16 Infraorbital / upper and lower eyelids
Summary and Key Features
• Successful periorbital rejuvenation demands close attention to patient’s desires and expectations, general anatomical variations, detection of subtle asymmetries, and individualized treatment
• Careful patient selection requires a thorough exploration into the patient’s desired outcome and concerns, a detailed medical and cosmetic history, and a thorough and comprehensive aesthetic assessment
• Precise placement of injections and accurate / individualized dosing are crucial in obtaining the most beneficial effects and avoiding adverse events
• Small doses in the lower lid can minimize infraorbital rhytides and widen the eye
• BoNT may also be used to correct eyelid malposition, including ptosis and asymmetry
• Poor patient selection, inappropriate injection techniques, and diffusion of the toxin can lead to serious adverse events and complications
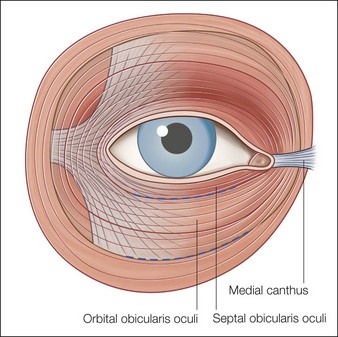
Anatomy of the eye
Complete knowledge and understanding of both dynamic and volumetric changes in the face, as well as the interaction between and function of various facial musculature and the surrounding soft tissue, are critical to ensuring successful outcomes with the use of BoNT in the periorbital region. Although in-depth examinations of facial anatomy have been published elsewhere, this chapter focuses on the anatomy of the eye relevant to the use of BoNT in the upper and lower eyelids (Fig. 16.1).
Patient assessment and selection
A complete medical and ophthalmic history is necessary, including previous experiences with rejuvenation procedures, surgery, and any other conditions that might influence treatment plans or outcome. The degree of rhytides and their potential response to treatment can be assessed via the Glogau photoaging scale (Table 16.1). Moreover, the quality of skin around the eye will also determine a treatment plan: patients with excessive skin above the eye, prominent fat pads in the lower lid, septal fat herniation, or severe elastosis (identified by a positive snap test), may require additional rejuvenating procedures such as laser or light-based therapies or even surgery prior to augmentation. All findings (including any sign of ptosis or asymmetry) should be noted and discussed with the patient, and standard digital photographs taken both before and after any treatments. Photographs should display the face in repose and at maximal expression to document changes on animation.
Table 16.1 Wrinkle severity and rejuvenation requirements
| Group severity* | Description | Rejuvenation modalities |
|---|---|---|
| II | Moderate; wrinkles in motion | Responds well to BoNT alone |
| III | Advanced; wrinkles at rest | BoNT plus additional correction, such as soft tissue augmentation |
| IV | Severe; only wrinkles | BoNT plus deeper skin resurfacing for maximal improvement |
* Based on the Glogau classification of photoaging.
Not everyone is a candidate for BoNT therapy. Aside from general contraindications (Box 16.1), caution should prevail in patients with a history and especially complications related to previous lower eyelid blepharoplasty and injections avoided in patients with lower lid laxity, due to the risk of scleral show, pre-existing conditions that could be worsened by treatment, such as mid-facial paresis or symptomatic dry eyes, stable or progressive muscular dystrophic conditions causing blepharoptosis, or anyone with already-compromised function of the orbicularis oculi.
Box 16.1
Contraindications and precautions to periocular BoNT treatment
| Contraindications | Precautions |
|---|---|
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|