Indications for lower extremity reconstruction in children are unique because most result from congenital conditions (eg, constriction ring, lymphedema, syndactyly, nevi, vascular anomalies). Like adults, pediatric patients also suffer from effects following extirpation and trauma. Principles of reconstruction are based on the condition and type of deformity. The pediatric population typically has fewer comorbidities than adults that can negatively affect outcomes (eg, diabetes, peripheral vascular disease), although children can be less compliant with postoperative care. Growth, development, appearance, and postoperative compliance are variables that especially influence operative management of children.
Key points
- •
Indications for pediatric lower extremity reconstruction often are related to congenital conditions.
- •
Principles generally follow adult lower limb reconstruction with special considerations for long-term functional and aesthetic outcomes.
- •
Immobilization of the extremity can help ensure protection of the limb postoperatively.
- •
Removal of large skin lesions before ambulation can reduce the risk of complications.
Introduction
The pediatric population is unique because many of the indications for lower extremity reconstruction are congenital conditions. The most common diseases managed by plastic surgeons are syndactyly, macrodactyly, constriction rings, lymphedema, congenital nevi, and vascular anomalies. Defects following extirpation and traumatic injuries are treated similarly to adults. Because of the pediatric age group, aesthetic outcomes are particularly emphasized by patients and families.
Indications and contraindications
Diagnosis of lower extremity disorders is made by history and physical examination. Indications for operative management are based on the type of congenital condition or defect.
Constriction Ring
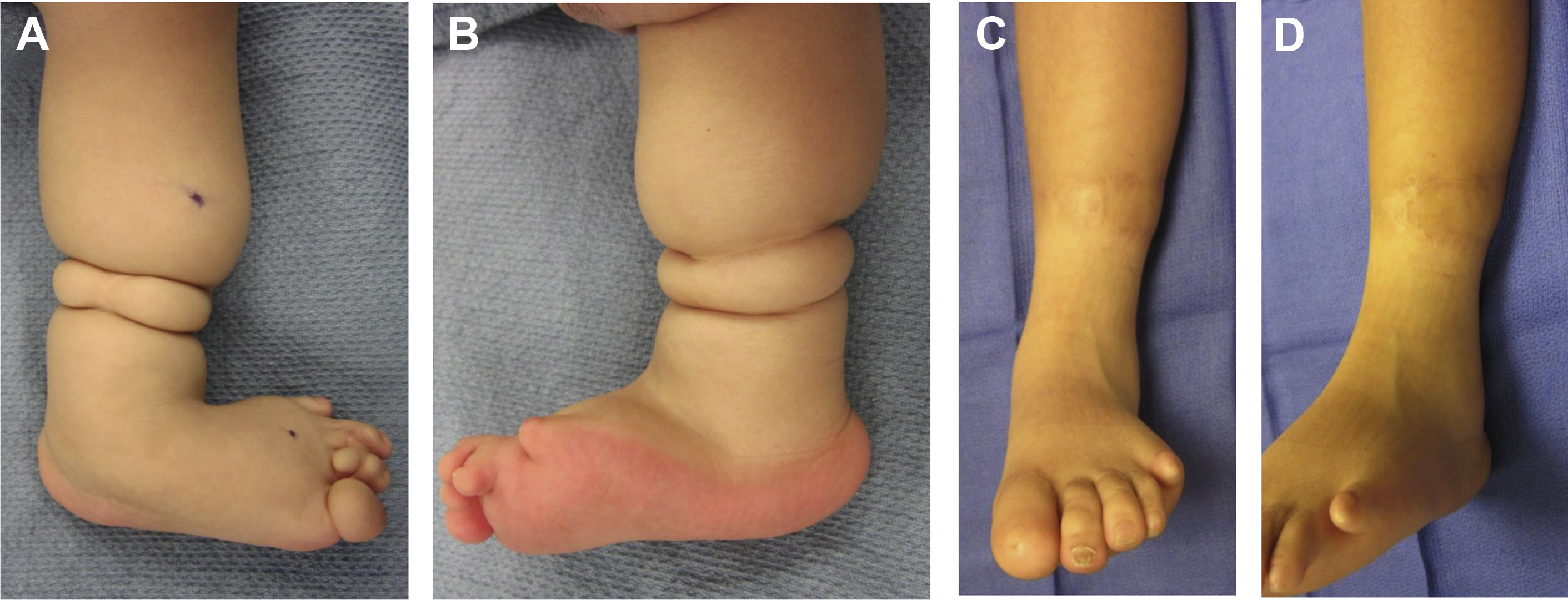
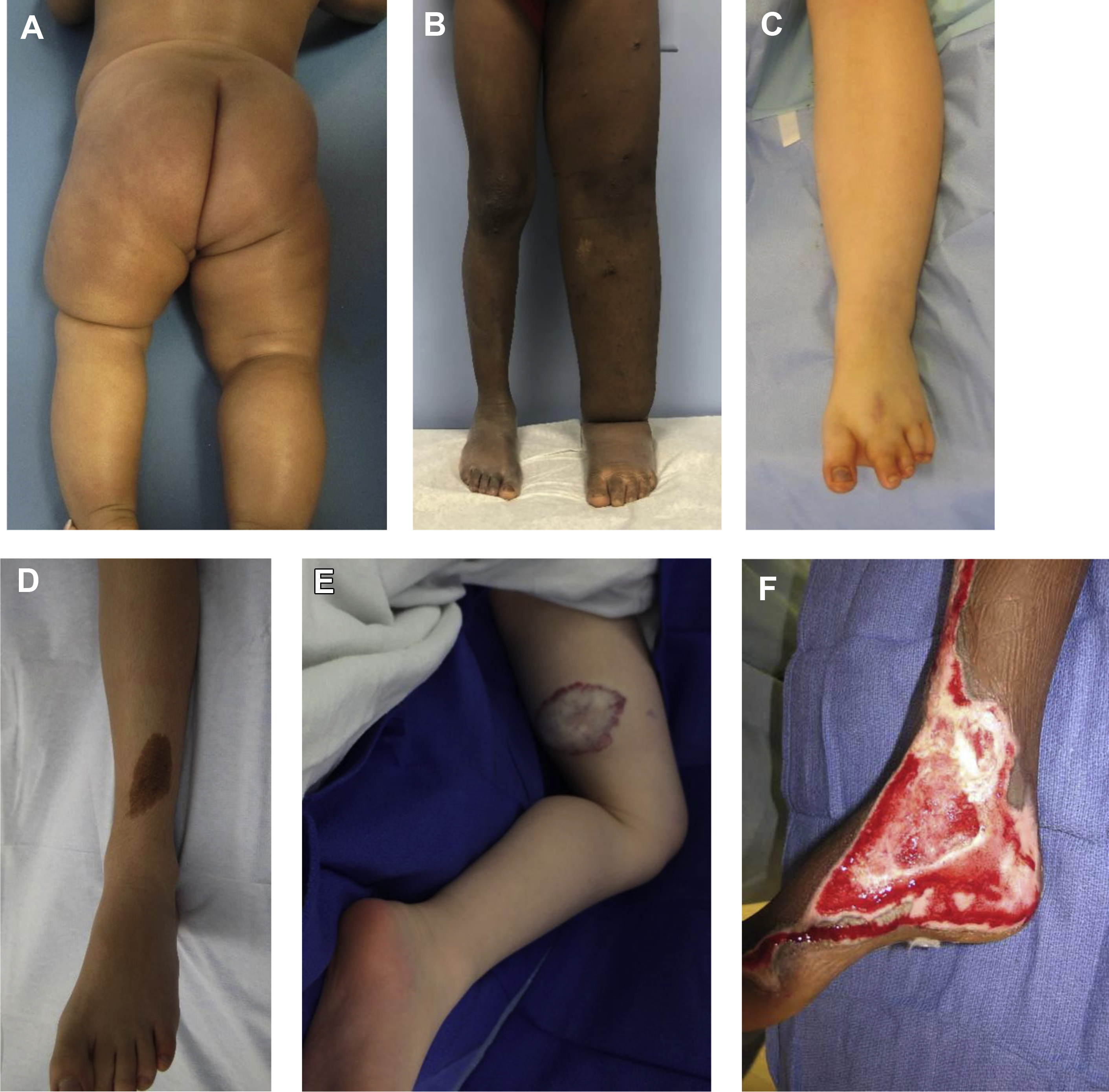
Constriction ring is most common in the toes but can affect any area of the leg ( Fig. 1 A). The spectrum ranges from superficial scarring to deep bands. Functional disability, growth disturbance, joint deformity, lymphedema, and congenital amputation can occur. Operative management is indicated to improve the appearance of a deformity as well as to correct any functional problems. Mild constriction rings not causing significant problems do not require intervention.
Lymphedema
Approximately 95% of patients with lymphedema do not require operative intervention and can be managed successfully with compression strategies (eg, stockings, pneumatic pump). Operative treatment is performed to improve the appearance of the limb if significant psychosocial morbidity is present, to reduce the number of infections, and to enhance the ability to ambulate and wear clothing ( Fig. 1 B).
Syndactyly
Syndactyly most commonly involves the second webspace ( Fig. 1 C). In Apert syndrome, syndactyly affects all 4 webspaces and bone coalition is rare distally. Syndactyly of the foot usually does not cause major functional problems. Most children are able to run and participate in sports. Treatment is usually requested by parents in early infancy or by patients during teenage years to improve the appearance.
Reconstruction Following Lesion Removal/Trauma
Giant nevi are at risk for developing melanoma and are excised if possible. Small, medium, and large nevi are removed if they appear atypical or are causing a significant deformity ( Fig. 1 D). Vascular anomalies typically are removed if they are symptomatic during infancy (eg, bleeding, infection, pain) or in childhood if they are causing a deformity ( Fig. 1 E). Defects resulting from lesion extirpation or trauma are managed similarly to adults ( Fig. 1 F). Usually adequate local tissue is available to cover bone or hardware proximal to the knee. Large areas of exposed bone or hardware involving the knee and mid-tibia may be covered using regional gastrocnemius or soleus flaps. Significant tissue loss involving the lower one-third of the leg can require free tissue transfer.
Preoperative evaluation and special considerations
Congenital anomalies do not require operative intervention unless they are causing a functional or “cosmetic” problem. The lower extremity is an unfavorable location to remove large lesions of the integument because skin redundancy is minimal and gravity favors swelling, which increases stress on the incision line. Placement of a cast or a removable knee brace after lesion excision should be considered to ensure better healing and avoid dehiscence. It is best to perform elective procedures after 6 months of age because the infant’s physiology approximates that of an adult, which reduces the risk of anesthesia. Because most infants begin ambulating at approximately 12 months of age, it is preferable to remove lesions before this time to reduce the risk of suture line dehiscence. If patients present after 12 months of age with lesions causing a deformity only (eg, infantile hemangioma, benign pigmented nevus), then removing the lesion before 4 years of age will eliminate the deformity before the child’s long-term memory and self-esteem begins to form. Some parents will prefer to wait until a child is old enough to participate in the decision to extirpate a lesion, which can occur in late childhood or early adolescence.
Constriction Ring
Operative treatment of a constriction ring should address the functional and aesthetic issues of the limb. Collaboration with an orthopedic surgeon is required in cases of joint involvement. For bands involving the legs or thighs, excision and flap advancement is performed. It is most favorable to treat before ambulation to take advantage of the extra soft tissue of an infant and easier immobilization.
Lymphedema
Patients are asked about risk factors for lymphedema (eg, family history, travel to areas endemic for filariasis, removal of or radiation to inguinal lymph nodes). Physical examination shows pitting edema and inability to pinch the dorsal skin of the foot (positive Stemmer sign). Definitive diagnosis of lymphedema is obtained with lymphoscintigraphy; the test is 96% sensitive and 100% specific for the disease. Individuals who are operative candidates (eg, repeated infections, large limb affecting activities of daily living) undergo MRI to determine if they have excess subcutaneous adipose hypertrophy that would benefit from suction-assisted lipectomy.
Syndactyly
Syndactyly most commonly affects the second webspace. Syndactyly usually does not result in lost function and patients are able to excel in physical activities. Operative intervention most often is performed to improve the deformity. Correction in infancy is advantageous before ambulation to reduce the risk of complications. Another common time to correct the syndactyly is during adolescence when patients become more self-conscious about their appearance. Before surgical correction, radiography is performed to determine if osseous fusion is present.
Reconstruction Following Lesion Removal/Trauma
Congenital nevi are evaluated by a dermatologist to determine if the lesion is concerning for malignancy. Patients with giant nevi larger than 2% total body surface area undergo MRI of the brain and spinal cord to rule out melanosis of the central nervous system. Most vascular malformations are evaluated by MRI to determine the extent of the lesion. Plain radiography is used to rule out fractures and foreign bodies following major traumatic injuries.
Almost all skin lesions can be removed by lenticular excision and linear closure; large areas may be managed by serial excision. Occasionally, large circumferential lesions require skin grafting or tissue expansion. Reconstruction of traumatic defects is based on the size, location, and depth of the wound. Superficial areas can be allowed to heal secondarily (with or without vacuum-assisted wound closure). Larger defects may be closed with delayed primary closure. Skin grafts are necessary if the wound cannot be closed linearly by advancing skin flaps. In the pediatric population, skin grafts should be avoided if possible because they cause a worse deformity than a linear scar and patients often will request that the graft be removed. Localized areas of exposed bone or tendon can be managed with vacuum-assisted wound closure to decrease the area of the wound and generate granulation tissue amenable to skin grafting. Large areas of exposed bone, tendon, or hardware in the lower leg require regional muscle flap closure or free tissue transfer.
Surgical procedures
Constriction Ring
We favor the technique described by Upton and Tan. Bands that are deep and narrow are favorable because they provide extra soft tissue to restore contour. The ring is marked and the skin is excised. Separate adipofascial and skin flaps are raised. The adipofascial flaps are mobilized and closed and then the skin flaps are approximated ideally away from the line of closure of the adipofascial flaps. Z-plasties are advocated extensively in the literature but are rarely needed. If the ring is deep or if there are multiple closely spaced rings, then a staged approach is considered ( Fig. 2 ).