Fig. 17.1
Anatomy of the abdominal panniculus. The areolar layer (AL) and the lamellar layer (LL) are separated by the fascia superficialis (F). (a) Cadaver after performing liposuction on the right side of the abdomen. Three levels are marked on the abdominal cutaneous layer: (B) supraumbilical, (A) umbilical, (C) infraumbilical. The skin is pulled upward by three hooks to show the panniculus. The arrows indicate that the AL remains of normal thickness and the LL shows that the fat tissue was liposuctioned. The F is mixed up with lamellar layer. (b) Close-up showing the thickness of the AL with preservation of the perforator vessels and connective tissue of the LL after liposuction
The clinical and metabolic alterations showed that there were not any specific disturbances after liposuction in a comparative study with patients who underwent aesthetic procedures (reduction mastoplasty, abdominoplasty, rhytidoplasty) [4, 9]. Other surgeons studied the same subject and found similar results [10].
Nevertheless, a very high incidence of local complications after liposuction in conjunction with conventional abdominoplasty intrigued me so much that I became very discouraged about performing a combined approach owing to the psychological repercussions for patients [11, 12]. Thus, in 1988, I made a radical decision not to perform any more of these associated procedures [12]. There were enough reasons to avoid performing this type of surgery for 10 years, from 1988 until 1998. During this period of time, only conventional abdominoplasty was performed on patients without localized adiposities, or isolated fat suction to remove only localized adiposities without skin resection.
For these reasons, our generation of plastic surgeons had the privilege of starting to employ the liposuction technique to achieve better results than performing conventional panniculus resection, as other authors have described the complications [13, 14]. However, we had to learn and acquire our knowledge secondary to our own efforts, with meticulous observations after operations, with detailed descriptions in books, discussions at Congresses, and scientific articles in journals [5, 6].
Although the combined procedure was no longer being performed, research was into anatomy, in addition to the behavior of the remaining fat tissue, did not stop [8]. Study of the complications and research continued into a new approach to solve both deformities – the flaccidity and excess skin associated with the treatment of localized adiposities on the abdominal wall.
After a long period of anatomical study and analysis of my patients concerning the complications of conventional abdominoplasty, I came to the conclusion that the origin of such complications was mostly venous and lymphatic stasis, because the perforator vessels were damaged during panniculus dissection, according to the classical operation (Fig. 17.2).
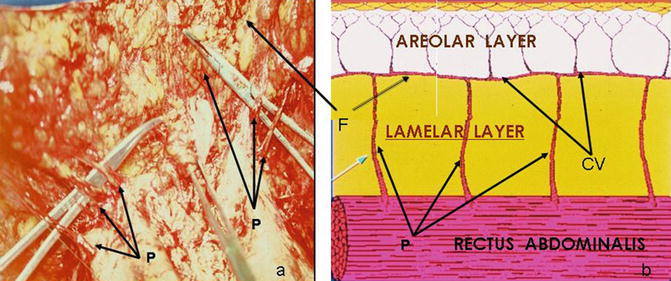
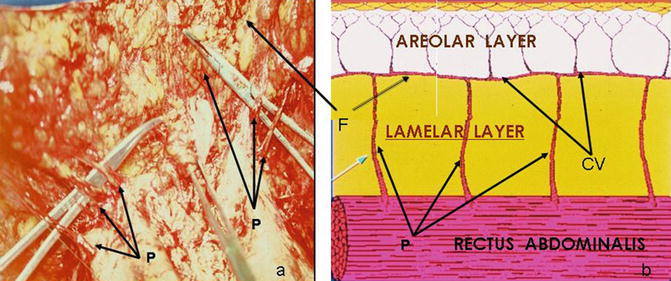
Fig. 17.2
The perforator vessels of the abdominal panniculus. (a) The forceps are introduced underneath the perforator vessels (P) preserved after the liposuction procedure. (b) Vascularization of the panniculus fascia superficialis (F) is located between the lamellar and areolar layers with the communicating vessels (CV). The perforator vessels (P) go from the rectus abdominalis to the fascia superficialis where the communicating vessels (CV) make a bridge of communication between them. Small vessels go perpendicular through the fat tissue of the AL to supply blood to the subdermis and dermis. Photos courtesy of Caia and Batuira
Following my anatomical research, the perforator vessels coming from the rectus abdominalis to the remaining panniculus were preserved after fat suction. Based on that unknown moment, I spoke with Prof. Callia about my scientific curiosity when he gave me some slides on which he showed me that the perforator vessels really were preserved after the liposuction procedure (Fig. 17.3). In fact, conventional abdominoplasty was carried out in a group of his female patients 6 months after the liposuction operation had been performed because they had complained about excessive redundant skin. I carefully analyzed his slides and compared them with mine, taken from my previous anatomical research in cadavers (Fig. 17.1). I concluded that it would be possible to perform panniculus resection combined with liposuction, as long as the perforator vessels were preserved. In addition, he gave me other slides showing a comparison between the behavior of the panniculus of a thin person and another one after liposuction properly performed on the lamellar layer (Fig. 17.3). Therefore, I found out that some skin with no fat tissue underneath could be removed with minimal bleeding, as the perforator vessels were not cut. For this reason, I am thankful to Prof. Callia for his encouragement in showing the right direction in which to follow my anatomical research to understand that mysterious knowledge concerning the behavior of perforator vessels after liposuction and also after panniculus resection.
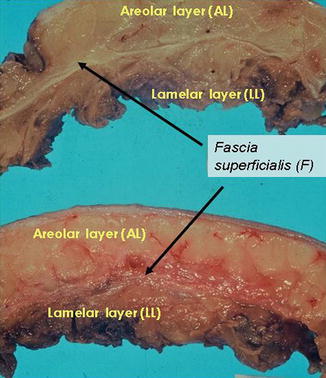
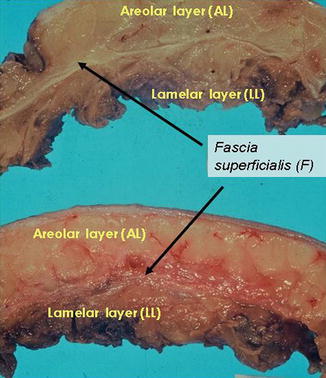
Fig. 17.3
Relationship between the AL and LL with the fascia superficialis. (Top) Section of a thin cadaver without liposuction. The AL is regular above the F, which is thin and well defined; the LL is thin and has no adiposity. (Bottom) Panniculus of a patient’s abdomen 6 months after liposuction. The AL maintains its regularity; however, the F and LL are mixed up because of the trauma caused by the cannula. Photos courtesy of Callia and Batuira. I am thankful to the latter for the uncharted segment, which is a fundamental support to learning the anatomy of the panniculus to develop lipoabdominoplasty
After 10 years of studying the anatomy, I concluded that it would be possible to perform liposuction associated with skin resection, without undermining the panniculus to maintain the perforator vessels. In fact, this is the basis of the concepts to improve abdominoplasty that I was obsessively pursuing.
The anatomical studies motivated me to perform on cadavers a full-thickness suction of the subcutaneous tissue in an elliptic area in the suprapubic region in addition to the medial thigh with localized adiposity. Afterward, skin resection was performed and similar structures to those found in cadavers after the liposuction procedure [8] were identified, which provided fundamental information. Liposuction was carried out afterwards below the fascia superficialis, that is, underneath the areolar layer of the panniculus, which slides from one border to another to facilitate the suturing of the surgical wound (Figs. 17.1 and 17.2). At that moment, I was sure that such an operation could be performed safely without any bleeding during and after surgery.
The first patients were operated on in early 1998, 10 years after the author’s radical decision to stop performing the combined procedures of liposuction with skin resection. The first was a female patient presenting an unaesthetic and deep surgical scar in the suprapubic region (Fig. 17.4). The second was another female patient with dark and thick skin and localized adiposity in the medial thigh region. First, the excess skin that should be removed was demarcated and also the area in which fat suction was to be performed. The operations were successfully carried out via the liposuction procedure on a full thickness area of skin, which was removed afterward without bleeding. Following the operation, liposuction was performed underneath the remaining panniculus without undermining it, and the border of the skin was sutured.
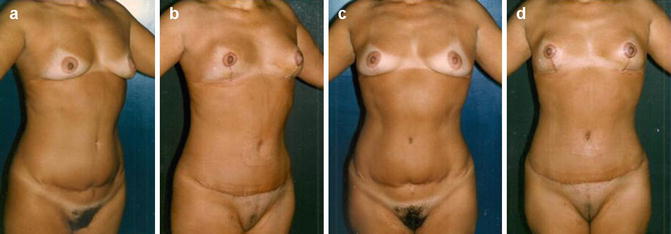
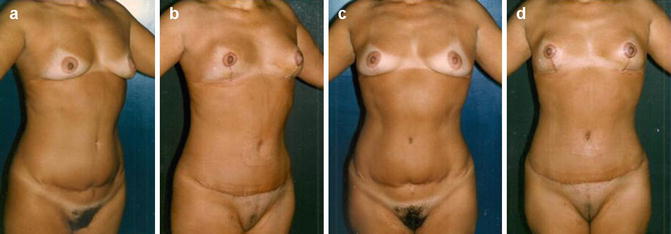
Fig. 17.4
A 53-year-old woman presented high and deep scars owing to previous abdominoplasty performed elsewhere and ptotic breasts. (a, c) Preoperative. (b, d) After lower lipoabdominoplasty in association with mastopexy
At that time, it was concluded that a new procedure could be performed to suction the accumulated fat combined with skin resection due to the redundant cutaneous covering after fat suction with minimal complications. In the original publication [15], this method was employed in 24 patients who underwent abdominoplasty combined with liposuction, which is a procedure performed in a closed vascular system as there was no damage to the perforator vessels, which is the main and essential concept of lipoabdominoplasty. To preserve the perforator vessels is the fundamental surgical principle of my new method, as the cannula does not damage the vessels coming from the muscles to supply the remaining fat layer of the panniculus (Fig. 17.2). Another surgical principle is that each perforator vessel (artery, veins, lymphatics, and nerves) is not cut, which works as multiple pedicles of the remnant areolar layer, which provides a smooth and regular surface on the abdomen wall after surgery. The same method was employed in 38 patients for the treatment of medial thigh lift [16]. Also, similar operations were carried out in eight patients for flankplasty and torsoplasty (Fig. 17.5) [17] as they presented cutaneous folds combined with an excess of localized adiposities. I employed the same surgical principles for the treatment of axillary regions in 21 patients [18].
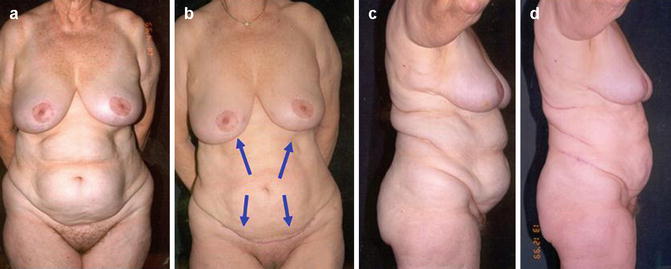
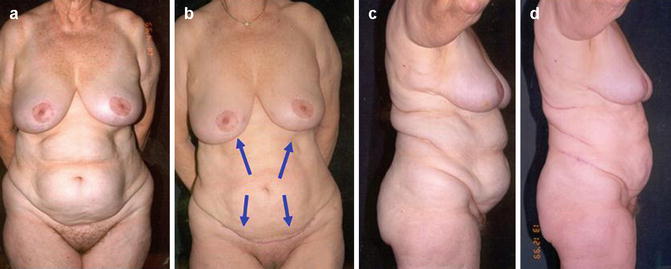
Fig. 17.5
A 75-year-old showing excess adipose tissue on the abdomen, flanks, and dorsum. She had previously undergone mastoplasty and had asked for abdominoplasty, but upper and lower lipoabdominoplasty was performed. (a, c) Preoperative. (b, d) After surgery demonstrating the improvement of the body contouring. The inframammary scars are hidden in the mammary sulcus. The arrows on b show the direction of traction of the abdominal panniculus
Therefore, the final conclusions of the new approach were to treat not only the abdominal wall, as the whole body may present localized adiposities and redundant skin as well. Owing to my anatomical investigations, several segments of the human body were adequately repaired with minimal complications using the same surgical principles, which are to preserve the perforator vessels to work as multiple pedicles to the abdominal wall, medial thigh lifting, flanks, and torso, and in the axillary regions.
After all of my presentations and publications, other surgeons started to perform and to speak about the new concepts and surgical principles regarding abdominoplasty [34–36], in one case without giving me the credit at the end of 2001 [37]. In fact, this was Saldanha’s first publication and presentation concerning abdominoplasty following my surgical principles that he learned from the publications and presentations.
17.3 Traditional Abdominoplasty
Abdominoplasty has been performed since nineteenth century for aesthetic treatment of the abdominal wall by abdominal lipectomy firstly described by Kelly (1899) [38] through elliptical horizontal skin resection with adipose tissue including the umbilical area. This was the beginning of a long and rich history along the last century followed by many other authors with horizontal incision as Malbec (1948) [39], Callia (1965) [40], Pontes (1966, 1982) [41, 42], Pitanguy (1967, 1977) [43, 44], Sinder (1975, 1979) [45, 46], vertical incision by Babcock (1916) [47], circular incision proposed by Gonzales-Ulloa (1960) [48], Vilain and Dubousset (1964) [49], submammary incision by Thorek (1939) [50], Rebello and Franco (1972) [51], Rebello (1982) [52], and recently I have introduced a half-moon-shaped skin resection in bilateral submammary folds [15].
Nevertheless, liposuction procedure was developed and popularized by Illouz [53, 54] (1980, 1992), which is the first surgical method for aesthetic treatment of the abdominal wall without performing skin resection. However, the use of lipoplasty enabled only localized adiposity as the skin excess and musculoaponeurotic disturbances require traditional techniques. Therefore, the indication of fat suction is restricting to patients presenting only localized adiposities on the anterior abdominal wall. When patients presenting with localized adiposities associated with excess skin require the combined procedure in which my method may be employed with smooth and harmonious results on the abdomen, medial tight lift, flanks, torso, upper extremities, face lifting, ear reconstruction, and on the reverse lower blepharoplasty.
17.3.1 Technique
The surgeon and patient must have a precise idea of what can be accomplished by lipoabdominoplasty and try to achieve the best for both. Some steps are essential for the success of the operation, which starts during a period from the first appointment until the final decision to schedule it. Didactically, they may be presented as:
A.
Surgical evaluation of the patients
B.
Selection of patients
C.
Surgical planning
D.
The operation
Selection and classification of the procedures
Type 1 – lower lipoabdominoplasty
Type 2 – upper lipoabdominoplasty
Type 3 – lower and Upper lipoabdominoplasty
Type 4 – full lipoabdominoplasty
(a)
Surgical demarcations
(b)
Liposuction procedure
(c)
Full-thickness skin resection
(d)
Creation of the new umbilical region during full lipoabdominoplasty
(e)
Plication of the musculoaponeurotic wall
(f)
Traction of the remaining panniculus and final suture
(g)
Bandaging
17.3.1.1 Surgical Evaluation of the Patient
Prior to surgical evaluation, during consultation the surgeon must listen attentively to the complaints and even expectations of the patients concerning her or his body contouring. Although the abdomen is the only segment patients are mostly concerned with, the entire body may be evaluated. Abdominal examination is performed initially with the patient in the standing position between two vertical mirrors, one in front of the other, and another mirror is situated at a 45° angle on the top. The patient must not be wearing any clothes and the nurse always on the side following the examination, which is good support for both patient and doctor. The patient is given the possibility of seeing his or her body from the front and back at the same time while the abdomen is evaluated. The posterior regions of the dorsum and lateral silhouette on each side are seen as well (Figs. 17.6 and 17.7). It is useful for a patient to follow the physical examination as quite often he or she presents some sort of body asymmetry that has not been noticed before (Fig. 17.8). Therefore, it is possible to evaluate the elasticity of the skin, the accumulation of adiposity, musculoaponeurotic laxity, and the presence of scars due to previous surgeries and if there is some asymmetry in the abdominal wall and in the posterior regions. The abdomen is measured in three circumferences: (a) the hypochondriac circumference, (b) the umbilical circumference, and (c) the iliac crest circumference. Also, the vertical measurement in the midline is necessary to evaluate the possibility of skin resection during surgery (Figs. 17.9 and 17.10). The ideal candidate for abdominoplasty is normal in weight for his or her stature and height. Usually, in a normal person, when the distance between the external furcula to the umbilicus is less than 38 cm, it may jeopardize blood supply to the remaining abdominal panniculus if all of the skin resection in the suprapubic region is done. It is more convenient to carry out the operation when this distance is greater. On the other hand, when the distance between the umbilicus and the pubis is more than 15 cm, it may be difficult to perform skin resection in all regions as it is mandatory in full lipoabdominoplasty. Under such circumstances, limited suprapubic resection is indicated without transposition of the umbilicus as occurs in lower abdominoplasty (Fig. 17.4). Therefore, location of the umbilicus is a good aesthetic and anatomical reference point concerning the selection of patients before performing abdominoplasty.

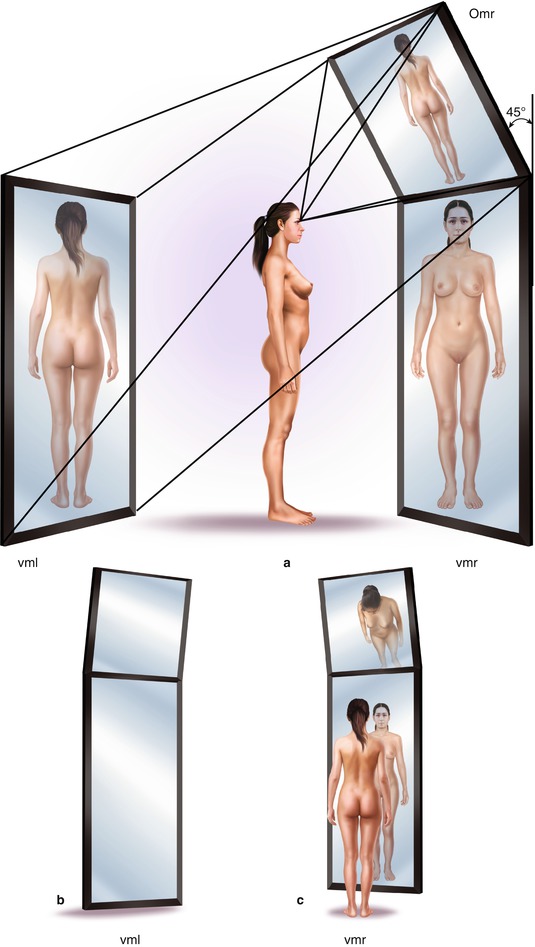

Fig. 17.6
Examination room with mirrors. thm top horizontal mirror, Oml 45° oblique mirror on the left side, Omr 45° oblique mirror on the right side, vml vertical mirror on the left side, vmr vertical mirror on the right side, b bed for patient’s examination in supine position
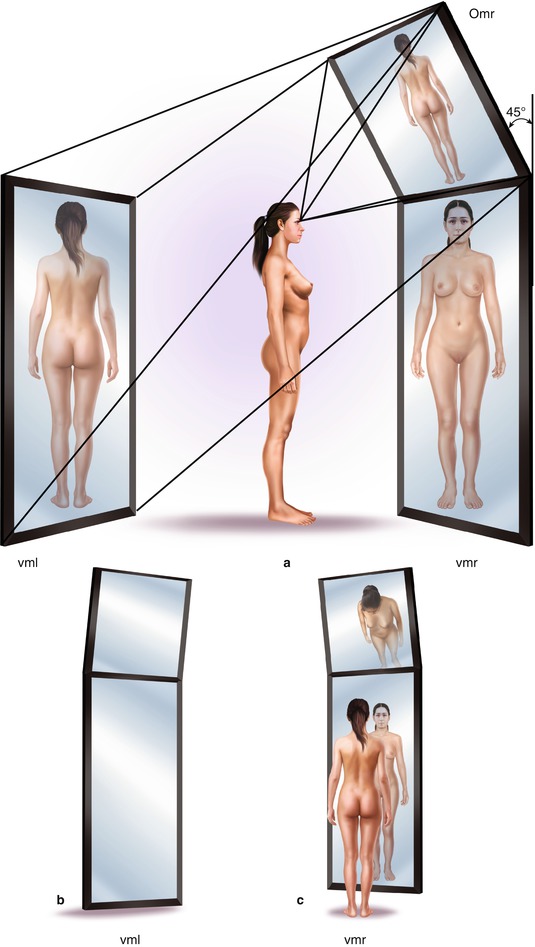
Fig. 17.7
Examination room with mirrors. (a) A female patient is in a standing position between the two vertical mirrors, vml and vmr. She can see herself from the front on the vmr and simultaneously she can see her back vml through the omr. (b) Vertical mirror on the left (vml). (c) Vertical mirror on the right (vmr) with a female patient in the standing position. She can see herself in front and from the back through the oblique mirror on the right (omr)
Fig. 17.8
Lower lipoabdominoplasty combined with torsoplasty to repair body asymmetry. (a–e) Preoperative 48-year-old female patient. (b, d, f) After lower lipoabdominoplasty in conjunction with torsoplasty following the same surgical principle, which is preservation of the perforator vessels
Fig. 17.9
Preoperative measurement of a patient in the standing position during consultation, (a) Vertical distance from the external furcula to the pubic bone; (b) vertical distance from the external furcula to the umbilicus; (c) horizontal circumference at the hypochondriac level; (d) circumference at the umbilical level; (e) circumference at the iliac crest level
Fig. 17.10
Measurement of a patient in supine position on a bed during a consultation. (a) vertical distance from the sternal notch to the pubic bone. (b) Vertical distance from the sternal notch to the umbilicus. (c) Patient taking a picture of herself while supine on bed through the top horizontal mirror (thm), while the surgeon measures her vertical distance
Afterwards the patient is placed in the supine position on the table with another mirror situated horizontally above so that he or she can see the deformities. At this time, it is important to evaluate the elasticity of the skin, the thickness of the abdominal panniculus, and muscular flaccidity as well. The patient can follow the examination through the mirror on top, which shows the alterations of the abdominal wall (Fig. 17.10). When there is a hernia of the umbilicus and diastasis of the rectus abdominalis is evident, it is useful to show these to the patient. The amount of excess skin may be carefully evaluated by placing the thumbs at the lateral borders of the symphysis pubis and grasping the abdominal pannicullus between the thumbs and fingers of each hand. When this maneuver is done with patient in the standing position, he or she may follow the examination on the vertical mirror strategically placed in front and at the back (Fig. 17.7). On the other hand, when the patient is supine on the bed, she or he follows the surgeon’s hands on the horizontal mirror placed on top. Patients may take pictures of their abdomen with the camera, which is a document that demonstrates that he or she understands the abdominal deformities in addition to the indication for operation (Fig. 17.10). This assessment indicates the feasibility of bringing the periumbilical skin down to the suprapubic skin where the incision will be made. Flexion of the hips further aids evaluation as it simulates the desired patient position for closure of the abdominal wall incision at the right point during surgery.
17.3.1.2 Selection of Patients
This is an important step prior to performing any procedure on the abdominal wall. Before a patient comes to the surgeon’s office, he or she has already selected his or her surgeon. In the same way each surgeon should also choose his or her patients. Therefore, after physical examination, each surgeon has enough time to evaluate if a patient is physically and psychologically healthy before planning the operation. In the case of patients who are psychologically unstable, complain too much about the results and scars, demonstrate unrealistic expectations of postoperative results, in addition to many other undesirable circumstances, it is the right time to cancel the operation [11, 12]. Also, patients presenting overweight should not be selected for abdominoplasty or liposuction, since such problems cannot be solved adequately through surgery.
A good understanding between the surgeon and the patient is mandatory before surgery. Even when patients seem to understand all about the proposed operation, they may have some sort of problem in accepting the surgical result or complications that sometimes occur despite all the care and attention postoperatively.
Excess adipose tissue on the abdominal wall, muscular flaccidity, diastasis of the rectus abdominalis, hernia, cutaneous striae, and unaesthetic scars on the abdomen give an unpleasant appearance to the body, requiring appropriate surgical treatment of damaged structures, which are good indications for abdominoplasty. However, when a patient presents only localized adiposity in the subcutaneous layers of the abdominal wall without any other anatomical disorder, liposuction is the best technique for treatment. It may occur in female and male patients of several age groups.
17.3.1.3 Surgical Planning
According to clinical evaluation and the selection of patients, the surgical planning of lipoabdominoplasty without panniculus undermining may be classified into four types of operation: lower lipoabdominoplasty, upper lipoabdominoplasty, upper and lower lipoabdominoplasty, and full lipoabdominoplasty.
Type 1: Lower Lipoabdominoplasty
Lower lipoabdominoplasty is a procedure comprising skin resection combined with liposuction for the repair of abnormalities on the lower segment of the abdomen, which is located below the umbilical area, specifically the suprapubic region. The main surgical principle is the preservation of perforator vessels, which work as multiple pedicles as the remaining panniculus is not undermined. Very often, gynecological surgeries or other operations on the infraumbilical area may also leave unaesthetic scars, sometimes retractile cicatricial tissue, or several other undesirable circumstances. With this approach, the umbilicus is not transposed owing to the very high implantation, as there is quite a long distance between the navel and the pubis. When patients present localized adiposities on the supraumbilical segment, even on the lateral and posterior regions of the torso, these must be treated simultaneously, popularized as mini-abdominoplasty [55, 56].
Type 2: Upper Lipoabdominoplasty
Upper lipoabdominoplasty is an operation comprising half-moon incisions with skin resection associated with liposuction of the submammary folds without damaging the perforator vessels, which work as multiple pedicles to the panniculus. Its indication is limited to the treatment of some deformities of the upper abdomen. When the abnormalities are restricted to localized adiposity, specifically the epigastric and hypochondriac regions, it is possible to achieve good aesthetic results during isolated fat suction. However, when there is redundant panniculus, it is not possible to reach adequate surgical results without performing skin resection. Unfavorable aesthetic results after superficial liposuction of the superior abdomen may also be adequately repaired. The first description regarding panniculus resection of the upper abdomen was reported by Thorek (1923) [50], and later Rebello and Franco (1972) [51] published on abdominoplasty through a submammary incision. This approach leaves a long scar on the anterior aspect of the chest, which is the main reason why it did not became popular among plastic surgeons.
Nevertheless, there are peculiar circumstances in which female patients present excess accumulated fat and flabby skin on the upper abdomen (epigastric and lateral regions), which is the main deformity indicating the need for upper lipoabdominoplasty. For this reason, this type of lipoabdominoplasty will be covered in this section, but it is useful to mention other information regarding the subject before a technical description of the surgery.
Type 3: Lower and Upper Lipoabdominoplasty
Lower and upper lipoabdominoplasty is a new approach with double treatment of the lower and upper abdomen in association with skin excision plus liposuction without transposition of the umbilicus [17]. Although two cutaneous incisions are made, the perforator vessels are not incised which is the fundamental surgical principle for providing normal vascularization to the remaining panniculus. In fact, the abdomen may be improved from the aesthetic point of view once the physical deformities are corrected and treated adequately. The surgical planning requires careful evaluation preoperatively when the high location of the umbilicus is the main anatomical reference point. Also, it is indicated in patients presenting inelegant and unaesthetic aspects of the abdomen due to unfavorable results of superficial liposuction.
Type 4: Full Lipoabdominoplasty
Full lipoabdominoplasty is a modality of operation through which all skin above the suprapubic region and below the umbilicus must be resected. In fact, the whole abdominal wall is treated, but the perforator vessels are not cut as the remaining panniculus is not undermined according to my original description [15, 22]. This is the main difference between my technique in comparison with conventional abdominoplasty when wide undermining is performed and all perforator vessels are cut. Once again, it is important to emphasize the importance of preoperative evaluation before planning the operation, particularly the measurement of the anatomical points regarding the location of the umbilicus. The surgeon must hold the panniculus below the umbilicus and be sure that it is possible to resect. The skin of the periumbilical area can be approximated to the suprapubic incision, which means that the upper abdomen can be pulled downward.
17.3.1.4 The Operation
After the previous steps described above the surgeon might have enough information to choose an adequate procedure for performing abdominoplasty. In all types of operation, all patients must present a normal blood test in essential examinations in addition to fundamental clinical evaluation performed by the physician, in which ECG and other specific examinations are carried out when necessary. A complete series of photos of the regions to be treated must already have been obtained.
The author performs all operations at the hospital under epidural or general anesthesia, where patients stay for at least 24 h. I prefer to demarcate the patient’s body the day before the operation. I consider it more convenient as I can see the patient’s deformities once more and explain to him or her all the details. The patient must remain in a standing position in front of the mirror, as is described on the section “Surgical Evaluation” so as to follow my drawing on his or her body. After careful analysis, all deformities are drawn. Two areas must be well demarcated: (1) The area for full-thickness skin resection where liposuction will be performed on the full thickness of the panniculus, and also to point out the location of the final scars. (2) The areas for deep liposuction (below the fascia superficialis) on the abdominal wall and in the lateral and posterior regions.
Selection and Classification of the Procedures
Type 1: Lower Lipoabdominoplasty
Lower lipoabdominoplasty is indicated when the patient presents moderate flaccidity of the panniculus and excess skin associated with localized adiposity in other regions of the torso. During surgical planning, it is mandatory to evaluate the amount of cutaneous resection to be done and the volume of fat to be removed by suction.
(a)
Surgical demarcation
The excess skin forms an elliptical area in the suprapubic region below the umbilicus. The umbilicus is not transposed. The areas presenting localized adiposity are marked on the abdomen and other regions of the torso as well (Fig. 17.11).
Fig. 17.11
Lower lipoabdominoplasty technique. (a) Demarcation for skin resection in the suprapubic area. (b) Liposuction procedure on the full thickness of the panniculus. (c) Skin resection is carried out. (d) Deep liposuction is performed below the fascia superficialis with preservation of the perforator vessels, which work as multiple pedicles providing a normal blood supply to the remaining abdominal panniculus
(b)
Liposuction procedure
Two types of liposuction are performed: full thickness of the panniculus and deep liposuction. First, liposuction is performed on the full thickness of the panniculus where skin resection is to be done. After this procedure, there is no fat tissue underneath the skin as the areolar and lamellar layers are aspirated, leaving only connective tissue, empty vessels, and lymphatics. Afterward, deep liposuction is carried out in all regions of the abdominal wall presenting localized adiposity. It is performed on the lamellar layer (below the fascia superficialis) to maintain a regular and harmonious thickness of the areolar layer (Fig. 17.11). It is useful to emphasize that when the areolar layer is damaged, the surface of the abdomen may have an unaesthetic wave-like appearance, which is difficult to remedy afterward. My previous publication [15] described the anatomy of the panniculus and its importance in preserving the perforator vessels on the lamellar layer.
After the liposuction procedure, the cutaneous and subcutaneous panniculus above the raw area slides easily over the musculoaponeurotic wall as there is no fat tissue below the fascia superficialis. The perforator vessels do not disturb the movement of the upper abdominal flap from top to bottom.
(c)
Full-thickness skin resection
The incisions are made according to the previous demarcations and are followed by full-thickness skin resection. This is preferably performed by using a knife, because if scissors are used at this stage, they may damage the vascular network of the subdermal layer, causing bleeding. After skin excision, it is possible to see that the perforator vessels were preserved during the previous liposuction procedure, as the panniculus is not undermined.
(d)
Plication of the musculoaponeurotic wall
When diastasis is evident, plication of the musculoaponeurotic wall may be performed in the midline. The perforator vessels indicate the location of the rectus abdominalis, which is helpful in identifying and suturing the internal borders of the muscles and the aponeurosis.
Before the liposuction technique, Callia (1965) [40] proposed sectioning the umbilical pedicle after panniculus undermining of the infraumbilical segment so as to be able to perform plication of the musculoaponeurotic wall in the midline (Fig. 17.12). Afterward, the umbilical pedicle is reimplanted at the muscular level. This situation demonstrates once again the importance of careful evaluation preoperatively, including measurement of the distances from the external furcula to the umbilicus, and from the umbilicus to the pubis. The author performs Callia’s procedure combined with liposuction without any undermining of the panniculus, which means that all perforator vessels are preserved. The plication of the muscular aponeurotic wall is performed from the level of the rib margin to the pubic area.
Fig. 17.12
Reinforcement of the musculoaponeurotic wall during lower lipoabdominoplasty without transposition of the umbilicus. (a) Abdominal panniculus is pulled upward after full-thickness liposuction and skin resection were performed in the suprapubic area. (b) Scissor sectioning of the umbilical pedicle according to Callia’s procedure through which it is possible to suture the rectus abdominalis in the midline from the upper abdomen to the pubis. (c) After plication of the muscles the pedicle of the umbilicus is sutured to it. (d) The remaining abdominal panniculus with the umbilicus pulled upward and the perforator vessels going from the rectus abdominalis to the panniculus
(e)
Traction of the remaining panniculus and final suture
Following the operation, the remaining panniculus is pulled downward and the wound is sutured at three levels. As described above, in the raw area there are only connective tissue, fascia superficialis, and empty perforator vessels, as after suctioning of the fat tissue they naturally collapse. In all perforator vessels the artery, veins, lymphatics surrounding them, and also a thin layer of subdermal tissue are present. The first level of suturing is the fascia superficialis, to approximate the border of the upper flap to the lower border, which avoids any scar depression after surgery. Afterward, the subdermal layer is folded over itself and sutured, and finally an intradermal running suture is applied to close the incision.
(f)
Postoperative dressing
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







