Leg ulcers and wound healing
Anna Rich RN (Dip BSc Hons)
John SC English FRCP
Introduction
Leg ulceration is a common and often debilitating problem. A leg ulcer can be defined as a loss of skin below the knee on the leg or foot, which takes more than 6 weeks to heal1. They affect 1-2% of the population and are more prevalent in females2. Venous leg ulceration is the most common aetiology (70-90%), followed by arterial (5-20%), and mixed venous and arterial ulceration (10-15%)3. These ulcers can also be affected by other underlying (e.g. diabetes) and unusual aetiologies (e.g. pyoderma gangrenosum), which may occur simultaneously and may also occur in isolation; they account for 5-10% of ulcers. The key to successful management of leg ulceration relies upon thorough assessment, establishment of a diagnosis, and treating the underlying pathology4.
This section on leg ulceration discusses the important factors involved in assessment and investigations to be considered. Aetiology of the more common types of leg ulceration will be presented as well as consideration for differing diagnosis. The main principles of leg ulcer and wound management and common therapies will also be discussed.
Clinical presentation
Venous disease
Venous leg ulceration arising from venous disease usually occurs as a result of incompetent valves in the deep and perforating veins. Incompetence of these valves results in a backflow of blood from the deep to the superficial veins, leading to chronic venous hypertension. Predisposing factors such as a previous medical history of deep vein thrombosis (DVT), lower limb fractures, varicose veins, phlebitis, pulmonary embolism, previous venous ulceration or a family history of leg ulceration or thrombosis, as well as standing occupations, limb trauma, or multiple pregnancies may be suggestive of venous disease. Obesity is an increasing cause of venous incompetence.
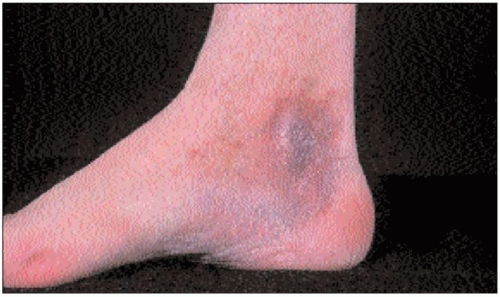
Ulcer site: ulcer is most likely to occur around the medial or lateral aspect of the gaiter area of the lower limb (10.1, 10.2).
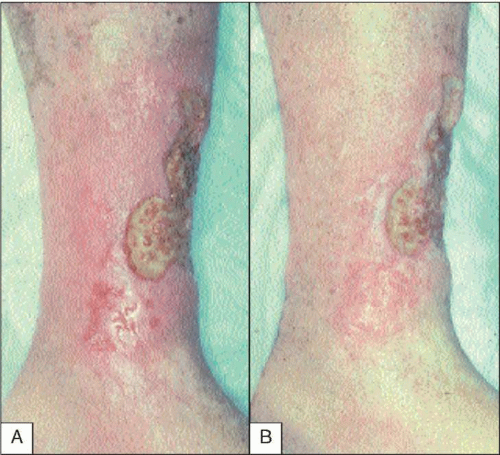
Ulcer appearance: venous leg ulcers tend to be shallow in appearance (10.3).
Pain: patients may complain of localized pain or a generalized aching/heaviness in their legs.
Limb appearance/skin changes:
Haemosiderin staining: brown/red pigmentation of the skin of the lower limb occurs as a result of the release of haemosiderin (a breakdown product of haemoglobin). It is released owing to distension of vessel walls and leakage of red blood cells into interstitial space (10.4).
Varicose eczema: eczema of the lower limb associated with venous hypertension; can be aggravated by allergic contact dermatitis from the medicaments used (10.5).
Ankle flare: chronic venous hypertension can result in the distension of tiny veins on the medial aspect of the foot/ankle (10.6).
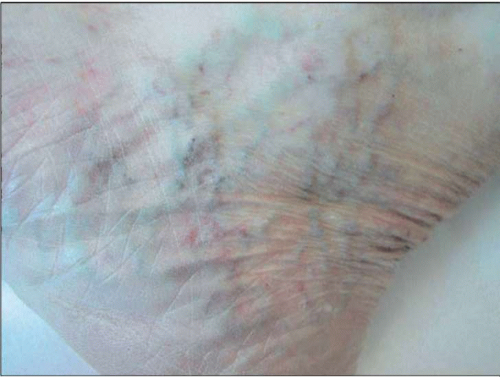
Atrophy blanche: areas of white skin, stippled with red dots of dilated capillary loops (10.7).
Varicose veins: distended veins, a sign of chronic venous hypertension usually due to damaged valves in the leg veins, which become dilated, lengthened, and tortuous (10.8).
Dermatoliposclerosis: ‘woody’ induration of tissues and fat, replaced by fibrosis (10.9).
Oedema: oedema tends to be generalized and worsens as legs are dependent as the day goes on; reduction in oedema is reported upon elevation of the limb(s) or after spending the night in bed (10.10).
 10.3 Venous ulceration and severe maceration from ulcer exudate. A potent topical steroid in addition to the compression will help healing in this situation. |
Arterial disease
Poor arterial supply as a result of narrowing or occlusion of the vessels may lead to tissue ischaemia and necrosis. Predisposing factors such as a previous medical history of myocardial infarction, transient ischaemic attacks, cerebral vascular attack, hypertension, diabetes, rheumatoid arthritis, peripheral neuropathy or diabetes, or a history of being a smoker may be suggestive of arterial disease.
Ulcer site: ulcers may be sited anywhere around the lower limb or foot.
Ulcer appearance: arterial ulcers tend to be deeper and more punched out in appearance (10.11, 10.12).
Pain: patients may complain of severe pain, worse at night or on elevation of the limb. They may also complain of intermittent claudication, cramp-like pain in the calf muscles brought on by walking a certain distance and relieved upon rest.
Limb appearance/skin changes:
Poor tissue perfusion and reduced capillary refill; absent or difficult-to-locate pedal pulses.
Loss of hair on the lower leg and the skin may appear atrophic and shiny, with trophic changes in the nails.
Muscle wastage in the calf.
The limb/foot may be cool to the touch with colour changes evident, pale when raised and dusky pink when dependent (10.13).
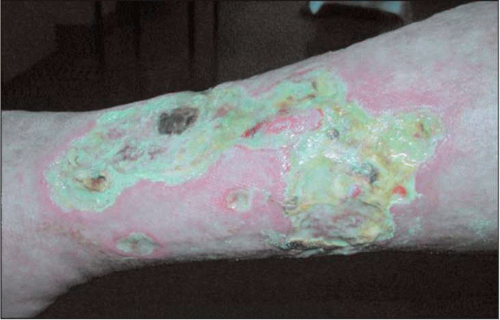
 10.14 Severe ulceration in mixed vessel disease. This ulcer responded very well to larva therapy.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|