Fig. 25.1
Potential hernia sites in laparoscopic RYGBP. (1) entero-enterostomy mesenteric defect; (2) space between mesentery of Roux and transverse mesocolon (Petersen’s space); (3) transverse mesocolon defect. All the procedures fashioning a Roux-en-Y limb result in mesenteric defects that may potentially cause IH (From Iannelli et al. [1])
However, even if the occurrence of IH has been described above all after RYGBP, this complication can potentially occur after all the bariatric procedures in which a Roux-en-Y limb is fashioned because of the creation of mesenteric defects [3]. A mean rate of 2.51 cases of IH after Roux-en-Y gastric bypass has been reported [1]. The rate of IH should raise up to 8.4 % in case of non-closure of mesenteric defects [2].
As a matter of fact, the ever increasing use of laparoscopic approach results in an increased incidence of IH when compared to open procedures, maybe because of the reduced formation of postoperative adhesions [4].
Finally, even the weight loss plays an important role in the high incidence of IH as a consequence of the reduction of intra-abdominal adiposity that may lead to the expansion of pre-existent mesenterical defect [1, 5].
IH often remains a misdiagnosed disease or an incidental finding because symptoms may be very vague and other clinical hypothesis are advocated. On the other side, it can present with an acute and dramatic clinical picture that can oblige the general surgeon to face an unusual disease.
An appropriate knowledge of bariatric techniques may help the general surgeon to recognize this potentially lethal complication in order to refer suspect cases of IH to bariatric surgeons and to assure the best care to patient presenting with most urgent symptoms.
25.2 Clinical Presentation and Management
The occurrence of IH after laparoscopic bariatric surgery has largely been reported in the literature and it is well known by bariatric surgeons. However, it still represents a challenge for general surgeons who do not have a specific knowledge of the bariatric techniques. Moreover, a certain diagnosis is often difficult because of the clinical presentation that can be vague and not so easy to recognize.
IH may present as either an acute or chronic clinical picture. In the first case, symptoms are usually evident and the surgeon has to face a dramatic acute abdomen secondary to intestinal ischemia or small bowel necrosis or perforation. When an acute clinical presentation is present, the indication to emergency surgery is evident and a surgical operation is always required. In these cases, an IH must always be researched by examining the whole small bowel. The laparoscopic exploration is a valid option if the surgeon is skilled in laparoscopy and if he knows the technical details of the reconstructions of bariatric surgery.
The diagnosis of IH may be more difficult if the patient presents with less evident clinical picture. In case of chronic IH, symptoms are little evident and not easy to recognize, laboratory and traditional radiological work-up are often unhelpful [6]. CT scan could help for the diagnosis of IH but a clear diagnosis remains difficult because often only indirect signs of intestinal obstruction can be found [7].
CT scan should be systematically examined by skilled radiologist and surgeons for these findings: direct or indirect signs of small bowel obstruction, mesenteric swirl, a thicken shape of the mesentery, mesenteric vessel engorgement, small bowel behind the superior mesenteric artery, displacement of the mesenteric trunk and jejuno-jejunostomy standing on the right side [2, 8].
A chronic IH hernia often presents with vague, colicky pain, which may change or disappear in the lateral decubitus. Nausea and postprandial vomiting may be present. The pain can mainly be localized in the left upper quadrant, even if other localizations are possible, and often resolves spontaneously [1, 9].
The presence of recurrent abdominal pain in a patient with a past history of RYGBP, even in absence of pathological laboratory or radiological findings, should raise the suspicion of a misdiagnosed IH. In these cases, a surgical exploration should be advocated and should be performed by laparoscopy by a surgeon with a good knowledge of bariatric techniques.
At the surgical exploration, the bowel can have an inflammatory aspect with signs of intestinal obstruction. In some cases, a chylous ascites can be found, associated or not with a white coat on the mesentery, maybe because of a lymphatic stagnation secondary to the intermittent torsion of the mesenteric vessels (Fig. 25.2).
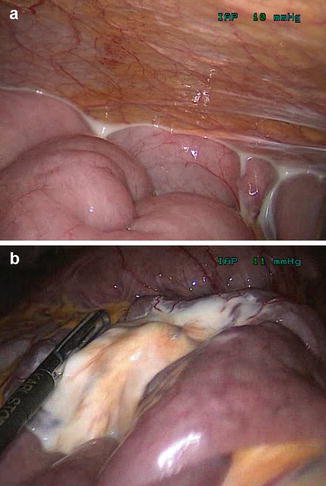
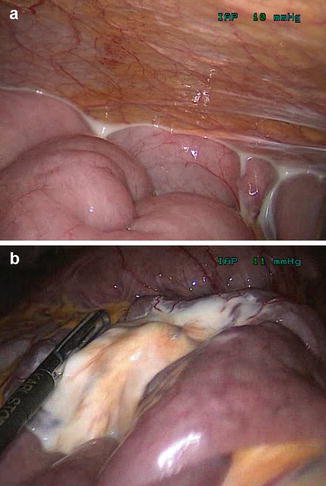
Fig. 25.2
Chylous asitis (a) and white mesenteric coat (b) in a case of internal hernia. This phenomenon may be due to lymphatic stagnation secondary to the intermittent torsion of the mesenteric vessels
At the surgical exploration, the whole small bowel must be examined and all the potential mesenteric defects must be researched. The aspect of the herniated bowel must be observed in each case in order to evaluate if a resection is needed. All mesenteric defects identified, above all if they gave origin to a symptomatic IH, should be closed.
We herein describe the technique that we usually use to perform laparoscopic exploration in patients with clinical or radiological suspicion of IH.
The patient is placed in the supine position with both legs in the straight position and secured to the operating table to allow for subsequent tilting. The surgeon stands on the patient’s right side with the assistant on his right side and the monitor is placed at the right side of the operating bed. The first 10-mm trocar is placed at the umbilicus, using an open technique and two 5-mm trocars are placed in the right flank. The 10-mm port will be used to introduce a 30° camera. The operating bed is tilted to the right side.
The procedure should start with the identification of the gastro-enterostomy. If the anastomosis is not evident because of some adhesions between the gastric pouch and the liver, it is probably better not to dissect but just to identify the alimentary limb.
In case of trans-mesocolic placement of the alimentary limb, an IH at the transverse mesocolon defect must be researched. An IH hernia at this site is often easy to recognize.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







