Fig. 15.1
This 33-year-old woman with stage III breast cancer had an excellent response to preoperative chemotherapy, and desired breast conservation. To minimize the potential for a poor cosmetic result with a defect in the upper pole, she underwent a right wire-guided lumpectomy (100 g) with simultaneous bilateral breast reduction (total masses 250 g left and 150 g right). The nipple was moved on the basis of an inferiorly based dermatoglandular pedicle. The pedicle filled the defect and her result is shown at 1 year following completion of radiation therapy for the right breast
15.4 Contraindications
The inferior oncoplastic pedicle technique typically cannot be used if the tumor defect is in the midline lower pole. If the tumor defect is slightly off midline and the inferior pedicle can be based more laterally or medially, then it can still be used for lower-pole tumors. Adequate base width is required and the pedicle cannot be detrimental to shaping the breast mound following resection. If it becomes difficult, then a more superiorly based pedicle is preferable. Central or subareolar tumors that require tumor resection directly beneath the nipple–areola complex could compromise nipple viability with a long inferior pedicle. Choosing a shorter pedicle or even amputation and free nipple graft is safer. Women with a previous infra-areolar biopsy scar or a tumor just inferior to the nipple are not candidates for the inferior pedicle procedure. Appropriate patient selection as always will minimize complications in patients with comorbidities and smokers.
15.5 Timing of Partial Breast Reconstruction
In general, partial breast reconstruction when indicated is best performed at the time of resection (immediate reconstruction). The main concern with immediate reconstruction is the potential for positive margins. When this concern does exist, the reconstruction can be delayed until final confirmation of negative margins (delayed–immediate reconstruction). This then allows the benefits of reconstruction prior to radiation therapy with the luxury of clear margins, although at the expense of a second procedure (Fig. 15.2). Such women at increased risk of positive margins included those under 40 years old, those with extensive ductal carcinoma in situ, those with high-grade tumors, those with a history of neoadjuvant chemotherapy, those with infiltrating lobular carcinoma, and those with human epidermal growth factor receptor 2/neu positivity [3, 7, 8]. The main disadvantage is the need for a secondary procedure, which might be unnecessary in most cases. When a flap reconstruction is required, we prefer to confirm the final margin status prior to partial breast reconstruction.
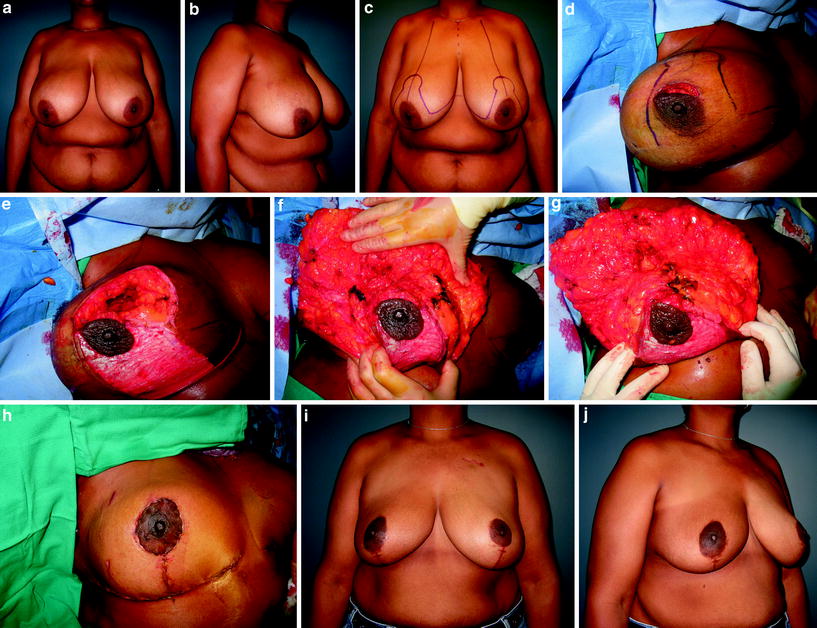
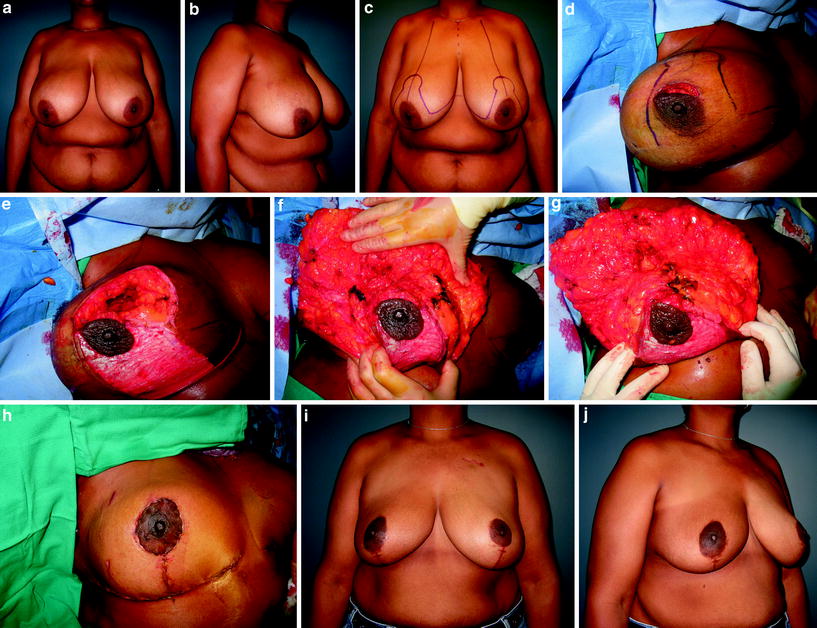
Fig. 15.2
This 49-year-old woman with macromastia had a resection above the nipple–areola complex. Her defect was reconstructed using an inferior pedicle breast reduction. Since there is little tissue on the pedicle above the nipple–areola complex to fill the dead space, the glandular tissue is plicated above the nipple for upper-pole volume. She is shown 1 year following completion of radiation therapy [11]
There are situations where poor results are encountered years following radiation therapy, which then require correction (delayed reconstruction). Reduction techniques should be used with caution in patients who have already been irradiated.
15.6 Surgical Technique
15.6.1 Preoperative Planning
The multidisciplinary team discusses the case and reviews the mammograms. The resective surgeon plans the tumor removal with or without radiographic guidance. The standard Wise pattern markings are then drawn preoperatively marking the nipple in the breast meridian about 19–23 cm from the sternal notch. The tumor defect location is anticipated and an inferior pedicle is drawn out. It should be about 8 cm wide in small breasts, and 10 cm or more in patients with large breasts. The location of the inferior pedicle can be adjusted either medially or laterally to maximize width and blood flow depending on the tumor location and degree of breast ptosis. A similar pattern is drawn on the contralateral breast for symmetry.
15.6.2 Resection
The breast surgeon then performs the tumor resection, ideally below or through the Wise pattern markings and not through the base of the inferior pedicle. If this approach is required for tumor resection, then an alternative pedicle design is required. Skin can be resected along with the tumor if desired as long as it is within the proposed area of dermatoglandular resection. It is important for the reconstructive surgeon to be present at the resection until a comfortable working relationship is achieved. Following tumor resection and intraoperative margin assessment, the cavity is clipped for postoperative surveillance and radiation boosting. The tumor specimen is weighed.
15.6.3 Reconstruction
The remaining breast tissue is examined. The goals are to [1] keep the nipple alive, [2] fill the dead space, and [3




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








