Lateral Cheek and Posterior Auricular Transposition Flap
R. O. DINGMAN
G. H. DERMAN
EDITORIAL COMMENT
An alternative to the procedure diagrammed in Figure 111.1 would be to continue the incision parallel to the nasolabial fold into the neck to create a large, posteriorly based flap and to advance it superiorly. A transverse cut across the neck with a back cut would be needed.
The posterior auricular transposition skin flap provides an excellent donor source to close soft-tissue defects in the buccal and parotid-masseteric areas. Even large areas can be reconstructed by this flap alone or with additional transposition, advancement, or bilobed flaps (1, 2, 3, 4) (Figs. 111.1 and 111.2).
INDICATIONS
Primary closure of defects or local flap reconstruction is complicated by the proximity of important anatomic structures that are fixed or easily distorted when tension is applied. Important among these are the facial nerve, ears, lips, eyelids, nose, and hairline. Exact or close matches of skin color, texture, and contour are prime considerations because of the highly visible location of these areas and the concern regarding an optimal aesthetic result.
ANATOMY
The posterior auricular transposition flap is composed of non-hair-bearing skin and a thin layer of subcutaneous tissue overlying the superficial cervical fascia covering the
sternocleidomastoid, occipitalis, and posterior auricular muscles anteriorly as well as the superior portions of the splenius capitis, semispinalis capitis, and trapezius muscles further posteriorly. The platysma muscle is present sometimes at the extreme anterior portion of the flap base. This muscle is not included in the flap but is left in place to protect the cervical and mandibular branches of the facial nerve.
sternocleidomastoid, occipitalis, and posterior auricular muscles anteriorly as well as the superior portions of the splenius capitis, semispinalis capitis, and trapezius muscles further posteriorly. The platysma muscle is present sometimes at the extreme anterior portion of the flap base. This muscle is not included in the flap but is left in place to protect the cervical and mandibular branches of the facial nerve.
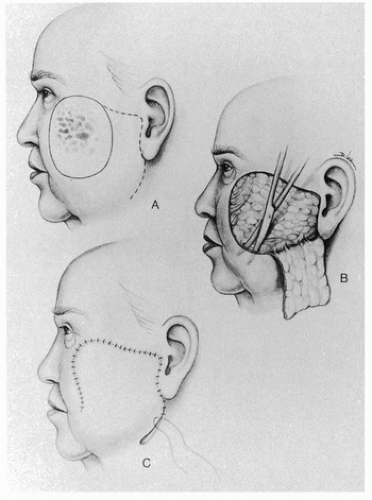 FIGURE 111.1 A-C: This older patient with a large amount of lax skin of the cheeks had malignant degeneration of a deeply pigmented lesion of the left face. The diagnosis was malignant melanoma. The lesion was excised with moderately wide margins and closed by development of a large cheek-neck flap advanced and rotated into the defect. If the single flap is not adequate for closure of the defect, it can easily be combined with a postauricular transposition flap (see Fig. 111.3).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





