Advances in anatomical research have created the base for a vast variety of flaps that can be raised in the hand. They are either based on the palmar arterial system or on the dorsal vascular system, which is fed by either perforating vessels from the palmar side or the dorsal arterial system nourished by dorsal carpal arterial network. The majority of small to moderate size defects in the hand can be reconstructed with these types of flaps.
Advances in anatomical knowledge, progress in surgical instrumentation, and innovative surgical techniques have significantly changed soft tissue reconstruction of the hand. Continual improvements in design and harvesting techniques have led to flap refinements, resulting in improved aesthetic and functional results following soft tissue reconstruction. This holds true for microsurgical free flaps, as well as for regional flaps, such as the intrinsic flaps in the hand.
Soft tissue defects of the fingers resulting in exposed tendons, bones, or joints are frequently encountered in hand surgery. Reconstruction can be challenging if the principle of replacing like with like is followed. Extensive literature is available concerning the variety of local and regional flaps that may be used for coverage of these defects.
Intrinsic flaps in the hand can be classified by
Vascular anatomy (axial/random pattern)
Donor site location
Perfusion pattern
Tissue components included.
Following descriptions by Littler and Bunnell, soft tissue reconstruction in the hand was limited to a small variety of flaps, often resulting in unsatisfactory results, due to considerable donor site morbidity and long rehabilitation times.
This changed with the first descriptions of dorsal metacarpal flaps by Earley and Milner as early as 1980. Their work was based on anatomical dissections performed by Manchot, Salmon and Spalteholz, who described the vascular architecture of the hand. Although, this knowledge was available, it was not applied in reconstructive surgery until the authors’ excellent results were reported. These publications also ignited a new wave of research in the vascular anatomy of the hand.
Much of the research was focused on the interconnections between the palmar arterial system and its perforating vessels into the vascular network of the dorsum of the hand.
In the last 20 years, many new flaps have been developed. These are based on small perforating vessels supplying defined skin areas mostly on the dorsal, but also on the palmar side of the hand. Due to the delicate nature of the feeding vessels, harvesting techniques have relied on microsurgical techniques. The authors have coined the term microsurgery without anastomosis for these dissection techniques. Since these flaps are raised within the territory of the hand and based on intrinsic vessels, they have been named intrinsic flaps.
This article will provide an overview of the most commonly used intrinsic flaps of the hand, covering the well-known dorsal metacarpal flaps, as well as some more exotic flaps that can be used for particular indications under suitable anatomical conditions. This article includes the anatomical base for the intrinsic flaps, harvesting techniques, indications, and the important tricks and pitfalls that should be considered to achieve the optimal results. With these flaps the majority of small-to-moderate-sized defects in the hand can be reconstructed with minimal donor site morbidity and excellent functional results.
Anatomy
Anatomical knowledge is the basis for successful flap surgery. Understanding the location of tiny perforating vessels, the angiosomes supplied by them, and their connective network to vascular system is essential in order to raise a well-perfused flap that can be reliably rotated or transferred into a defect.
The vasculature of the hand is based on 2 major feeding vessels, the radial and the ulnar artery. Although they are constant, their contribution to the perfusion of the hand varies significantly. Together with both interosseus arteries (posterior and anterial), they feed the carpal network of the wrist by forming a system of palmar and dorsal transverse arches.
The common digital arteries and their cutaneous perforators provide the blood supply of the palm. Two palmar arches (the superficial and deep palmar arch) are formed by the terminal divisions of the ulnar and radial artery and many communications in the palm. The main tributary of the deep palmar arch is the radial artery, while the ulnar artery mainly supplies the superficial palmar arch.
The common digital arteries arise from the superficial palmar arch and run distally until they reach the web space, where they divide into a pair of proper digital arteries. Proximal to their division, the common digital artery usually gives off a branch that runs dorsally to connect with the dorsal metacarpal arterial system.
The palmar metacarpal arteries originate from the deep palmar arch and run distally along each metacarpal. At the metacarpophalangeal (MP) joint they divide into 2 arches, which connect the palmar with the dorsal metacarpal network and form an anastomosis between the deep, superficial palmar arch, the palmar and dorsal metacarpal arteries, and the common digital artery. This network provides the blood supply to the synovial sheaths and intrinsic muscles of the hand. At the MP and interphalangeal (IP) joints, transverse arches connect the palmar and dorsal arterial arches. Vincular vessels arise from the transverse arches to the flexor tendons and palmar structures. Similar to this arrangement, at the distal phalanx the 2 digital arteries connect through a terminal transverse arch and provide nutrient branches to the nail germinal matrix.
Frequently used flaps
Homodigital Island Flaps
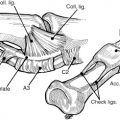
Homodigital island flaps are designed on the digital arteries as well as their concomitant veins. Grayson ligaments on the palmar side and Cleland ligaments on the dorsal side protect these vessels. From the digital arteries at the proximal interphalangeal joint (PIP) or distal interphalangeal joint (DIP) runs a palmar arch to provide retrograde blood flow, on which a retrograde pedicle can be harvested.
Due to the rich vascularization of the hand, flaps can be harvested on a proximal or distal pedicle. Proximally based flaps are called antegrade flaps. Flaps that are nourished by distal inflow are called retrograde flaps. Retrograde flaps can be used to cover distal defects over the DIP or the PIP. These are usually insensate flaps, but can be reinnervated when defects of the fingertips are reconstructed. The proper digital nerve is then included and reconnected to the distal stump of the contralateral proper digital nerve at the defect site. Antegrade flaps usually do not reach further than the PIP, but can also be employed to reconstruct defects over the MP joints or the distal metacarpals.
Antegrade flaps are ideally centered over the feeding vessels and should not exceed an arc of rotation of 90° to 120°, whereas reverse pedicle flaps may have up to 180° rotation arc, with an increased risk of kinking of the pedicle. Adding 10% to 15% more length to the pedicle, avoiding the use of narrow tunnels for the pedicle, and using a loose closure of the wound should avoid these complications. The size of the flap should be slightly bigger than the size of the defect, due to shrinking of the harvested flap.
The donor site can be closed primarily in many cases. A full-thickness skin graft should be employed, when primary closure is not possible, to achieve an inconspicuous donor site ( Figs. 1 and 2 ).