLE is made, initial and longitudinal evaluation for systemic manifestations of SLE is recommended (Tables 33.2–33.4).
Table 33.2
The American College of Rheumatology 1982 revised criteria for classification of systemic lupus erythematosus.*
Although these criteria are very helpful in distinguishing SLE from other rheumatologic conditions, they are not very helpful in distinguishing other skin diseases from LE. See Appendix for 2012 Systemic Lupus International Collaborating Clinics classification criteria for SLE.
| Criterion | Basic Definition |
| 1. Malar rash | Fixed erythema, flat or raised over malar eminences |
| 2. Discoid rash | Typical DLE lesions |
| 3. Photosensitivity | Skin rash due to an unusual reaction to sunlight |
| 4. Oral ulcers | Oral or nasal ulceration, observed by a physician |
| 5. Arthritis | Non-erosive, involving ≥2 peripheral joints |
| 6. Serositis | Pleuritis or pericarditis |
| 7. Renal disorder | Persistent proteinuria or cellular casts |
| 8. Neurologic disorder | Seizures or psychosis |
| 9. Hematologic disorder | Hemolytic anemia or leukopenia or thrombocytopenia |
| 10. Immunologic disorder | Anti-dsDNA or anti-Sm or antiphospholipid antibodies |
| 11. Antinuclear antibody | Abnormal ANA titer, in the absence of drug-induced SLE |
* The proposed classification is based on 11 criteria. For the purpose of identifying patients in clinical studies, a person shall be said to have SLE if any 4 or more of the 11 criteria are present, serially or simultaneously, during any interval of observation.
DLE, discoid lupus erythematosus.
Table 33.4
Different forms of cutaneous lupus and their associations with systemic lupus erythematosus (SLE).
| Type of Cutaneous Lupus | Association with SLE |
| • Acute cutaneous lupus erythematosus (ACLE) | ++++ |
| • Subacute cutaneous lupus erythematosus (SCLE) | ++ |
| • Chronic cutaneous lupus erythematosus (CCLE) | |
| • Discoid lupus erythematosus (DLE*) | |
| – Localized (head and neck) | + |
| – Widespread/disseminated | ++ |
| – Hypertrophic | + |
| • Lupus erythematosus tumidus (LET) | +/– |
| • Lupus panniculitis | + |
| • Chilblain lupus | ++ |
| • Other variants | |
| • Bullous eruption of SLE | ++++ |
| • Rowell’s syndrome | ++ to ++++ |
* Risk factors for the development of SLE include widespread DLE, arthralgias/arthritis, anemia, leukopenia, increased ESR, and higher ANA titers.
• Before making a definitive diagnosis of cutaneous lupus, it is necessary to exclude a drug-induced etiology (Table 33.5).
• Treatment options for the various subtypes of CLE are fairly similar (Table 33.6).
Table 33.6
Suggested therapies for cutaneous lupus erythematosus (CLE).
All patients should be counseled about daily sun protection, as both UVA and UVB can trigger flares of CLE and may even lead to exacerbations of systemic symptoms. Topical therapy is indicated in local disease and as an adjunct to systemic therapy in severe and widespread CLE. Systemic therapy is indicated when skin lesions are widespread, disfiguring, scarring, or refractory to topical agents, or when extracutaneous manifestations are present, e.g. arthritis.
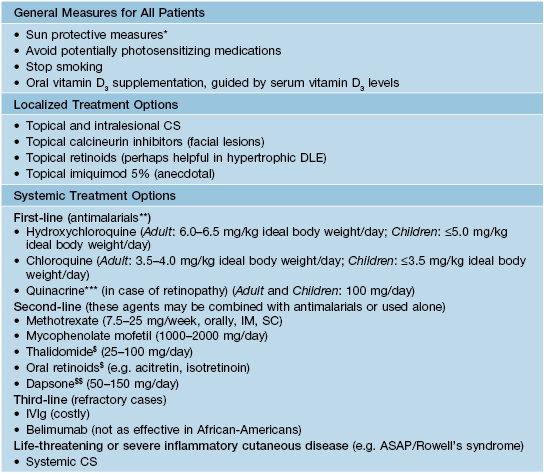
* Broad-spectrum sunscreen, sun avoidance, sun-protective clothing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree