Brian P. Maloney, William Truswell IV, and S. Randolph Waldman, address questions for discussion and debate:
- 1.
Is surgery ever a better alternative than injectable fillers for enhancement of the lips?
- 2.
What role do permanent lip implants play for today’s patients?
- 3.
How do you manage the small-mouthed person seeking lip enlargement?
- 4.
How do you handle down-turning corners of the mouth?
- 5.
How do you handle a person who previously had full lips but now is losing volume, especially in the corners?
- 6.
What qualities of the lip are important to preserve when considering various lip augmentation materials and techniques?
- 7.
What are the best ways of reducing the length of the upper lip?
- 8.
Analysis: Over the past 5 years, how has your technique or approach to lips changed, or what is the most important thing you have learned in performing lip augmentations?
Brian P. Maloney, William Truswell IV, and S. Randolph Waldman, address questions for discussion and debate:
- 1.
Is surgery ever a better alternative than injectable fillers for enhancement of the lips?
- 2.
What role do permanent lip implants play for today’s patients?
- 3.
How do you manage the small-mouthed person seeking lip enlargement?
- 4.
How do you handle down-turning corners of the mouth?
- 5.
- 6.
- 7.
What are the best ways of reducing the length of the upper lip?
- 8.
Video of surgical technique of subnasal lip lift and advancement of lower lip accompanies this article. Available at : http://www.facialplastic.theclinics.com/
Is surgery ever a better alternative than injectable fillers for enhancement of the lips?
Maloney
Yes, surgery may be a better alternative for the patient with thin lips and poor definition of Cupid’s bow. For the patient with congenitally thin lips, the vermilion advancement is an excellent means of increasing the amount of vermilion show. This procedure can be combined with lip augmentation procedures if additional bulk is desired ( Fig. 1 ).

Surgery is also an excellent procedure for the patient who desires lip augmentation; however, the upper lip may be too long and the patient may display no incisor show. Augmenting the lips in this case would only make the lip longer, throwing the lips more out of balance. A nasal-base resection would be a better alternative to augmentation. Once the length of the lip is shortened, augmentation can be performed if necessary.
Acellular human dermal matrix graft augmentation of the lips can be an excellent means of creating more vermilion show in a thin-lipped patient. This surgical procedure is performed through a single incision in each commissure; a submucosal tunnel is created, and the matrix can be placed into both upper and lower lips.
When cosmetic surgeons attempt to create large lips from small ones by injecting fillers, the end result is generally a duck-bill, stiff, sausage-like look to the lip. The most commonly used lip fillers are hyaluronic acid fillers. By their physical nature they are liquids. Liquids by definition take the shape of their containers. It is very difficult to stretch a vermilion with a liquid filler and have it result in a natural long-lasting change. With increasing refinements of hyaluronic acid, newer products offer a higher degree of cohesiveness. Cohesiveness refers to the molecules’ ability to stay together and resist being dispersed. For high-motion areas that require augmentation, these highly cohesive fillers will offer more semisolid properties; however, the end result of overfilling with the latest fillers generally is an overdramatic feature.
I have found multiple V-Y advancements of the entire wet lip surface as an augmentation technique to result in a bulky lip with poor movement. Lips are very dynamic in nature, and any surgical procedure needs to maintain a soft flexible lip to allow it to function properly. Man-made implants such as those using expanded polytetrafluoroethylene (ePTFE) and saline as fillers, tend in my experience to restrict lip movements and often result in extrusion when placed in the upper lip. The lower lip is more tolerant of the implants because of its more basic structure and movement.
Truswell
Surgical lip enlargement should be considered in patients with very thin lips for whom injectable fillers or implants would be more distorting than enhancing. The best way to help these patients, in my opinion, is to perform a direct lip lift, a subnasal lip lift, or a V-Y augmentation. All of these procedures have varying results and can be fraught with complications.
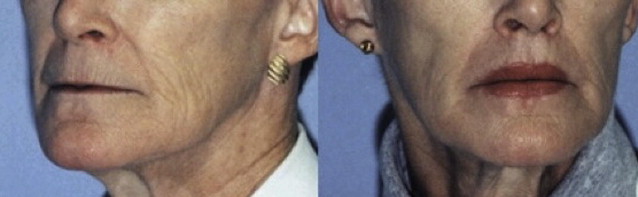
Direct lip lifting is performed by excising a portion of the white lip and advancing the mucosa upward as an advancement flap. This technique will shorten the white upper lip. The incision should be placed above the white roll of the upper lip to preserve this feature. Meticulous closure is paramount in minimizing the scar that will occur. The patient must understand this issue. The scar can be camouflaged with dermabrasion or laser resurfacing. Lipstick can hide it, as can cosmetic tattoo. If not done with skill and precision, the scar can be emotionally and socially debilitating ( Figs. 2 and 3 ).

The subnasal lip lift is another technique designed to shorten the white lip while elevating the red lip. This procedure is done by excising a strip of skin with the incision placed just below and precisely following the gentle curve of the nasal sill. The remaining lip is elevated as an advancement flap and carefully sutured in place. Difficulties with this procedure include scar formation and the fact that this will only elevate the middle third of the upper lip.
V-Y lip augmentation is a surgical approach that avoids skin incisions, therefore avoiding problems with cutaneous scarring. Good results require an exacting technique. Multiple V-Y flaps shift lateral tissues centrally to lift and add fullness to the lip. The lips can be projected forward by this technique, which can leave the patient with an unpleasant pucker. The thin, aged lip will not lend itself readily to this procedure. The postoperative course for this surgery can be prolonged, with considerable swelling and down-time for the patient.
Waldman
Only in extreme situations and after lengthy conversation with the patient do we consider a surgical approach over the use of injectable fillers. Surgery is only appropriate for the rejuvenation patient who might present with increased distance between the vermilion and the base of the nose and also demonstrating loss of philtral architecture. In addition, there are situations whereby the corners of the mouth are so dependent that injectable fillers have no chance at success. In this situation we may consider a corner-of-the-mouth lift. This operation has been well documented, as has the subnasal lip lift, in a previous issue of this journal. It is important to remember that there are specific indications and also anatomic prerequisites for either the subnasal lip lift or the corner-of-the-mouth lift. If these parameters are not present then surgery should not be considered.
What role do permanent lip implants play for today’s patients?
Maloney
At this time, other than autologous fat or human acellular dermal matrix graft, I do not recommend “permanent lip implants.” I have found that because of the high motion of the lip area, autologous fat may resorb. Success rates can be increased by asking the patient to limit lip movements for the first 2 weeks after the procedure to help with graft revascularization. In an unpublished multicenter study by Maloney, Waldman, and Kridel (1997), acellular dermal matrix grafts were found to result in lip augmentation for at least a year for 89% of the study patients.
Permanent injectable implants may include polymethylmethacrylate (PMMA) beads coated with cow collagen, or microdroplet silicone. Although the PMMA filler is on at least the third generation, I have seen so many reactions present from earlier generations that I do not consider it an option ( Fig. 4 ). Multinucleated giant cells are known to surround both PMMA and microdroplet silicone. These cells may stay dormant for several years and then be activated. The end result can be swollen, red, tender nodules.

Over the years I have placed ePTFE lip implants in the upper and lower lips, only to see most of them extrude from the upper lip. I am concerned that recent modifications incorporating saline-filled lip implants would have the same result. This shortcoming is due to a basic difference between the embryology of the upper and lower lip, and their resultant movements. The upper lip flexes much more than the lower lip with speech, and therefore makes it less tolerant than the lower lip with regard to implants. I believe it is the complex movement of the lip as opposed to the configuration of the ePTFE that is the greatest challenge to be overcome with lip implants.
Truswell
For some time now the public has shown an increasing desire for procedures that are quick and affordable with the expenditure of no or minimal down-time. The results they seek are ones that are effective and long lasting, if not permanent.
One drawback of injectable fillers is that they are generally, in the short or long term, temporary with the exception of injectable silicon. The wish for a permanent solution has led to the development of soft-tissue implants. These materials include ePTFE, silicone gel, and silicon rubber (for nasolabial folds) among others. The ideal permanent implant will have the properties of ease of placement with little down-time, softness, no visibility, good biocompatibility and biointegration, no patient rejection, long-term predictability, minimal to no shrinkage, no migration, the ability to individualize the implant to the patient, ease of removal, and affordability. These attributes exist with the implants of ePTFE material.
The implants are not well suited for patients with very thin lips that have little vermilion showing. Otherwise they are an excellent choice for any patient wishing a permanent solution for lip augmentation. The implants insert readily with local anesthesia, and are soft and natural in appearance. The dual-porosity ePTFE implants have excellent biocompatibility and biointegration, allowing cellular ingrowth into the framework of the strands. These implants have little to no adverse effects on the motion and function of the lips and oral commissure, and do not alter the shape of the lips or mouth. I have had extensive experience with dual-porosity ePTFE lip implants and have inserted more than 250 of them. I have had only one extruded, owing to infection. One patient had them replaced for shrinkage of less than 10% longitudinally. The implants are well tolerated and do not interfere with lip function, from whistling to kissing.
Waldman
Some physicians will use silastic implants to augment a younger person’s lips. Such an approach is one we have not yet attempted, although we have not ruled it out should long-term results demonstrate patient satisfaction and minimal problems.
Previously we were among the first to use ePTFE for lip enhancement, but the material demonstrated too many variables in the healing process and we abandoned this procedure in favor of the new improved group of temporary injectable fillers. Other materials that have been tried but have not stood the test of time include cadaver dermis, dermal-fat grafts, and injectable silicone. In general, however, I would say that whatever we use in the lips must be easily reversible, that is, no residual damage to the lips following removal!
Remember the phrase on many of our diplomas that reminds us “Physician first do no harm.” Too often we forget this as aesthetic plastic surgeons.
What role do permanent lip implants play for today’s patients?
Maloney
At this time, other than autologous fat or human acellular dermal matrix graft, I do not recommend “permanent lip implants.” I have found that because of the high motion of the lip area, autologous fat may resorb. Success rates can be increased by asking the patient to limit lip movements for the first 2 weeks after the procedure to help with graft revascularization. In an unpublished multicenter study by Maloney, Waldman, and Kridel (1997), acellular dermal matrix grafts were found to result in lip augmentation for at least a year for 89% of the study patients.
Permanent injectable implants may include polymethylmethacrylate (PMMA) beads coated with cow collagen, or microdroplet silicone. Although the PMMA filler is on at least the third generation, I have seen so many reactions present from earlier generations that I do not consider it an option ( Fig. 4 ). Multinucleated giant cells are known to surround both PMMA and microdroplet silicone. These cells may stay dormant for several years and then be activated. The end result can be swollen, red, tender nodules.
Over the years I have placed ePTFE lip implants in the upper and lower lips, only to see most of them extrude from the upper lip. I am concerned that recent modifications incorporating saline-filled lip implants would have the same result. This shortcoming is due to a basic difference between the embryology of the upper and lower lip, and their resultant movements. The upper lip flexes much more than the lower lip with speech, and therefore makes it less tolerant than the lower lip with regard to implants. I believe it is the complex movement of the lip as opposed to the configuration of the ePTFE that is the greatest challenge to be overcome with lip implants.
Truswell
For some time now the public has shown an increasing desire for procedures that are quick and affordable with the expenditure of no or minimal down-time. The results they seek are ones that are effective and long lasting, if not permanent.
One drawback of injectable fillers is that they are generally, in the short or long term, temporary with the exception of injectable silicon. The wish for a permanent solution has led to the development of soft-tissue implants. These materials include ePTFE, silicone gel, and silicon rubber (for nasolabial folds) among others. The ideal permanent implant will have the properties of ease of placement with little down-time, softness, no visibility, good biocompatibility and biointegration, no patient rejection, long-term predictability, minimal to no shrinkage, no migration, the ability to individualize the implant to the patient, ease of removal, and affordability. These attributes exist with the implants of ePTFE material.
The implants are not well suited for patients with very thin lips that have little vermilion showing. Otherwise they are an excellent choice for any patient wishing a permanent solution for lip augmentation. The implants insert readily with local anesthesia, and are soft and natural in appearance. The dual-porosity ePTFE implants have excellent biocompatibility and biointegration, allowing cellular ingrowth into the framework of the strands. These implants have little to no adverse effects on the motion and function of the lips and oral commissure, and do not alter the shape of the lips or mouth. I have had extensive experience with dual-porosity ePTFE lip implants and have inserted more than 250 of them. I have had only one extruded, owing to infection. One patient had them replaced for shrinkage of less than 10% longitudinally. The implants are well tolerated and do not interfere with lip function, from whistling to kissing.
Waldman
Some physicians will use silastic implants to augment a younger person’s lips. Such an approach is one we have not yet attempted, although we have not ruled it out should long-term results demonstrate patient satisfaction and minimal problems.
Previously we were among the first to use ePTFE for lip enhancement, but the material demonstrated too many variables in the healing process and we abandoned this procedure in favor of the new improved group of temporary injectable fillers. Other materials that have been tried but have not stood the test of time include cadaver dermis, dermal-fat grafts, and injectable silicone. In general, however, I would say that whatever we use in the lips must be easily reversible, that is, no residual damage to the lips following removal!
Remember the phrase on many of our diplomas that reminds us “Physician first do no harm.” Too often we forget this as aesthetic plastic surgeons.
How do you manage the small-mouthed person seeking lip enlargement?
Maloney
Beauty by definition is a face that is in proportion and balance. Surgically creating a larger mouth can be challenging. Therefore, I begin my physical examination by evaluating the patient’s overall facial proportions. If the lower third of the face has squared off because of excess facial fat or ptosis of the cheek fat pad caused by aging, the mouth will appear smaller. For the most patients as they age, the ratio of the width of the face to the width of the mouth increases. If the face can be narrowed by facial liposuction or a facelift, I will discuss these options with the patient. If a patient has thick facial skin, I may also discuss partial or total removal of the buccal fat pad in an attempt to narrow the width of the face ( Fig. 5 ).










