57. Liposuction
Cedric L. Hunter, Rohit K. Khosla, Jeffrey R. Claiborne, Simeon H. Wall, Jr.
■ First recorded attempt at lipectomy is attributed to the French surgeon Dujarier, who, in the 1920s, attempted to remove fat from a dancer’s calves using a uterine curette.1
• Vascular damage resulted in amputation of the leg.
■ In the mid-1970s Giorgio Fischer and his father, Arpad Fischer, developed the “cellusuctiotome,” an instrument made of a hollow curette and blade attached to a suction pump. This method had a high rate of bleeding complications.
■ Yves-Gerard Illouz and Pierre Fournier improved on the prior techniques by replacing the sharp curettes of the 1970s with a cannula and suction system, the introduction of a “wetting solution” containing saline solution and hyaluronidase, and the use of a “crisscross” technique.
• These methods decreased bleeding and contour-associated complications.
■ In the 1980s a dermatologist, Jeffrey Klein, introduced the tumescent technique.
• Tumescent technique: Subcutaneous infiltration of a large volume of diluted lidocaine and epinephrine that expands the fat compartment causing it to become swollen and firm, or tumescent
• Provides local anesthesia and reduces blood loss
ANATOMY
SUBCUTANEOUS LAYERS (Fig. 57-1)
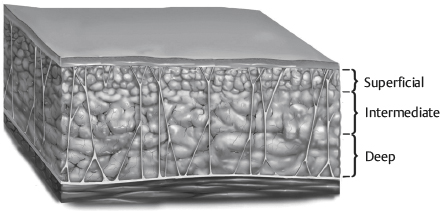
Fig. 57-1 Differences in subcutaneous tissues in various areas of the body.
■ Subcutaneous adipose tissue is divided into superficial and deep layers throughout the body by Scarpa fascia or the superficial fascial equivalent.2
■ For purposes of body contouring, the subcutaneous fat is arbitrarily divided into three layers.3
• Superficial
► Dense fat, adherent to overlying skin
► Aggressive, avulsive, or thermal liposuction methods should be used with great caution in this layer to prevent contour irregularities and skin damage.
• Intermediate
► Safest layer
► Most commonly suctioned layer
• Deep
► Loose and less compact layer
► Can be removed safely in most areas
ZONES OF ADHERENCE (Fig. 57-2)
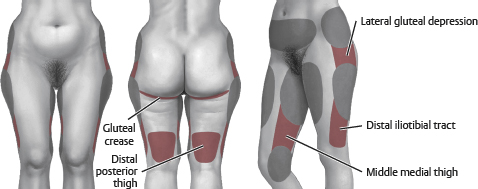
Fig. 57-2 Zones of adherence.
■ Distal iliotibial tract
■ Gluteal crease
■ Lateral gluteal depression
■ Middle medial thigh
■ Distal posterior thigh
CAUTION: Be very cautious removing fat from zones of adherence. The stiff fibrous network predisposes these areas to postoperative contour deformities.
SENIOR AUTHOR TIP: The rigid fibrous connections at zones of adherence can be relaxed using an exploded tip cannula without suction (i.e., separation and equalization). The tissue will become more pliable to allow smooth transitions into surrounding areas and enable these zones to be traversed or treated safely.
CELLULITE (GYNOID LIPODYSTROPHY)
■ Peau d’orange and mattresslike deformity seen primarily in women and obese patients
■ Two types4
• Primary or cellulite of adiposity: Results from hypertrophic fat cells in the superficial fat between the septa of the superficial fascial system
► Typically present when supine and erect, seen in younger women
► Generally not improved with skin-tightening procedures
• Secondary or cellulite of laxity: Results from increased skin and superficial fascial system laxity
► Present when erect but not supine, usually >35 years of age
► Treated with skin- and superficial fascial system-tightening procedures
PREOPERATIVE EVALUATION
PHYSICAL EXAMINATION
■ Check for deviation from ideal contour (Fig. 57-3).
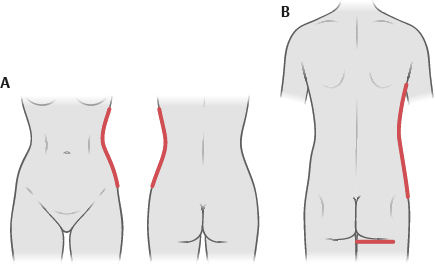
Fig. 57-3 Ideal contour. A, Female. B, Male.
• Female ideal contour
► Concavity below the rib cage that changes to a convexity over the hips and thighs
► Medial and lateral thighs have mild convexities.
► The buttock crease blends laterally with thigh.
• Male ideal contour
► More linear silhouette, less concavity and convexity below rib cage and over thighs
► The buttock crease is squared and linear.
► Flat anterior infraumbilical region
• Note any of the following:
► Asymmetries
► Dimpling/cellulite
► Location of fat deposits
► Areas of adherence
► Hernias and myofascial diastasis
• Check skin laxity.
• Examine spine for scoliosis.
► May cause asymmetry
• Assess for hernias/diastasis.
MEDICAL HISTORY
■ Agents that interfere with coagulation should be avoided.
• Aspirin
• NSAIDs
• St. John’s wort
• Vitamin E
• Herbal supplements
• Other anticoagulants
■ Note personal and family history of deep venous thrombosis or clotting disorders.
■ Photographs
• Standard photographs of areas to be treated should be obtained.
• See Chapter 3 for further details on photography.
SENIOR AUTHOR TIP: Patient selection is critical. Common pitfalls include: redundant and poor quality skin, obesity with excess intraabdominal fat and unreasonable expectations.
PERIOPERATIVE CONSIDERATIONS
PREOPERATIVE
■ Complete blood cell count if expecting to perform large-volume (>5 L total lipoaspirate) procedure
■ Perioperative IV antibiotics
■ Deep venous thrombosis prophylaxis
• Intermittent pneumatic compression devices should be used intraoperatively.
• Chemoprophylaxis may be given to those at higher risk (see Chapter 11).
HYPOTHERMIA
■ Forced-air warming blankets
■ Consider circulating warm water mattresses
■ Cover exposed body areas.
■ Warm intravenous fluids.
■ Warm operating room.
■ Warm wetting solutions.
POSITIONING
■ Pad all pressure points.
■ Prone position
• Protect face, breasts, and genitals.
• Soft hip roll beneath iliac crest
■ Supine position
• Arm abduction <90 degrees to prevent brachial plexus injury
• Hips and knees flexed at 30 degrees with a pillow
SENIOR AUTHOR TIP: Using multiple patient positions allows for target areas to be treated thoroughly, without the distortion and compression from the operating table seen when using a single supine position, or even in supine/prone positioning. Three positions: Supine, lateral decubitus, and the opposite lateral decubitus allow for complete exposure of the body circumferentially while avoiding the more onerous and time-consuming prone position. As a caveat, if the operating surgeon is strongly one-handed, adding the prone position to the standard three position routine can help intraoperative assessment and prevent asymmetries. Additionally, multiple patient positions allow cross-hatching and help ensure complete treatment. It also reduces the risk of creating iatrogenic contour deformities.
MARKINGS (Fig. 57-4)
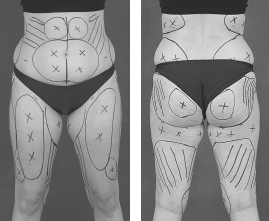
Fig. 57-4 Markings. Circled Xs are over zones of prominence, and lines are over zones of adherence.
■ Patients should be marked when they are in an upright position or standing.
■ Use marker to outline areas to be treated.
■ Mark zones of adherence and other areas to be avoided with parallel lines or cross-hatch marks.
INCISIONS
■ Longer for ultrasound-assisted liposuction (UAL) compared with suction-assisted liposuction (SAL) (6-8 mm versus 2-3 mm, respectively).
■ Incisions can be placed anywhere adjacent to areas being treated.
■ Multiple incisions are used for access to target areas, and ideally they are strategically located to allow crisscross suctioning.
• Liposuction from a single access incision may lead to contour deformity.
■ Locations (Fig. 57-5; Box 57-1)
Box 57-1 INCISION LOCATIONS FOR LIPOSUCTION
• Breast (male): Anterior axillary fold and/or periareolar
• Lateral back: Lateral bra line
• Vertical back: Midline
• Flank/hip: Sacral, groin crease, midaxillary line in panty line
• Abdomen: Lateral lower abdomen/suprapubic/umbilical
• Buttock: Sacral, midaxillary line in panty line
• Lateral thigh: Midaxillary line in panty line
• Posterior thigh: Midaxillary line in panty line
• Medial thigh: Medial groin crease and inguinal crease
• Anterior thigh: Inguinal crease
• Upper arm: Anterior and posterior axillary folds, olecranon radial elbow crease
LIPOSUCTION CANNULAS5
■ Most tips are blunt with multiple openings set back from the end to allow suctioning of fat with passage of the cannula.
• Blunt tips limit risks of penetration of unwanted structures such as fascia, peritoneum, vessels, and nerves.
■ Suction cannulas range from 1.8 mm up to 1 cm in diameter (typical use for liposuction is 2.5-5.0 mm) with varying cannula lengths.
• Larger suction cannulas are typically used for deeper tissue.
• As suction cannula size increases, the rate of fat removal with each pass increases, as does the risk of contour irregularities.
PHYSICS AND THEORY OF LIPOSUCTION6
■ SAL removes fragmented fat through a cannula and tubing into a receptacle.
■ Fragmentation of fat
• “Jackhammer effect”: The cannula striking fatty tissue
• The avulsion of fat into the islets of the cannula as the cannula moves in and out
■ Rate of fat aspiration
• Directly proportional to the diameter of the cannula and suction tubing
• Directly proportional to vacuum pressure
• Inversely proportional to the length of the cannula
• Poiseuille law concepts
► R = (L/r4) × K, where R is the resistance, r is the radius of the tube, L is the length of the tube, and K is a constant factor
WETTING SOLUTIONS
PURPOSES
■ Volume replacement
■ Hemostasis
■ Enhance cavitation (UAL)
■ Dissipate heat
■ Constituents vary, examples:
• 1000 ml of lactated Ringer solution at 21° C
• 30 ml of 1% lidocaine plain (15 ml if large volume)
• 1 ml of 1:1000 epinephrine
■ Klein recipe7
• 1000 ml normal saline solution
• 50 ml 1% lidocaine plain
• 1 ml 1:1000 epinephrine
• 12.5 ml of 8.4% sodium bicarbonate
► Alkalization may decrease pain with infiltration, but is not needed with general anesthesia.
WETTING SOLUTION TECHNIQUE8 (Table 57-1)
Table 57-1 Wetting Solution Infiltrate and Estimated Blood Loss by Technique
| Technique | Infiltrate | Estimated Blood Loss (as % volume) |
| Dry | None | 20-45 |
| Wet | 200-300 ml/area | 4-30 |
| Superwet | 1 ml infiltrate:1 ml aspirate | <1 |
| Tumescent | 3-4 ml infiltrate:1 ml aspirate | <1 |
Infiltrate may contain lidocaine, epinephrine, and/or sodium bicarbonate, depending on surgeon’s preference.
LIDOCAINE IN WETTING SOLUTION7,9–11
■ Analgesia is provided for up to 18 hours postoperatively.
■ Recommended maximum is 7 mg/kg in the presence of epinephrine (4 mg/kg in the absence of epinephrine).
■ The estimated maximum safe lidocaine dosage using the tumescent technique is 35 mg/kg.
• Peak plasma concentration is 10-14 hours after infiltration.
• Klein’s original study noted doses up to 52 mg/kg with no adverse effect; this has been confirmed in other studies.
• Objective signs of lidocaine toxicity at plasma concentration >5 µg/ml
■ Use of high quantities of lidocaine made possible because of:
• Diluted solution
• Slow infiltration
• Vasoconstriction of epinephrine
• Relative avascularity of fatty layer
• High lipid solubility of lidocaine
• Compression of vessels by infiltrate
LIDOCAINE TOXICITY12 (Table 57-2)
Table 57-2 Plasma Lidocaine Levels and Symptoms of Toxicity
| Plasma Level (µg/ml) | Symptoms |
| 3-6 | Subjective (circumoral numbness, tinnitus, drowsiness, lightheadedness, difficulty focusing |
| 5-9 | Objective (tremors, twitching, shivering) |
| 18-12 | Seizures, cardiac depression |
| 12-14 | Unconsciousness, coma |
| 15-20 | Respiratory arrest |
| >20 | Cardiac arrest |
LIPOSUCTION TECHNIQUES
SUCTION-ASSISTED LIPOSUCTION (SAL)8,13
■ Surgeon’s arm provides energy.
■ Movement of cannula results in mechanical disruption and avulsion to allow fat cell aspiration.
■ External source of suction to facilitate fatty tissue removal (usually 300-600 mm Hg)
ULTRASOUND-ASSISTED LIPOSUCTION (UAL)13–16
■ First described by Zocchi15 in 1992
■ Piezoelectric crystals in the probes convert electric energy into high-frequency sound waves that interact with tissue to create interstitial cavities and cellular fragmentation—a process termed, “cavitation.”
• Adipose is more susceptible than muscle, fascia, or neural tissue.
• The emulsified fat is then removed through the cannula.
• Heat is generated as a byproduct.
■ Use a hollow cannula or a solid probe.
■ UAL with improved contouring over SAL for fibrous areas such as:
• Upper abdomen
• Back
• Flanks
• Gynecomastia
■ Three-stage technique
• Stage I: Subcutaneous infiltration with wetting solution
• StageII: Ultrasound treatment to emulsify fat
• Stage III: Evacuation of emulsified fat and final contouring with SAL
■ Key factors to UAL
• The stroke rate is slower than with traditional SAL to allow time for cavitation.
• The dry technique should never be used with UAL (minimum superwet environment).
• The cannula/probe must be moving at all times to limit thermal injury.
• The endpoint is a loss of resistance to probe advancement (Table 57-3).
Table 57-3 Surgical Endpoints for UAL and SAL/PAL
| Endpoint | UAL | SAL/PAL |
| Primary | Loss of tissue resistance Blood aspirate | Final contour Symmetrical pinch test |
| Secondary | Treatment time Treatment volume | Treatment time Treatment volume |
PAL, Power-assisted liposuction; SAL, suction-assisted liposuction; UAL, ultrasound-assisted liposuction.
■ Complications of UAL
• Thermal injury (burn or blisters of skin)
• Seroma
• Hyperpigmentation
■ Superficial UAL
• Can result in increased skin retraction but at the risk of increased contour deformities
• Power settings and suction should be decreased compared to those used in deeper planes.
• Be careful to prevent thermal skin injury.
■ UAL advantages
• Decreased surgeon fatigue in more fibrous tissues
• May improve skin tightening
■ UAL disadvantages
• Equipment cost
• Slightly larger incisions
• Longer operative times
• Increased risk of thermal injury to skin
• Increased scarring in adipose tissue bed
• Cannula misguidance due to diminished cannula resistance
POWER-ASSISTED LIPOSUCTION (PAL)5,13,17,18
■ Augmented SAL with externally powered reciprocating cannula replicating the to-and-fro motion of the operator’s arm19
■ Approximately 2 mm motion at rates of up to 4000-6000 cycles/minute
• Electric energy source or medical grade compressed air
• Less wetting solution is required compared to UAL.
■ PAL advantages
• Decreased surgeon fatigue
• Large volumes
• Revision liposuction
• Shortened procedure times
■ PAL disadvantages
• Operator discomfort induced by vibrating handpiece
• Noise generation
LASER-ASSISTED LIPOSUCTION (LAL)5,17,20
■ Technique involves subcutaneous insertion of a laser fiber via a small skin incision.
• Fiber is either housed with a cannula or as a single fiber.
■ Most commonly used wavelengths in the United States
• 924/975 nm, 1064 nm, 1319/1320 nm, and 1450 nm
■ Laser acts to disrupt cell membranes and emulsify fat by photothermolysis.
• Different wavelengths vary in their effectiveness to preferentially target adipose cells and photocoagulation of small vessels while excluding surrounding structures.
■ Previously marketed for skin-tightening effect (mostly anecdotal)
• Theory: Heating of the subdermal tissue contributes to possible skin-tightening effect.
• Studies have shown no difference between LAL and conventional techniques.
■ Four-stage technique
• Stage I: Subcutaneous infiltration with wetting solution
• Stage II: Application of energy to the subcutaneous tissues with laser probe
• Stage III: Evacuation of emulsified fat with SAL
► Some advocate skipping this stage in smaller regions (neck) and allowing the body to absorb the liquefied contents.
• Stage IV: Subdermal skin stimulation
■ LAL advantages
• Decreased intraoperative blood loss
• Decreased postoperative ecchymosis
• Possible skin tightening (not confirmed)
■ LAL disadvantages
• Potential thermal injury to skin
• Equipment cost
• Prolonged procedure time
• Increased scarring in adipose tissue bed
• Cannula misguidance due to diminished resistance
WATER-ASSISTED LIPOSUCTION (WAL)21,22
■ Technique uses a dual-purpose cannula to emit pulsating, pressurized, fan-shaped jets of wetting solution with simultaneous suctioning of the fatty tissue and instilled fluid.
• Injected fluid loosens fat cells while minimizing surrounding soft tissue damage.
■ Can be done in office setting under local anesthetic
■ Two-stage technique
• Stage I: Subcutaneous preinfiltration with wetting solution
► A standard wetting solution for local anesthesia and vasoconstriction
• StageII: Simultaneous infiltration of “rinsing solution” and aspiration
► Lower infiltration setting and lower lidocaine concentration
• Endpoint: Final contour and pinch test
■ WAL advantages
• Reduced pain for patient
• Decreased need for general anesthesia
• Patient awake and able to change positions
■ WAL disadvantages
• Equipment cost
RADIOFREQUENCY-ASSISTED LIPOSUCTION (RFAL)23,24
■ Technique uses bipolar radiofrequency energy to disrupt the adipose cell membrane and facilitate lipolysis.
• A hollow cannula allows simultaneous aspiration of liquefied fat.
■ Allows a constant treatment depth
■ Controlled thermal injury at subdermal surface may lead to skin-tightening effect.
■ The external electrode has a thermal sensor that measures skin temperature to prevent thermal injury.
• Once the skin reaches 38°-42° C, thermal heating is complete and completion SAL or PAL contouring is then performed.
• Approximately 30% of aspiration occurs during RFAL.17
■ Three-stage technique
• Stage I: Subcutaneous infiltration with wetting solution
• Stage II: Radiofrequency energy treatment to emulsify fat
• Stage III: Evacuation of emulsified fat and final contouring with SAL or PAL
• Endpoint: Loss of resistance to forward motion rather than pinch or palpation
■ RFAL advantages
• Decreased surgeon fatigue, especially in fibrous areas
• Decreased ecchymosis
• Possible skin-tightening effect
■ RFAL disadvantages
• Potential thermal injury
• Equipment cost
• Prolonged procedure time
TIP: Thermal methods of liposuction (laser, ultrasonic, radiofrequency, and others) dramatically reduce cannula resistance within the tissues indiscriminately, narrowing the resistance differential between targeted and unwanted tissues. Thereby, surgeon precision is compromised as the tactile feedback is blunted. Additionally, these devices create a significant scar burden, and as the skin redrapes postoperatively, the fibrosis generated predisposes the patient to dermal adherence to underlying tissues, which can result in contour deformities and unnatural contours.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







