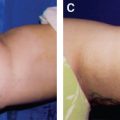
CHAPTER 13 Today liposuction has become one of the most frequently performed plastic surgery procedures in the world. According to the annual survey of the American Society for Aesthetic Plastic Surgery (ASAPS) in 2015, there were 342,494 liposuction operations performed in United States, and many more operations were performed by non-board-certified plastic surgeons. Liposuction procedures are ranked as the #1 procedure in plastic surgery, followed by breast augmentation. Buttock augmentation procedures were up by 92% in 2015. Liposuction requires thoughtful planning and an artistic eye to achieve an aesthetically pleasing postoperative result. Careful selection of patients, proper surgical technique, and diligent perioperative patient care help to prevent contour irregularities. The patient’s expectations should be based on realistic preoperative evaluation of the individual’s age, skin elasticity, the volume of fat to be removed, and the area of liposuction. True body sculpting demands a three-dimensional artistic understanding of the anatomic and surgical adipose layers of the central trunk. This is essential to prevent sequelae from suction-assisted lipoplasty. The best results are obtained by treating moderate localized fat deposits in a normal-weight patient whose body contour has not been successfully managed by diet and exercise. Physicians practicing liposuction surgery should have adequate training and experience in the field. In this chapter we will share our experience with liposuction, its pitfalls, the goals to be achieved, and methods for performing the procedure safely. To determine the appropriate surgical plan for a patient requesting body contouring surgery, the surgeon must carefully consider the anatomic characteristics of the area to be treated. Fat is deposited in the subcutaneous layer in almost all areas of the body. Fat cells may not be distributed evenly, causing some areas to be more prominent than is ideal. Patterns of fat distribution differ among races, ages, and sexes. The actual number of fat cells remains stable during adult life. The cells get larger with weight gain and smaller with weight loss. In general, women have a proportionately higher percentage of body fat than men. Women typically have a disproportionate number of fat cells in their hips and upper thighs, whereas men tend to have a more even distribution of fat cells in the trunk. A progressive accumulation of fat occurs intraabdominally as a person ages. This intraabdominal fat is not treated by liposuction, and thus must be differentiated carefully from subcutaneous fat when evaluating a patient for surgery. The principal anatomy of the abdominal wall comprises multiple layers: skin, subcutaneous tissue including fatty layer and Scarpa fascia, muscles and investing deep fascia, transversalis fascia, and peritoneum from exterior to interior. The primary target of liposuction is the subcutaneous layer in which the cannula is inserted. There is fat tissue in the subcutaneous layer of the abdominal wall, along with perforating arteries, veins, lymphatics, and nerve branches. Small branching vessels originate from the thoracic, lumbar, intercostal, external and internal iliac, common femoral, and superior or inferior epigastric vessels. The superficial vascular structures in the subcutaneous tissues supply the tissues superficial to the external oblique aponeurosis and anterior rectus sheath. The deep vascular structures in the musculofascial layers supply the muscles and tissues below these layers. The term lateral thigh aggregate describes a combined area of subcutaneous fat that consists of the lateral trochanteric area, the inferolateral buttock, and the bananaform fold of the proximal posterior thigh. Immediately below the subcutaneous fat pad of the lateral thigh is the tensor fascia lata and, more posteriorly, the muscles of the buttock and thigh. The sciatic nerve, located approximately 2 cm deep to the surface of the gluteus muscle, is outside the surgical field, even during liposuction of the inferolateral buttock or the posterior thigh. Understanding where and why more volume is required to recreate gluteal projection comes from familiarity with the anatomy of the gluteal and hip region. The superficial gluteal fascial apron and the deep gluteal fascia fuse, become tightly adherent, and form the infragluteal fold, which is an important feature of an aesthetically pleasing gluteal area. Liposuction in the infragluteal fold area for correction of a “banana roll” (a pocket of fat beneath the buttock crease) must be avoided. The deep gluteal fascia is important as a fixation point in many types of gluteal procedures and serves as a strong retaining fascia in the subfascial augmentation with implants. Several perforators from the superior and inferior gluteal arteries supply the gluteal area. Before it enters the gluteus maximus muscle to supply perforators to the superior portion of this muscle and overlying skin, the superior gluteal artery passes superior to the piriformis muscle. The inferior gluteal artery passes inferior to the piriformis muscle and supplies the lower half of the gluteus maximus muscle and overlying structures. All perforators from the inferior gluteal artery pass through the gluteus maximus, as do half the perforators from the superior gluteal artery; the other half pass through the gluteus medius muscle. Sensation to the gluteal region and lateral trunk comes from several sources: the dorsal rami of S3 and S4, the cutaneous branches of the iliohypogastric nerve arising from the L1 root, and the superior cluneal nerves that originate from the L1, L2, and L3 roots and then pass over the iliac crest. Anatomic Danger Zones ■ Patients who have significant intraabdominal fat may have a widened, squared appearance if only abdominoplasty is performed. The same procedure in a patient without significant intraabdominal fat can better define the waist and improve the gluteal contour. ■ Gluteal aesthetics can be greatly enhanced by judicious liposuction of the abdomen; the anterior, medial, and lateral thigh; the flanks; and the lumbosacral region. ■ Overaggressive liposuction of the breasts, buttocks, infragluteal fold, and hips often produces suboptimal aesthetic results and could lead to the necessity of secondary interventions for repair. ■ Poorly placed incisions in the area to be liposuctioned can detract from the regional aesthetics. ■ Familiarity with the target area is crucial; for example, liposuction in the chest for breast reduction may accidentally cause perforation of the chest wall and lead to pneumothorax. ■ In the abdominal area, liposuction when performed by a poorly trained surgeon or other operator may accidentally lead to perforation of abdominal hollow organs. ■ Increased compartment pressures with diminished perfusion to the area to perform autologous fat grafting can be caused by large-volume fat grafting within these compartments. ■ Damage to the vessels with bleeding and hematoma formation, or mass effect from large-volume fat grafting, can theoretically increase compartment pressures beyond a safe limit. Although still disputed in the literature, a compartment pressure higher than 30 mm Hg may cause necrosis of muscle in as little as 4 to 6 hours and Wallerian nerve degeneration in 8 hours. Although small-volume liposuction may not be associated with major hemodynamic changes, large-volume liposuction (defined as removal of more than 4 L of fat and fluid) does result in alteration of hemodynamics. An increase in cardiac index, heart rate, mean pulmonary arterial pressure, stroke volume index, and right ventricular stroke work index, along with a decrease in mean arterial pressure and systemic vascular index, has been observed during large-volume liposuction. There is also an increased risk of hypothermia in patients undergoing large-volume liposuction. Exposure of large body surface areas, infusion of large volumes of cold wetting solutions, the long duration of the procedure, general anesthesia, heat loss during mechanical ventilation, ambient room temperature, and intravenous fluids all contribute to hypothermia in these patients. Complications such as cardiac dysrhythmias, coagulopathies, oliguria, and electrolyte imbalance are worsened by hypothermia. Both the hemodynamic and thermoregulatory changes may persist for more than 24 hours after the beginning of surgery. The recommended volume of fat removed is in proportion to the patient’s weight; it generally should not exceed 4500 cc in a single operative session. Liposuction is not a means to produce weight loss but rather is intended to improve contours. Patients at or near their ideal body weight with localized areas of adipose tissue are much better candidates than obese individuals. Candidates should be carefully evaluated for their expectations and the actual results that can be achieved through liposuction. Adhering to appropriate indications and carefully planning the procedure are just as important as the surgical procedure itself. Patients who clearly have a psychiatric disorder, such as body dysmorphic disorder, should be referred for psychiatric evaluation. However, there are subtle cases in which patients present with low self-esteem, a borderline type of anxiety, and unrealistic expectations. In those cases, sometimes it is better to decline to operate on the patient. The ideal patient for liposuction has a small amount of adipose tissue to be suctioned to improve his or her body contour, has no skin laxity, and is dedicated to a healthy lifestyle, including daily physical exercise and a healthy diet. A good liposuction candidate should have a BMI between 25 and 29.9. It is the responsibility of the surgeon to discuss all of the concerns, risks, goals, and expectations of the procedure with the patient and ensure that the patient understands and accepts these factors to avoid false expectations and future frustration. Preoperative patient evaluation includes a thorough history and physical examination. Patients should be in either American Society of Anesthesiologists (ASA) class I or class II. Patients with uncontrolled medical problems are not candidates for liposuction of the trunk and thighs. Liposuction is contraindicated in patients with severe cardiovascular disease, in patients with severe coagulation disorders including thrombophilia, and during pregnancy. A thorough medical history is obtained, with special attention to any history of bleeding diathesis, emboli, thrombophlebitis, infectious diseases, poor wound healing, and diabetes mellitus. Patients with a medical history of these conditions need to receive medical clearance before undergoing liposuction. The history also includes prior abdominal surgery, prior liposuction, and problems from past surgical procedures. The safety of the liposuction technique depends not only on the amount of tissue removed but also on the patient’s overall health. It is ideal for the patient to be as fit as possible before the procedure and not to have smoked for several months. If any concerns exist regarding the health of the patient, the patient should be referred to the anesthesiologist or the patient’s primary care physician for evaluation. The use of all medications, vitamins, and herbs is documented, with particular attention given to medications that affect blood clotting, such as aspirin, NSAIDs, vitamin E, and anticoagulants. Drugs that may interact with lidocaine, epinephrine, or sedative and anesthetic agents must be noted. Candidates for liposuction should be in a healthy state both physically and mentally. Weight should be stable or decreasing with diet and exercise. Patients who are experiencing rapid or persistent weight gain should be started on a program of exercise and nutritional modification before being accepted as surgical candidates. Preoperative laboratory studies include a complete blood cell count, prothrombin and activated partial thromboplastin times, a blood chemistry profile, liver function tests, a pregnancy test for women of child-bearing age, and an ECG. An ultrasound scan of the chest is helpful to determine the relative proportion of breast tissue and fat in gynecomastia, or in the upper and lower abdomen excluding pathology when abdominal liposuction is indicated. Patients must have reasonable goals and expectations. Perfectionistic patients are rarely happy with the surgical outcome, and the surgeon should decline performing liposuction in such individuals. One should not offer elective aesthetic surgery to patients with body dysmorphic disorder or eating disorders. If the patient has reasonable expectations that agree with technically achievable results, he or she will tend to be very happy with the outcome. The key is to address preexisting skin contour irregularities, asymmetries, skin laxities, and redundancies to help the patient understand what kind of result can be obtained. In these cases, the possibility of secondary procedures and touchup procedures should also be emphasized. Thorough clinical examination should include a detailed evaluation of the regions to be contoured, including notations of hernias, scars, asymmetries, cellulite, and stretch marks. The quality of the skin, particularly its elasticity, and the presence of striae and dimpling should be noted. The underlying abdominal musculofascial system is evaluated for the presence of flaccidity, integrity, and diastasis recti. The areas of fat deposits are documented. The patient should sign a detailed consent form listing details about the procedure and possible complications. The consent form should specifically state the limitations of the procedure and whether more procedures will be needed to achieve optimal results. The patient is provided with adequate opportunity to seek information through brochures, computer presentations, and personal discussions. The patient is examined standing, sitting, and lying down, and careful palpation is performed. Evaluation of the area to be liposuctioned allows the surgeon to decide whether any associated surgical procedures are needed to achieve a better cosmetic result. Standardized photo documentation is required. The surgeon must pinch, feel, inspect, move, and contour the subcutaneous tissue in a manner that will produce an improved skin contour. It is imperative to keep the patient’s unique physical characteristics and skin type in mind when planning the procedure. Skin that has poor elasticity will not recontour. The surgeon will factor in all of these issues to determine just how much fat to remove, and from which areas, to produce an acceptable final result. Preoperative sedation in the surgical suite is administered. Anesthesia consists of an epidural block and intravenous sedation. With the patient standing, contour lines are drawn about the fat to be extracted and the areas that require fat grafting. The areas to be aggressively treated are clearly marked, as are areas not to be treated, and areas to be “feathered,” or lightly treated. Different-colored marking pens or one color with different types of marks are used, as long as it is clear to the surgeon. The patient is placed in the prone position, and when the liposuction and fat grafting have been performed in these areas, the patient is transferred to the supine position. Intraoperative intravenous cefazolin is administered before liposuction and fat grafting.
Liposuction of the Trunk and Thighs
Surgical Anatomy
Physiologic Considerations
Indications and Contraindications
Patient Evaluation
CLINICAL EVALUATION OF THE DEFORMITY
Preoperative Planning and Preparation
Surgical Technique
ANESTHESIA
MARKINGS
PATIENT POSITIONING
TECHNIQUE
Plastic Surgery Key
Fastest Plastic Surgery & Dermatology Insight Engine

 Beatriz Nicaretta Aris Sterodimas
Beatriz Nicaretta Aris Sterodimas