35. Lower Blepharoplasty
Jason K. Potter, Ted H. Wojno
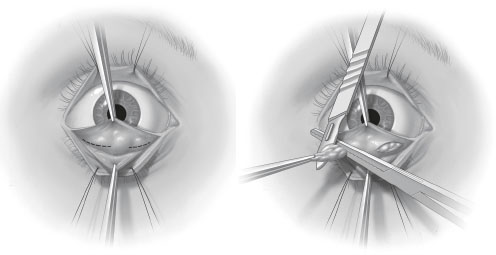
ANATOMY (Fig. 35-1)
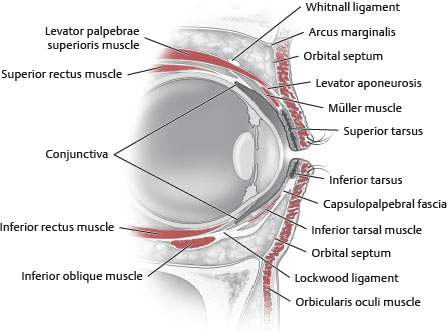
Fig. 35-1 Cross section of the upper and lower eyelids.
TERMINOLOGY
■ Dermatochalasis: Excess eyelid skin
■ Blepharochalasis: Thin, excessive eyelid skin secondary to recurrent bouts of painless lid edema
• 80% may have onset prior to age 20.
■ Blepharoptosis: Drooping or ptosis of the upper eyelid
■ Ectropion: An outward turning of the eyelid margin
• Senile: Results from age-related laxity of lower lid
• Cicatricial: Results from scar-induced retraction of lower lid
■ Entropion: Rolling of eyelid margin inward toward the sclera
• May result in irritation of the cornea or sclera by lashes
■ Retraction: A downward displacement of the lid margin resulting in inferior scleral show
■ Steatoblepharon: Excess or protruding fat through a lax septum
AESTHETIC EVALUATION OF THE LOWER LID1,2
■ Lid position: Lower lid should rest at level of limbus without scleral show between the limbus and lid margin.
■ Pretarsal bulge: Pretarsal orbicularis oculi hypertrophy considered by many to be aesthetic component of the youthful lower lid.
• Often present in attractive eyes
• Results from pretarsal orbicularis muscle fullness
■ Lid-cheek junction: Smooth, convex, essentially imperceptible transition from lid to cheek in youthful patients (Fig. 35-2)
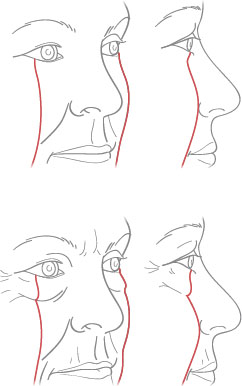
Fig. 35-2 Comparison of lid-cheek junction appearance in youth versus aged.
• Stigmata of aging include:
► Excess skin, pseudoherniation of intraorbital fat, malar pad descent, nasojugal groove, visible inferior orbital rim
► Hollowed appearance from paucity of intraorbital fat
CHARACTERISTICS OF THE AGING LOWER LID (Fig. 35-3)
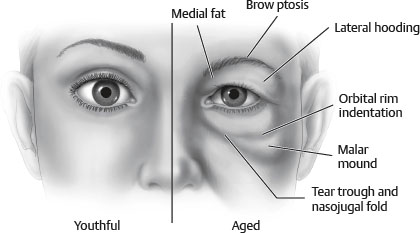
Fig. 35-3 Characteristics of aging periorbital region.
■ Skin quality
• Redundant with excessively thin and crêpey qualities
• Rhytids, fine and deep (crow’s-feet)
• Residual lines or wrinkles inevitable postoperatively
■ Skin pigmentation (blepharomelasma)
• Hyperpigmentation of the skin
■ Orbit vector: Position of globe relative to the inferior orbital rim
• Useful for predicting postoperative tendencies of lid position
• Negative vector orbits have poor lower lid suspension and are at risk for postoperative ectropion and retraction.
■ Lid laxity: Horizontal lid laxity has significant risk for postoperative lid malposition.
• Snap-back test: is delayed return of the lid margin to native position when retracted downward with finger traction.
• Pull-away test: is abnormal when the examiner grasps the lid margin between the index finger and thumb and pulls it away from the globe more than 10 mm.
• Best corrected with supplemental canthal anchoring procedures (see Chapter 38)
■ Redundant, ptotic orbicularis oculi muscle (festoon)
• Squint (or squinch) test: Forced closure of eyelids improves festoon if secondary to ptotic orbicularis oculi muscle
• Malar bag: Shelving of orbicularis oculi muscle over orbital retaining ligament with excess intraorbital fat
► Correction involves improving lid-cheek junction (Loeb procedure, septal reset, midface lift).
■ Bulging orbital fat: Weakening of the orbital septum may result in herniation of orbital fat pads creating visible deformity of the lower lid.
• This may be corrected by fat removal, repair of septum without fat removal, and fat relocation.
• Current techniques emphasize fat preservation.
■ Tear trough (see Chapter 29)
• According to Barton et al,3 created by herniation of orbital fat, tight attachment of the orbicularis along the arcus marginalis, and malar retrusion
• According to Codner et al,4 created by herniation of fat over the orbitomalar ligament, which arises from periosteum and attaches to skin
► According to this definition, the tear trough arises over a triangular space defined by the orbitomalar ligament, levator labii superioris, and levator alaeque nasi.
NOTE: The terms orbitomalar ligament, orbital retaining ligment, orbicularis retaining ligament refer to the same anatomic structure.
• Pronounced tear trough deformity may not be corrected with traditional blepharoplasty techniques alone.
■ Visible palpebromalar and nasojugal grooves
■ Lacrimal function: All patients should be questioned about dry eye symptoms.
• Blepharoplasty may contribute to or worsen dry eye symptoms in susceptible patients.
• Ophthalmologic consultation may be warranted.
■ Scleral show
• Lower lid should be at or within 2 mm of inferior limbus.
• Tarsal laxity, negative vector orbit, exophthalmos, or middle lamellar contracture of lower lid can be present.
SURGICAL TECHNIQUES
NOTE: Numerous lower lid blepharoplasty techniques have been reported. The following lists include the most commonly performed techniques.
SKIN RESURFACING
Patients with isolated fine lines may be treated with skin resurfacing techniques alone such as chemical peel or laser resurfacing (see Chapters 16 through 18).
SKIN-ONLY BLEPHAROPLASTY (PINCH BLEPHAROPLASTY)
■ Indications
• Patients with minimal redundant skin or fullness, usually isolated to the pretarsal region, and not associated with more significant age-related periorbital changes such as fat herniation, lid laxity or orbicularis ptosis
■ Technique5
• Forceps are used to gently pinch the redundant skin over the pretarsal orbicularis oculi to determine the width of skin to be resected.
• Appropriate width of skin to be resected is that which does not induce changes in the position of the lower lid.
• Skin to be excised is marked with a fine-tipped marker.
• Incision is performed with a No. 15 blade and excision of skin-only is performed with cautery.
• No undermining or elevation of a skin flap
NOTE: If pretarsal orbicularis hypertrophy is present and contributing to excessive fullness, a strip of pretarsal muscle may be excised as well.
NOTE: The pinch technique for skin excision may be combined with other blepharoplasty maneuvers such as transconjunctival fat removal in appropriate patients.