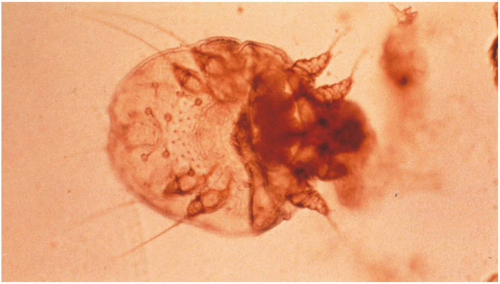
Scabies is a highly contagious, common parasitic infection, characterized by intense itching and superficial burrows. It is caused by the microscopic mite Sarcoptes scabiei. Scabies infections affect both males and females of all socioeconomic and ethnic groups. Transmission most often occurs through direct skin-to-skin contact, with a higher incidence occurring through prolonged contact within households or neighborhoods. For this reason, outbreaks are common in extended-care facilities, prisons, child care facilities, and schools. Less frequently, the mite is transmitted by indirect contact through fomites, and can live for up to 3 days on inanimate objects like bedding or clothing.
Clinical Presentation
The clinical presentation varies based on the type and location of lesions. Symptoms begin insidiously and are often mistaken for skin conditions such as dermatitis. Widespread pruritus is common, and severe nocturnal pruritus is the hallmark characteristic of scabies infection. Light pink curved or linear burrows, occasionally seen with a black dot on one end representing the mite, are pathognomic but not always seen. Scratching the area can destroy burrows (
Figure 13-2), displace mites, and promote the spread of mites to other locations on the body.
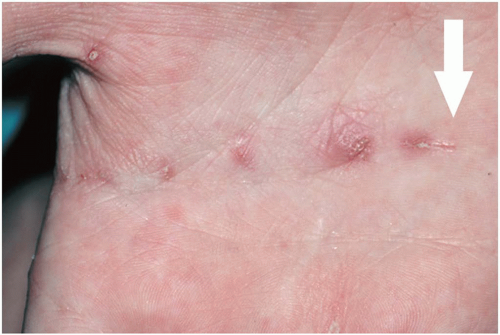
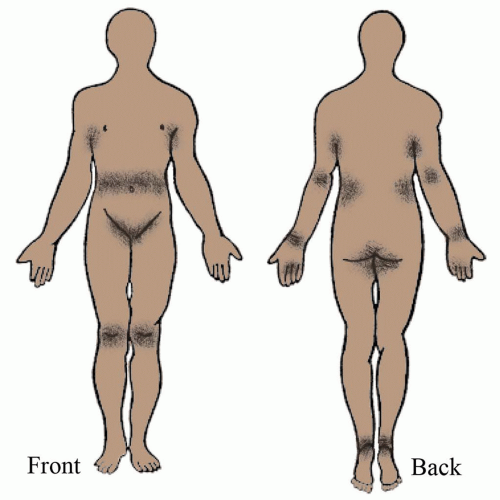
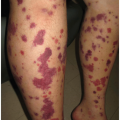
Older children and adults commonly present with red papules and vesicles that can be seen in the finger webs, wrists, lateral aspects of feet and hands, waist, axillae, buttocks, penis, and scrotum (
Figure 13-3). Infants and small children may develop pustules on the palms and soles, and in some cases the head and neck. A good rule of thumb is to always suspect scabies on men with pruritic papules on the scrotum or penis (diaper area for children) or nipple region in women. Nodules on the trunk and axillae may erupt as a result of the host’s exuberant immune response to the scabies.
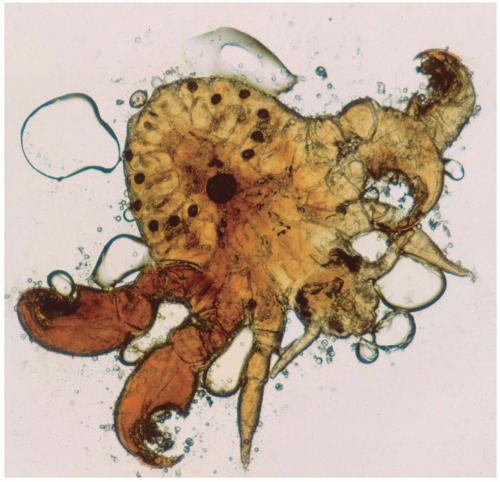
Crusted (Norwegian) scabies
Crusted scabies (also called hyperkeratotic or Norwegian) is severe and less common than general scabies infection. Patients at risk are the immunocompromised, elderly, and/or mentally or physically disabled. Compromised immunity, along with decreased itch sensation, leads to the infestations of hundreds to millions of mites. These patients classically present with asymptomatic, hyperkeratotic crusting on the palms and soles, thickened (dystrophic) nails, thick crusts and gray scales on the trunk and extremities, and verrucous
(wart-like) growths in areas of trauma (
Figure 13-4). Hair loss may also be present. Mites involved in crusted scabies are not more virulent than those found in traditional scabies infection; they are present in massive numbers. Individuals infected are highly contagious and therefore require quick and aggressive medical treatment.
Management
Management of scabies requires both pharmacologic treatment and environmental eradication. Topical permethrin 5% cream is the treatment of choice (
Table 13-1). Many of the topical treatments available are generally effective after one application; however, a second treatment after 1 week is common. Several second-line therapies are available, including topical sulfur 10% lotion and crotamiton 10% lotion, which has a higher failure rate of 40%.
Warning: Lindane 1% topical application, once considered the treatment of choice, is now FDA approved only for use in individuals who failed appropriate doses of other approved therapies or are intolerant to other treatments, in view of its neurotoxic side effects. In 2009, the American Academy of Pediatrics recommended that lindane not be used for children even as a second-line therapy. The state of California banned the use of lindane because of its reported neurotoxicity and environmental hazards.
Oral ivermectin, an antihelminthic agent, has been used off label for effective treatment of scabies with concurrent use of a topical scabicide. Ivermectin tablets, available in 3 mg, are dosed 200 µg per kg and may be repeated in 2 weeks. It should not be used in children under 5 years of age. Ivermectin is very effective in scabies epidemic and immunocompromised patients. Treatment for Norwegian scabies may require 200 µg per kg dose on days 1, 2, 8, 9, 15 and further doses on days 22 and 29, if severe.
Patients should be instructed on the appropriate application of topical scabicides. It is important to bathe prior to application, which is generally recommended at bedtime. Ensure fingernails are trimmed and clean. Apply topical scabicide to all skin from the neck down, ensuring all skin folds are treated, including finger and toe webs, under the fingernails, axillae, umbilicus, and the anal and vaginal clefts. Inadequate coverage is the primary cause of treatment failure. In infants, covering their hands with mittens helps prevent removal and ingestion of the product. If infection of the face or scalp is suspected, such as the case with infants or crusted scabies, also treat the skin above the neck, avoiding the eyes and mucous membranes. If the scabicide is washed off or removed prior to the required treatment duration, reapply more.
Once the recommended application time has lapsed, the patient may wash off the topical scabicide using soap and warm water. It is important to stress that only clean towels, clothing, and linens should be used to decrease reexposure. Members of the same household, including intimate contacts, should be treated empirically with topical scabicides at the same time as the infected patient. All clothing, bedding, and towels in contact with infected skin must be washed and dried on the hottest possible settings. Items unable to be washed may be sealed in a plastic bag for at least 1 week. Floors and chairs should be cleaned and vacuumed, while pets do not require treatment. Children may return to school and adults to work the day after treatment. Schools and workplaces may require a written statement from the patient’s health care provider.
Crusted scabies is more challenging to treat because of the thick, hyperkeratotic scale, making it difficult for topicals to penetrate and kill thousands of mites. Combination therapy with topical permethrin and oral ivermectin is frequently used. Despite treatment with scabicides, inflamed pustules, erosions, and crusts may occur
secondary to scratching. Pruritus associated with hypersensitivity to mites can last for up to 2 to 4 weeks after effective treatment.
Prognosis and Complications
Patients with scabies infections have an excellent prognosis with proper treatment. Postscabetic pruritus, associated with a hypersensitivity response, is common and may persist for weeks after treatment, despite scabies eradication. Properly treated patients should begin to show steady improvement in pruritus after about 2 to 3 weeks. Symptoms are typically managed with oral antihistamines (e.g., cetirizine, loratadine, or hydroxyzine) and topical corticosteroids. Short courses of oral corticosteroids are generally reserved for severe and intractable cases.
Secondary infections caused by Staphylococcus aureus or Streptococcus pyogenes may occur. Antibiotic use should be considered as indicated.
Patient Education and Follow-up
Patient education is an important step to successfully treating scabies infection. Patients should be educated not only on application technique of antiparasitic medication but also on household management of inanimate objects since mites can live up to 3 days off a human host. The Centers for Disease Control and Prevention (CDC) has up-to-date information on prevention, control, and institutional spread. Patients can be reassured that after full treatment they are able to return to school and work and resume normal social interactions.